SimCase 001
A 51 year-old-man is brought in by ambulance in acute respiratory distress. He is febrile and has a GCS of 13. His respiratory rate is 40 and SpO2 is 82% on 15L non-rebreather mask. The prehospital team have managed to gain vascular access with two large bore cannulae.
The nurses are placing an NIV mask and warming up the Hamilton-T1.

Questions
Which ventilator mode and strategy do you use?
| Mode/card | NIV-ST |
| Strategy | Protective/oxygenation |
How do you titrate PEEP?
Start at 10 – titrate as per PEEP/FiO2 scale; aim SpO2 >95%
How do you titrate FiO2?
Start at 50; titrate as per PEEP/FiO2 scale; aim SpO2 >95%
How do you titrate ΔPsupport?
Start at 10 and ensure TV> 520ml (>6ml/kg). If he was to remain on NIV then assess RR in 15 mins; if >25, increase TV to 8ml/kg and then reassess in another 15 going to a max of 10ml/kg
| Mode/card | NIV-ST |
| Strategy | Protective/oxygenation |
| Titrate PEEP | Start at 10 – titrate as per PEEP/FiO2 scale; aim SpO2 >95% |
| Titrate FiO2 | Starts at 50; titrate as per PEEP/FiO2 scale; aim SpO2 >95% |
| Titrate ΔPsupport | Start at 10 and ensure TV> 520ml (>6ml/kg). If he was to remain on NIV then assess RR in 15 mins; if >25, increase TV to 8ml/kg and then reassess in another 15 going to a max of 10ml/kg |
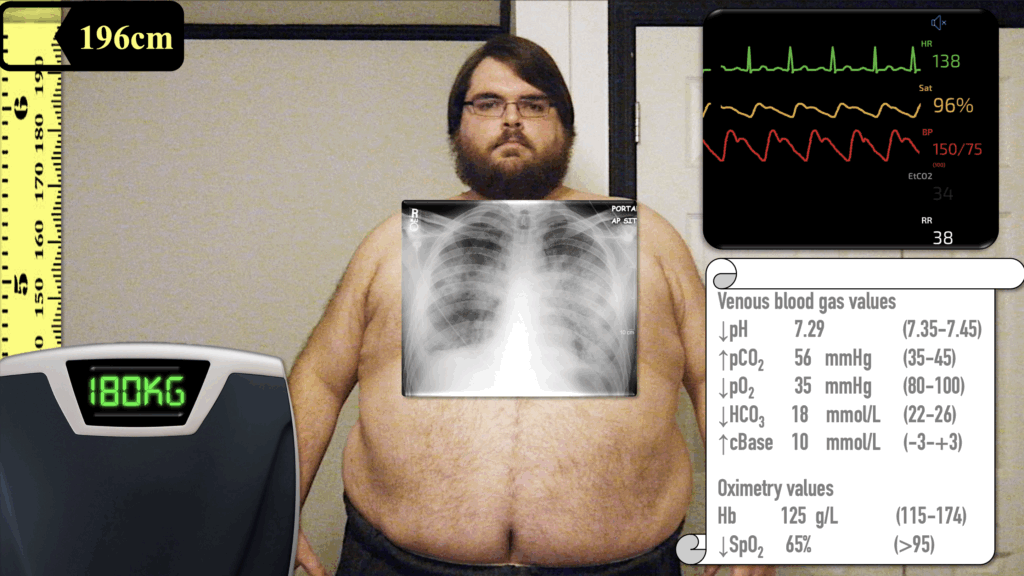
After 30 minutes, a CXR and venous blood gas (VBG) are performed
Questions
Interpret the CXR and ABG
CXR: bilateral pneumonia
VBG: This gas shows a patient who is severely hypoxic with a mixed acidosis: predominantly respiratory (high CO₂) but also a metabolic component (low HCO₃⁻ and base excess)
- pH 7.29 (low): Acidaemia.
- pCO₂ 56 mmHg (high): Respiratory acidosis.
- HCO₃⁻ 18 mmol/L (low) + Base excess –10: Metabolic acidosis component
Bilateral pneumonia and VBG shows he’s tiring -> patient needs intubation
How would you preoxygenate this patient in preparation for intubation?
