Dacryocystitis
Dacryocystitis is an infection of the nasolacrimal sac and duct. It is typically caused by obstruction of the lacrimal drainage system, leading to stasis and secondary infection.
Anatomy
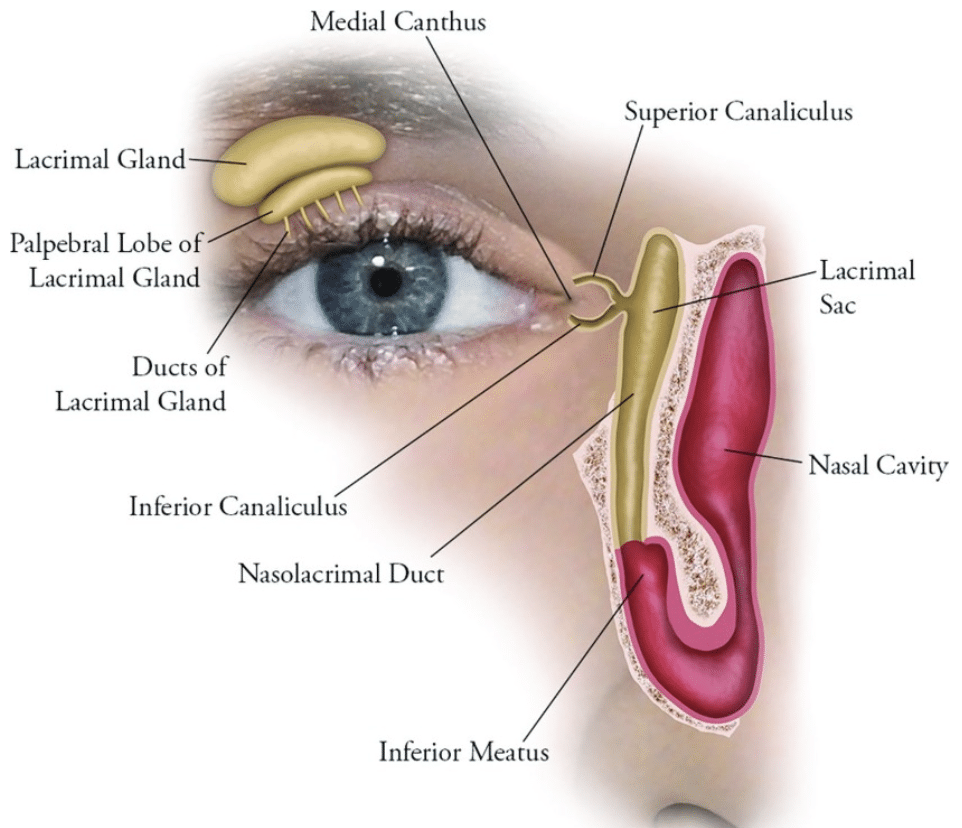
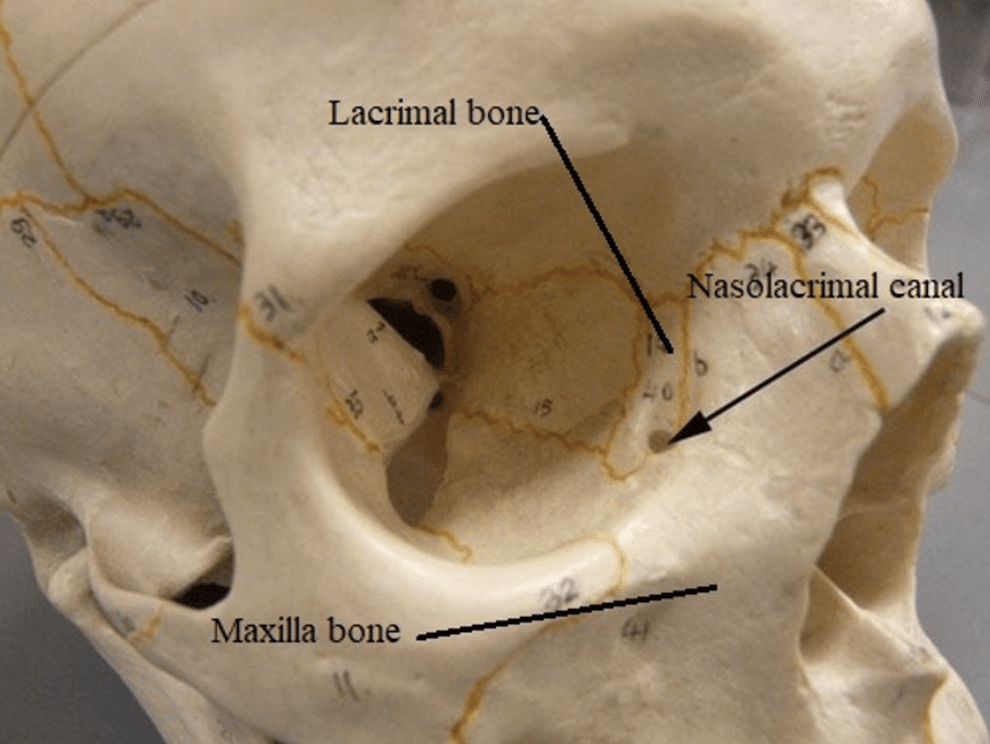
The Lacrimal Apparatus
| Component | Description |
|---|---|
| Lacrimal gland | Has two parts: a larger orbital part and a smaller palpebral part; both lie around the levator palpebrae superioris muscle and posterior to the orbital septum. |
| Ducts | ~12 ducts open into the lateral superior fornix of the conjunctiva. |
| Tear drainage | Tears flow across the cornea to the lacus lacrimalis, enter the lacrimal puncta, then drain via the lacrimal canaliculi to the lacrimal sac, and through the nasolacrimal duct into the inferior nasal meatus. |
| Lacrimal fold | A mucosal fold at the distal duct opening prevents air from entering during nose blowing. |
| Nerve supply | Parasympathetic secretomotor fibres are via the lacrimal nerve (from the maxillary branch of CN V). |
Pathology
Common organisms:
| Organism | Notes |
|---|---|
| Staphylococcus aureus | Most common |
| Streptococcus pneumoniae | Common |
| Streptococcus pyogenes | May cause rapid progression |
| Haemophilus influenzae | Especially in children |
| Pseudomonas aeruginosa | Consider in chronic/recurrent infections |
Causes:
| Group | Cause |
|---|---|
| Neonates/Children | Congenital nasolacrimal duct obstruction (up to 20% of newborns; 90% resolve by 6 months) Craniofacial abnormalities (may cause more severe infections e.g. orbital cellulitis) |
| Adults | Chronic allergic rhinitis Chronic sinusitis Facial trauma Faciomaxillary tumours |
Clinical Assessment
Dacryocystitis may present in acute or chronic forms.
Symptoms and Signs
- Inflammation over lacrimal sac/duct
- Swelling
- Redness
- Tenderness
- Warmth
- Epiphora
- Excessive tearing
- Purulent discharge
- Expressed from punctum on pressure
- Eyelash matting/crusting
- Abscess formation

Complications
| Complication | Description |
|---|---|
| Conjunctivitis | Local spread of infection |
| Fistula formation | Rupture through skin with drainage |
| Periorbital/orbital cellulitis | Serious local extension |
| Spreading facial cellulitis | May obscure the diagnosis of dacryocystitis |
| Meningitis | Rare but serious |
Investigations
| Test | Purpose |
|---|---|
| Swab for M/C/S | Culture purulent discharge when possible |
| CT scan | Identifies abscesses, soft tissue inflammation, and bony involvement |
| Dacryocystography (DCG) | Contrast study to assess duct patency; may be done with fluoroscopy, CT, or MRI |
Management
| Intervention | Notes |
|---|---|
| Analgesia | Paracetamol, aspirin, NSAIDs, opioids if severe |
| Warm compresses | Aid drainage of pus |
| Antibiotics | Oral: flucloxacillin or clindamycin for 7–10 days IV: vancomycin + third-gen cephalosporin if febrile/unwell |
| Crigler massage | Downward massage of lacrimal sac 2–3 times/day (especially in infants) |
| Surgery | Drain abscesses if present Dacryocystorhinostomy (DCR) for chronic or recurrent cases (can be done endoscopically to avoid scarring) |
Disposition
- Refer all suspected cases to Ophthalmology.
- Urgent referral if signs of orbital cellulitis or other serious complications.
Appendix 1
Appendix 2
Appendix 3

References
FOAMed
- Bell DJ. Dacryocystography. Radiopaedia
Publications
- The Eye Emergency Manual, NSW Department of Health, 3rd ed. 2023
Fellowship Notes
Ba(Hons) Sheffield University, MBBS Newcastle University, MRCEM. UK Emergency Medicine doctor working in Australia |Stronger Medicine|
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |


