Acute Bacterial Conjunctivitis
Acute bacterial conjunctivitis is common and usually self-limiting, but high-risk groups must be screened for serious causes such as gonococcus and trachoma.
Introduction
Acute conjunctivitis can be:
- Bacterial
- Viral
- Allergic
- Irritative/Chemical
While often diagnosed clinically, distinguishing mild bacterial conjunctivitis from viral or allergic types can be difficult. Empiric treatment is typically initiated.
Always consider serious causes in at-risk groups, including:
- Hypopyon
- Gonococcal conjunctivitis
- Trachoma
- Herpetic infection
Epidemiology
- Common worldwide, especially in children under 5 years
- Gonococcal outbreaks reported in northern and central Australia
- Trachoma remains a major issue in Aboriginal communities
- Human-to-human transmission via contact with infected conjunctival or respiratory secretions
- Neonatal transmission can occur during vaginal delivery
Pathology
Common Bacterial Pathogens
| Common | Less Common / High-Risk |
|---|---|
| Haemophilus influenzae | Pseudomonas aeruginosa |
| Streptococcus pneumoniae | Staphylococcus aureus |
| Neisseria gonorrhoeae | |
| Neisseria meningitidis | |
| Chlamydia trachomatis (trachoma) |
- Incubation:
- Bacterial: 24–72 hours
- Trachoma: 5–12 days
- Reservoir: Humans
- Transmission: Direct contact, respiratory droplets, flies (trachoma)
- Infectious Period: While discharge is present
- Susceptibility: Universal; maternal immunity not protective
Clinical Assessment
Serious Causes to Consider
- High-Risk Groups
- Aboriginal populations (trachoma)
- Look for follicles, diffuse inflammation, or trichiasis
- Neonates
- Increased risk of gonococcal, meningococcal, and staphylococcal infections
- Aboriginal populations (trachoma)
- Hypopyon
- Must be actively excluded
- Foreign Body
- Exclude predisposing irritants
- Herpetic Infection
- Requires slit lamp exam
- Look for dendritic ulcer or nasociliary involvement (zoster)
Typical Presentation of Bacterial Conjunctivitis
- Ocular discomfort or “grittiness”
- Photophobia
- Conjunctival inflammation
- Purulent discharge
- Starts unilateral → becomes bilateral via cross-contamination
- 64% resolve spontaneously in 5 days (may last up to 14 if untreated)
Investigations
| When to Investigate | What to Order |
|---|---|
| Severe or high-risk cases (gonococcus, trachoma, neonates) | Swab for culture & PCR |
| Herpetic infection suspected | Slit lamp exam |
Management
- Irrigation
- Sterile saline to remove discharge
- Avoid Eye Padding
- Analgesia
- Oral analgesics as needed
- Anti-Irritant Drops
- Phenylephrine 0.12% for symptomatic relief
- Antibiotics
- Quinolones, gentamicin, and tobramycin are available but not first-line for uncomplicated cases.
- Neisseria spp. → require systemic antibiotics and specialist input
- Trachoma → systemic azithromycin or erythromycin (per guidelines)
| Drug | Dosing |
|---|---|
| Chloramphenicol | Drops 0.5%: 1–2 drops 2-hourly, then reduce to 6-hourly as improved |
| Ointment 1%: Use at bedtime | |
| Framycetin | Drops 0.5%: 1–2 drops 1–2 hourly, then reduce to 8-hourly as improved |
- Avoid:
- Topical steroids
- Topical anaesthetics
- Referral Criteria
- No improvement with treatment
- Visual impairment
- Suspected herpes, gonococcus, chlamydia
- All neonates → refer to paediatrics
Appendix 1
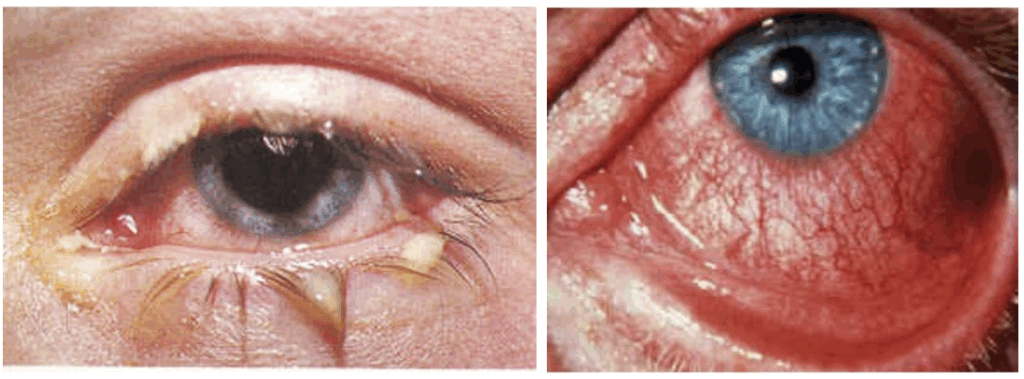
Right: Viral conjunctivitis
Appendix 2

Middle: Herpes Zoster Ophthalmicus with nasociliary nerve involvement.
Right: Flourescein stained cornea demonstrating a dendritic ulcer.
References
FOAMed
- Nickson C. Ophthalmology Befuddler. Clinical Cases. LITFL
- Nickson C. A Gritty Sticky Red Eye. LITFL
Publications
- Roper-Hall MJ. Thermal and chemical burns. Trans Ophthalmol Soc U K (1962). 1965;85:631-53.
- Dua HS, King AJ, Joseph A. A new classification of ocular surface burns. Br J Ophthalmol. 2001 Nov;85(11):1379-83.
- The Eye Emergency Manual, NSW Department of Health, 3rd ed. 2023
Fellowship Notes
Ba(Hons) Sheffield University, MBBS Newcastle University, MRCEM. UK Emergency Medicine doctor working in Australia |Stronger Medicine|
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |


