Corneal foreign bodies
Corneal foreign bodies are common ED presentations. Most can be removed safely under topical anaesthesia, but high-velocity injuries require exclusion of penetrating trauma.
Introduction
- Corneal foreign body is a common ED presentation.
- Most can be removed under local anaesthesia using a sterile needle or dental burr.
- Always consider the mechanism of injury — high-velocity trauma may cause penetrating injury.
Pathology
- Any material can lodge in the cornea.
- Most common ED presentation: high-velocity metal fragment.
- Grinder injuries rarely penetrate.
- Hammer-on-metal or high-speed drill injuries → higher risk of penetrating injury and intraocular foreign body.
Clinical Assessment
History
- Intense eye pain, watering, and foreign body sensation
- Symptoms may also occur with a subtarsal FB (under eyelid)
- Mechanism of injury: important for velocity and penetration risk
Examination
- Check visual acuity
- Inspection
- FB often visible; use slit lamp if not obvious
- Assess cornea, anterior chamber, iris, pupil, and lens for signs of penetration
- Evert the upper lid — look for subtarsal FBs
- Establish site of FB
- Central cornea (within 3 mm of pupil): scarring risk → consider ophthalmology referral
- If no FB found:
- Consider abrasion/ulcer (use fluorescein + cobalt blue light)
Investigations
- If penetrating injury suspected → plain radiographs or CT to detect intraocular FB
Management
- Topical anaesthetic (e.g. oxybuprocaine, amethocaine)
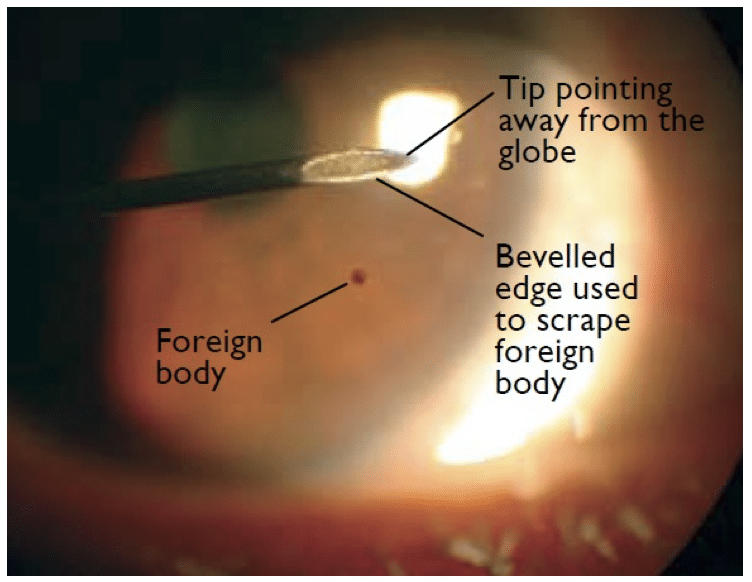
- Removal technique:
- Use 19–30G needle on 2–3 mL syringe
- Approach obliquely, bevel edge to scrape FB away from globe
- Remove associated rust rings with:
- Sterile needle
- Dental burr
- Algebrush device
- Subtarsal FBs → remove with cotton bud
- Eye pad optional:
- May improve comfort for 1–2 hours only
- Topical antibiotics:
- Drops 4x daily for 3–4 days
- Ointment at night if needed
- Contact lenses:
- Stop wearing until healed + 1 week
Disposition
- GP review in 48 hours
- Ophthalmology referral if:
- All FBs cannot be removed
- Central corneal involvement
- Suspicion of penetration
Appendix 1
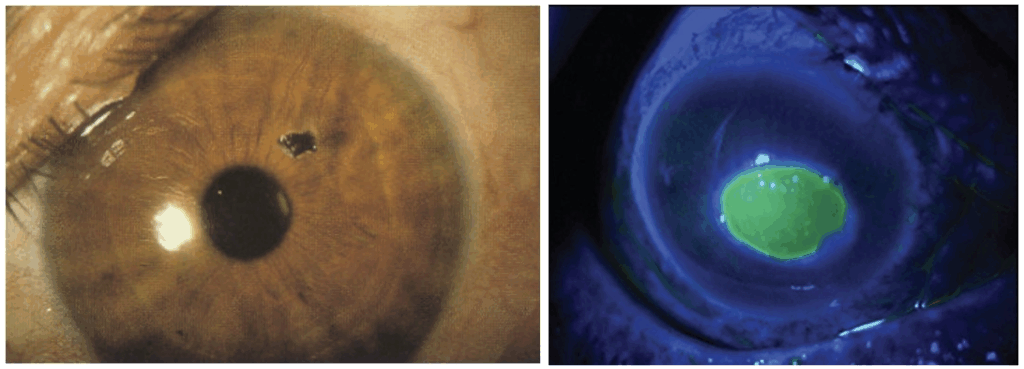
Right Central corneal ulcer seen with fluorescein staining under cobalt blue light
Appendix 2
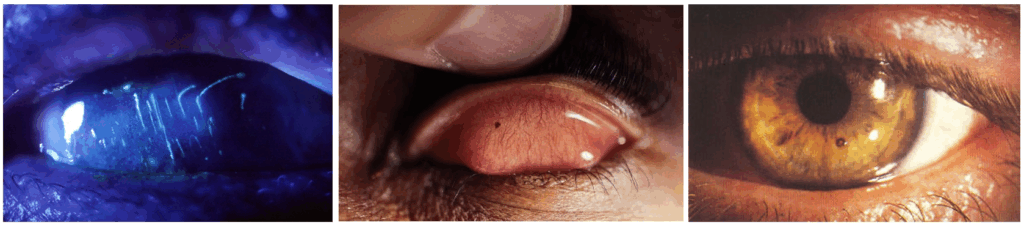
Middle: a small metal fragment subtarsal FB.
Right: Rust ring
References
FOAMed
- Nickson C. Ophthalmology Befuddler. Clinical Cases. LITFL
Publications
- The Eye Emergency Manual, NSW Department of Health, 3rd ed. 2023
Fellowship Notes
Ba(Hons) Sheffield University, MBBS Newcastle University, MRCEM. UK Emergency Medicine doctor working in Australia |Stronger Medicine|
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |


