5-step COVID: A cognitive aid for the pandemic airway
Editorial note: This is a guest post by Dr Peter Brindley (@docpgb), Dr Jarrod Mosier (@jarrodmosier), and Dr Chris Hicks (@humanfact0rz). The information provided is consistent with the current Safe Airway Society COVID-19 Consensus Statement – Airway Management and Tracheal Intubation.
– Dr Chris Nickson
Introduction
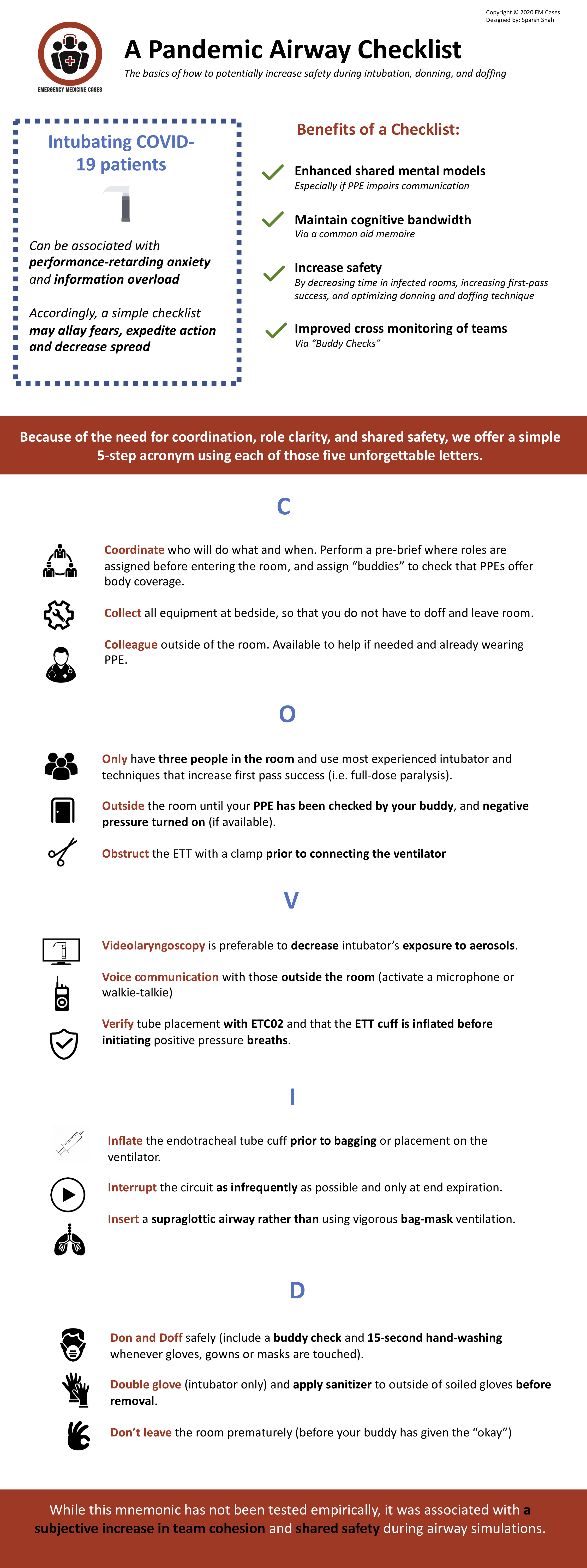
Viruses such as the SARS-CoV-2, which causes covid-19, can be associated with performance-retarding anxiety and information-overload; especially for those performing stressful procedures like intubation, and especially if there are unfamiliar steps. We offer this simple airway-management mnemonic/checklist/cognitive-aid that utilizes the five letters: C.O.V.I.D. Our goal is to allay fears, expedite action, decrease viral spread, and highlight what has changed. This aide-memoire can also be used for future highly infectious aerosol generating viruses, or whenever enhanced PPE is required. After all, we need to protect our staff, as well as patients, now and always; and other infectious pandemics are predicted.
An easy to remember cognitive aid may help because it can enhance shared mental models (especially if personal protective equipment (PPE) impairs communication), maintain cognitive bandwidth (via a common aide-memoire), increase safety (by decreasing time in infected rooms, increasing first-pass success, and optimizing donning and doffing technique) and make it routine to cross-monitor team members using ‘buddy checks’.
