Priapism
Priapism is a persistent, painful erection not related to sexual stimulation, lasting at least 2–4 hours. It is classified into:
- Non-ischaemic (high flow, arterial): Less common, usually self-limiting.
- Ischaemic (low flow, veno-occlusive): Most common, a urological emergency.
The duration of priapism is strongly associated with incidence of subsequent erectile dysfunction
Epidemiology
Priapism can occur in any age group, however, there is a bimodal peak distribution of incidence, occurring between 5 -10 years in children and 20 – 50 years in adults. Overall it is a rare condition, but is relatively more common in those with sickle cell disease
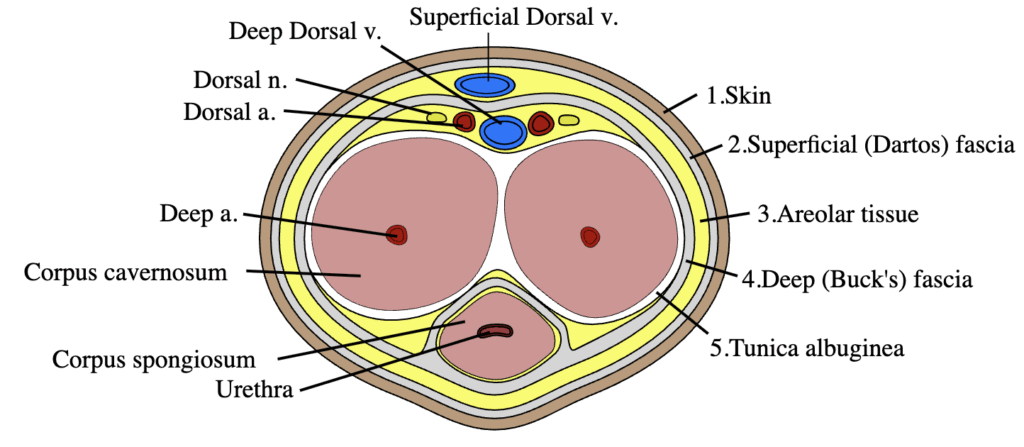
Anatomy
Pathophysiology
Erection results from increased arterial flow and reduced venous outflow. In ischaemic priapism, outflow fails, leading to hypoxia and acidosis. If untreated beyond 4–6 hours, tissue damage begins. Permanent dysfunction is likely if lasting >24 hours.
Priapism generally involves the corpora cavernosa only, although occasionally affects the corpus spongiosum and the glans penis
Nitric oxide (NO) is the major neurotransmitter controlling erection; the endothelium that lines the corpora cavernosa secretes NO. This occur in both normal and pathologic erections.
Causes
- Idiopathic (common)
- Medications: PDE5 inhibitors, intracavernosal injections, alpha-blockers, antipsychotics, cocaine
- Hematological: Sickle cell disease (esp. children), leukemia
- Neurologic: Spinal trauma
- Trauma: Pelvic/perineal
- Other: Infections, malignancy, venoms (e.g., redback spider)
Complications
Complications depend on the duration of symptoms, the patient’s age, and the underlying pathology. The time to treatment is the single most important factor affecting outcome. Ischaemia of the tissues generally begins to occur after 6 hours.
- Erectile dysfunction due to fibrosis
- Impotence
- Rarely ischemic gangrene
- Occasionally urinary retention.
Classification
- Ischaemic Priapism: Painful, rigid corpora, flaccid glans. Tue Urological Emergency.
- Non-Ischaemic Priapism: Less painful, partially rigid, often post-trauma. Not an emergency.
- Recurrent (Stuttering): Episodic, often in sickle cell disease. May lead to full ischaemic episodes.
