SimCase 002
A 72 year-old-man is brought to the emergency department by ambulance with acute respiratory distress. He is a chronic smoker with no documented past medical history and has never been admitted to hospital.
On arrival he is on 15L O2 via non-rebreather mask (NRB), has a GCS of 13 and is speaking 2-3 words per breath. The prehospital team have gained vascular access with two wide bore cannulas in.
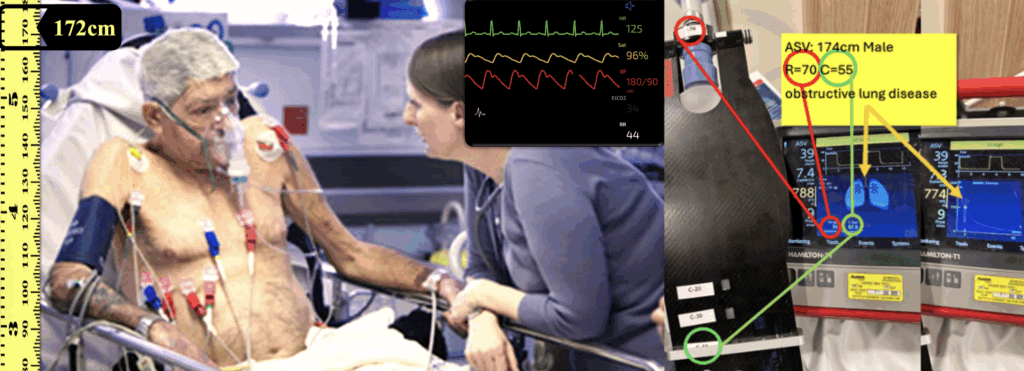
The nurses are placing an NIV mask and warming up the Hamilton-T1.
Questions
Which ventilator mode and strategy do you use?
| Mode/card | NIV-ST |
| Strategy | Obstructive |
How do you titrate PEEP?
- Start at 5
How do you titrate FiO2?
- Default is 50 – Aim for SpO2 86-92%
How do you titrate ΔPsupport?
- Start at 10 and ensure TV>6ml/kg (>410ml).
- If after 15 min RR is >25, increase to TV >8ml/kg (>547ml)
- If after another 15 min RR is >25, increase to TV >10ml/kg (>685ml)
- Check gas in an hour
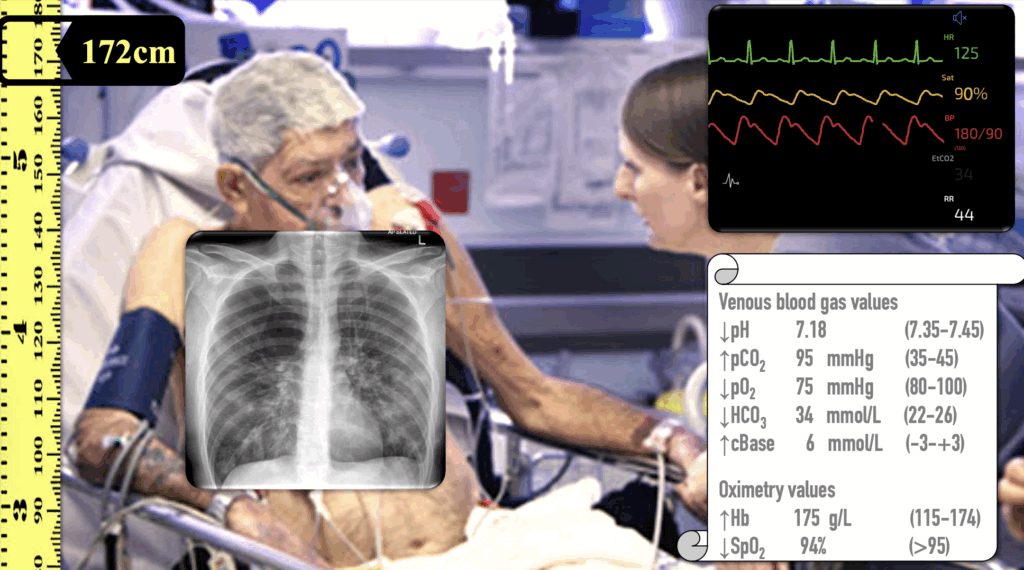
After 30 minutes, a CXR and venous blood gas (VBG) are performed
Questions
Interpret the CXR and ABG
CXR: COPD
VBG:
- pH 7.18 (low): Significant acidaemia.
- pCO₂ 95 mmHg (very high): Severe respiratory acidosis (marked CO₂ retention).
- HCO₃⁻ 34 mmol/L (high) + Base excess +6: Renal metabolic compensation is present.
- Hb 175 g/L (high): Suggests secondary polycythaemia, consistent with chronic hypoxia.
- Interpretation: Acute on chronic respiratory acidosis (e.g. COPD exacerbation) with severe CO₂ retention with partial metabolic compensation.
Acute on chronic respiratory acidosis – severe acidaemia = tiring
You decide to intubate, what’s you preoxygenation strategy?
VAPOX: Ventilator-assisted preoxygenation
- PEEP = 5
- FiO2 = 100%
- Rate = 6 so that it’s obvious when Ketamine kicks in
- Ketamine 0.5 mg/kg IBW; so likely 50mg over 90s
The patient has been successfully intubated
Questions
Which ventilator mode and strategy do you use?
| Mode | SIMV+ |
| Strategy | Obstructive Input MALE & 172cm (T1 IBW= 68kg with 6ml/kg TV = 410ml) |
How do you titrate patient’s respiratory rate?