Even without COVID-19, airway management is more dangerous and complex when performed away from Operating Rooms, or if it includes unfamiliar staff (1). Cognitive aids with fewer than seven steps, and those that ask questions (i.e. “what will you do, and when”) appear to be superior to those that are long or passive (2). Moreover, checklists should facilitate safe teamwork not just individual taskwork (3).
In the case of highly infectious diseases such as COVID-19, safety requires undoing years of muscle memory (e.g. avoiding bagging, high flows, etc to prevent aerosolization). To date, much of the work on airway management has focused on the anatomical difficult airway, or the physiologically difficult airway (i.e. low blood pressure, right ventricular pathology) (4). While both are important, pandemics require increased attention to situational difficulty (personal fear, situational unfamiliarity) (1-5). Because of the increased need for coordination, role clarity, and shared safety, we offer a 5-step acronym using five unforgettable letters.
5-step COVID Cognitive Aid
Step 1: C
- Coordinate who will do what and when. Perform a pre-brief (3) where roles are assigned before entering the room, and assign “buddies” to check that PPEs offer body coverage.
- Collect all equipment at bedside, so that you do not have to doff and leave room.
- Colleague outside of the room. Available to help if needed and already wearing PPE.
Step 2: O
- Only have three people in the room and use most experienced intubator and techniques that increase first pass success (i.e. full-dose paralysis).
- Outside the room until your PPE has been checked by your buddy, and negative pressure turned on (if available).
- Obstruct the ETT with a clamp prior to connecting the ventilator
Step 3: V
- Videolaryngoscopy is preferable to decrease intubator’s exposure to aerosols.
- Voice communication with those outside the room (activate a microphone or walkie-talkie)
- Verify tube placement with ETC02 and that the ETT cuff is inflated before initiating positive pressure breaths.
Step 4: I
- Inflate the endotracheal tube cuff prior to bagging or placement on the ventilator.
- Interrupt the circuit as infrequently as possible and only at end expiration.
- Insert a supraglottic airway rather than using vigorous bag-mask ventilation.
Step 5: D
- Don and Doff safely (include a buddy check and 15-second hand-washing whenever gloves, gowns or masks are touched).
- Double glove (intubator only) and apply sanitizer to outside of soiled gloves before removal.
- Don’t leave the room prematurely i.e. before your buddy has given the “okay”.
In closing
While this mnemonic has not been tested empirically, it received iterative multi-professional input (MD, RN, RT) and multidisciplinary input (Critical Care, Emergency Medicine, Anesthesia). It was finessed during 10 drafts and over 20 iterative high fidelity mannikin simulations, and until no further changes were requested. It was deemed robust enough to serve throughout the hospital, and to benefit all members of the airway team. It was associated with an increased in subjective team cohesion and interdisciplinary esprit de corps. It was also associated with individual and shared safety: regardless of one’s specialty or role.
References
- Brindley PG, Beed M, Law JA, Hung O, Levitan R, Murphy MF, Duggan LV. Airway management outside the operating room: how to better prepare. Can J Anaesth. 2017. May;64(5):530-539.
- Gawande A. The Checklist Manifesto: How to Get Things Right. Metropolitan Books; 2009. [google books]
- Hicks C, Petrosniak A The Human Factor: Optimizing Trauma Team Performance in Dynamic Clinical Environments. Emerg Med Clin North Am. 2018 Feb;36(1):1-17.
- Brindley PG, Beed M, Duggan LV, Hung O, Murphy MF. Updating our approach to the difficult and failed airway: time to “stop and think”. Can J Anaesth 2016; 63(4): 373-81
- Mosier JM. Joshi R, Hypes C, Pacheco G, Valenzuela T, Sakles JC The physiologically difficult airway. West J Emerg Med. 2015 Dec; 16(7): 1109–1117.
Author’s affiliations
- Brindley PG, MD FRCPC; Department of Critical Care Medicine, Department of Anesthesiology and Pain Medicine, and the Dosseter Ethics Centre, University of Alberta, Edmonton, Canada
- Mosier JM, MD FCCM; Department of Emergency Medicine and Department of Medicine, Division of Pulmonary, Allergy, Critical Care and Sleep, University of Arizona College of Medicine, Tucson, AZ. USA
- Hicks CM, MD FRCPC; Department of Emergency Medicine, St Michael’s Hospital, University of Toronto, Ontario, Canada.
SARS-CoV-2
novel coronavirus of COVID-19
Brindley PG, MD FRCPC; Department of Critical Care Medicine, Department of Anesthesiology and Pain Medicine, and the Dosseter Ethics Centre, University of Alberta, Edmonton, Canada | @docpgb |