VAPOX: Ventilator-assisted preoxygenation – ramping pillow should be inserted and positioning checked so that ear is above sternal notch and face parallel to ceiling
- PEEP = 20 as likely OSA
- FiO2 = 100%
- Rate = 6 so that it’s obvious when Ketamine kicks in
- Ketamine 0.5 mg/kg IBW; so likely 50mg over 90s (avoid bolus as will be become trsansiently apnoeic, and if OSA with obstruct)
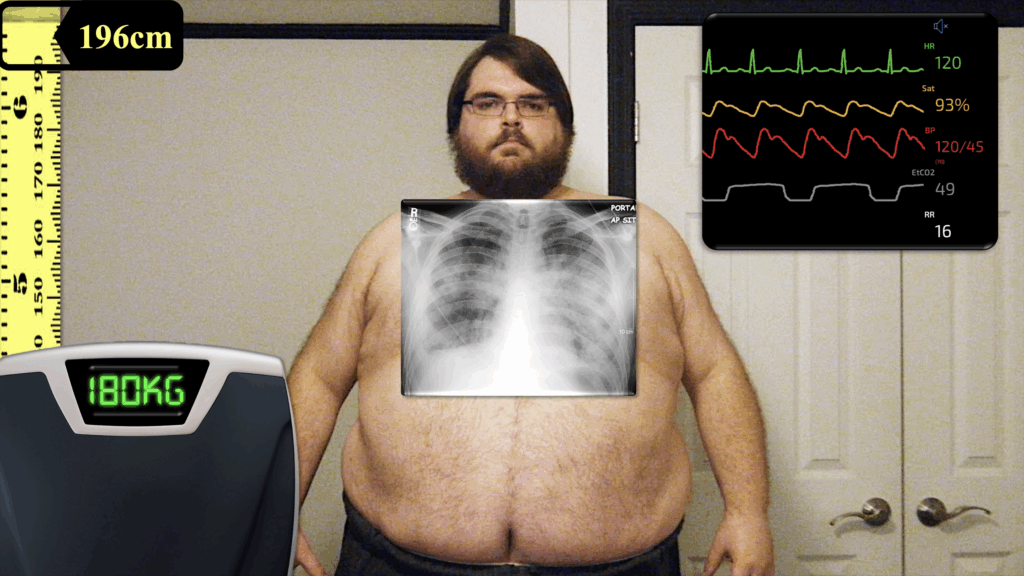
The patient has been successfully intubated
Questions
Which ventilator mode and strategy do you use?
| Mode | SIMV+ |
| Strategy | Protective. Input MALE and 196cm (T1 says IBW=90kg and TV =540ml) |
How do you titrate patient’s respiratory rate?
- RR = 16
- Titrate later depending on gases
How do you titrate patient’s PEEP and FiO2?
- Start at initial NIV settings
- Use PEEP/FiO2 scale aiming for SpO2 >95%
The VT alarm sounds…
How do you troubleshoot this?
- Press Alarms
- Increase upper limit of Pressure (max 70) while trouble shooting to allow TV
- If still going off, touch Graphics then Dynamic lung – make diagnosis of restrictive lung disease
Now that the patient is stablised…switch to ASV so they see what it does
- 110% MinVol
- PEEP 10
- FiO2 50%
- Gives RR 20 and TV 420mL
Use the card to show how the ‘safety window’ can be used diagnostically
- Tall rectangle = obstructive lung
- Long rectangle = restrictive lung
The small square of the mixed lung disease is the T1 threading the small needle of a COPD with pneumonia, balancing the degree of obstruction/restriction
Facilitator Notes
Facilitator notes for running Simulation
Facilitator Notes (for running the sim):
Once stabilised, switch to ASV: set 110% MinVol, PEEP 10, FiO₂ 50%. Show how the ASV safety window changes shape with restrictive vs obstructive patterns.
SimMon: manually set RR to 40 at start
At 30 min, show bilateral pneumonia on CXR, VBG with fatigue → force decision to intubate
After intubation, drop compliance to trigger pressure-limitation alarms → guide learners to raise alarm limits, then use Dynamic Lung to identify restrictive physiology
Further Reading
- Own the Hamilton with video overview
- Hamilton Guideline Cards (Adult/Paediatric) [PDF download]
- Hamilton Guideline Cards (Paediatric/Neonates) [PDF download]
- Simulation Case 001
- Simulation Case 002
References
- Senthi A. VAPOX Protocol. EDguidelines
- Grant S, Khan F, Keijzers G, Shirran M, Marneros L. Ventilator-assisted preoxygenation: Protocol for combining non-invasive ventilation and apnoeic oxygenation using a portable ventilator. Emerg Med Australas. 2016 Feb;28(1):67-72.
Emergency physician FACEM, Melbourne Australia