- RR = 10
- Titrate later depending on gases ensuring that no gas trapping on flow curve
How do you titrate patient’s PEEP and FiO2?
- Leave PEEP at 5
- Titrate SpO2 to 86-92%
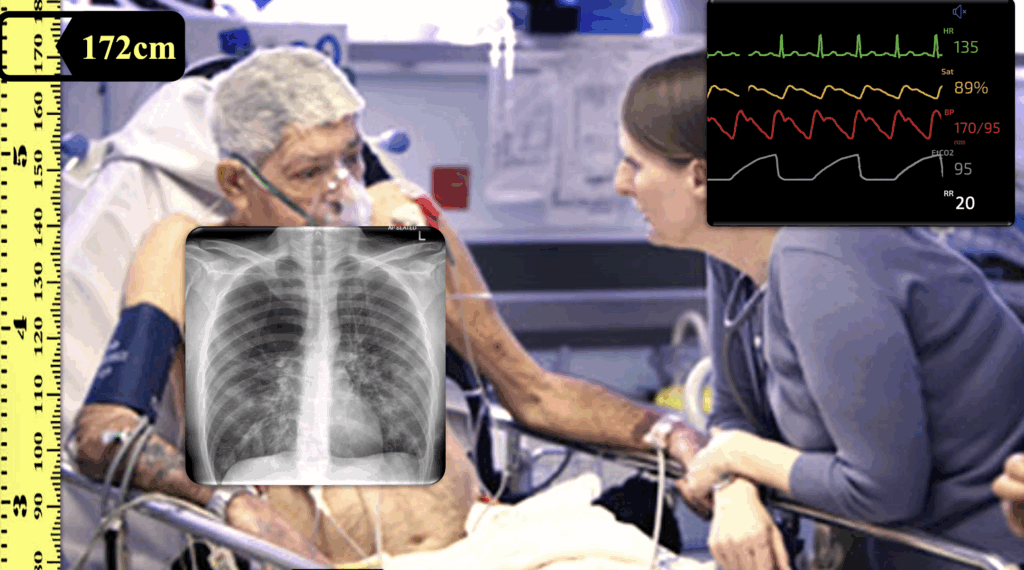
Sim-Mon: shark-fin on waveform ETCO2
T1: not returning to baseline (gas-trapping) on flow-curves
T1: High-pressure low-volume alarms
How do you troubleshoot this?
- Press Alarms
- Increase upper limit of Pressure (max 70) while trouble shooting to allow TV
- If still going off, touch Graphics then Dynamic lung – make diagnosis of OBSTRUCTIVE lung disease
Note: if we didn’t change, gas trapping would get to the point that we would be have MIXED LUNG DISEASE (box on right; high resistance and high compliance) which would manifest itself as dropping BP and we would need to disconnect patient & manually decompress chest.
As it is we need to decrease the rate – use the flow curve to show them how to get to the optimal rate. Ensure your I:E is >1:4
Now that the patient is stablised…switch to ASV so they see what it does
- 90% MinVol
- PEEP 5
- FiO2 titrate to SpO2 to 86-92%
- Gives RR 9 and TV 682mL
Use the card to show how the ‘safety window’ can be used diagnostically
- Tall rectangle = obstructive lung
- Long rectangle = restrictive lung
The small square of the mixed lung disease is the T1 threading the small needle of a COPD with pneumonia, balancing the degree of obstruction/restriction
The T1 uses significantly larger volumes than our manual strategy but that’s because our manual strategy of 6ml/kg is an oversimplification. You want your plan B to be different from your plan A
Facilitator Notes
Facilitator notes for running Simulation
SimMon: Show shark-fin ETCO₂ waveform.
T1: Demonstrate flow curves not returning to baseline (gas trapping).
Trigger high pressure/low Vt alarms → guide learners to:
- Press Alarms, temporarily increase pressure limit (max 70).
- Use Graphics → Dynamic Lung → identify obstructive pattern.
Make the point: if untreated, gas trapping → mixed lung disease with hypotension → disconnect and decompress chest.
Once stable, switch to ASV:
- %MinVol: 90%
- PEEP: 5
- FiO₂: titrate to SpO₂ 86–92%
- Learners should observe T1 chooses larger Vt and lower RR than their manual settings.
Further Reading
- Own the Hamilton with video overview
- Hamilton Guideline Cards (Adult/Paediatric) [PDF download]
- Hamilton Guideline Cards (Paediatric/Neonates) [PDF download]
- Simulation Case 001
- Simulation Case 002
References
- Senthi A. VAPOX Protocol. EDguidelines
- Grant S, Khan F, Keijzers G, Shirran M, Marneros L. Ventilator-assisted preoxygenation: Protocol for combining non-invasive ventilation and apnoeic oxygenation using a portable ventilator. Emerg Med Australas. 2016 Feb;28(1):67-72.
Emergency physician FACEM, Melbourne Australia


I find it interesting that the decision was made to intubate based on the blood gas results. I see many advanced COPD pts with pCO2 > 100 and pH as low as 7.05 that do just fine on NIV-ST with careful titration of pressure support, bronchodilators, and steroids. It is usually a mental status deterioration or non-reassuring TV to suggest tiring out which will make the decision easier.