Clinical Assessment
- Pain severity and duration
- Past medical history (e.g., sickle cell, medications)
- Physical: Tender, rigid corpora cavernosa; flaccid glans; check for trauma
Investigations
- FBE, reticulocyte count, hemoglobin electrophoresis (if hemoglobinopathy suspected)
- Cavernosal blood gas:
- Ischaemic: pH < 7.25, pO2 < 30, pCO2 > 60
- Non-ischaemic: Approximate arterial blood
- Urine drug screen
- Doppler ultrasound (if diagnosis unclear)
Management
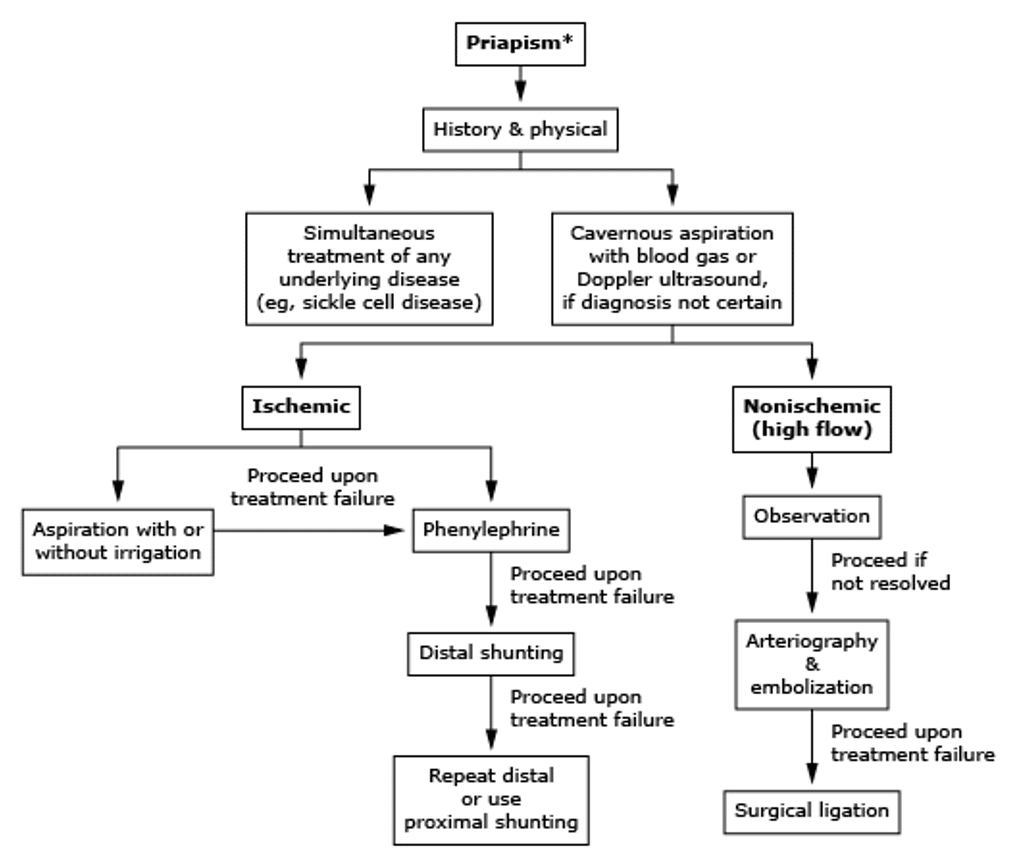
Ischaemic Priapism:
- Analgesia: IV or oral opioids
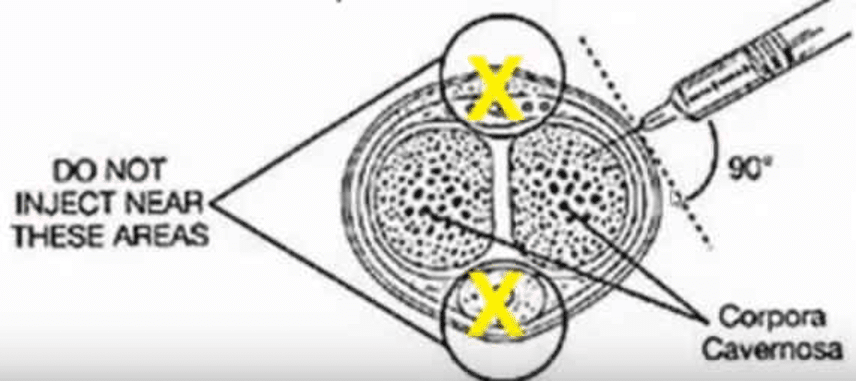
- Aspiration: From lateral corpus cavernosa (10 or 2 o’clock)
- Saline Irrigation: May improve resolution
- Alpha-agonists:
- Phenylephrine: 100–500 mcg/mL; 1 mL every 3–5 min up to 1 hour. pure alpha-adrenergic agonist, is considered the sympathomimetic of choice for ischaemic priapism as it has less risk of cardiovascular side effects compared to adrenaline
- Metaraminol: 0.5 mg every 5 min to 5 mg max
- Surgery: If above fails, shunt procedure
Non-Ischaemic Priapism:
- Observation: Often self-limiting
- Analgesia
- Embolization: For persistent cases
- Surgical ligation: If embolization fails
Disposition
- Ischaemic: Refer to Urology if unresponsive to aspiration and medication
- Non-ischaemic: Urology follow-up within a week if persistent
Algorithm for the treatment of priapism:
Cavernosal Blood Gas Interpretation
Note: Do not insert the needle near the dorsal midline (risk of damage to the neurovascular bundle) or near the ventral midline (risk of damage to the urethra)
| Type | pH | pO2 | pCO2 |
|---|---|---|---|
| Ischaemic Priapism | <7.25 | <30 | >60 |
| Non-Ischaemic Priapism | ~7.4 | >90 | <40 |
| Normal Venous Blood | 7.35 | 40 | 50 |
References
FOAMed
- Miers J, Mackenzie J. Procedure: Priapism management. LITFL
- Johnston M. A Most Discombobulating Gas. LITFL
Publications
- Lawton LD. Emergency department management of ischaemic priapism. Emerg Med Australas. 2021 Jun;33(3):555-558.
- Montague DK, Jarow J, Broderick GA, Dmochowski RR, Heaton JP, Lue TF, Nehra A, Sharlip ID; Members of the Erectile Dysfunction Guideline Update Panel; Americal Urological Association. American Urological Association guideline on the management of priapism. J Urol. 2003 Oct;170(4 Pt 1):1318-24.
- Salonia A, Eardley I, Giuliano F, Hatzichristou D, Moncada I, Vardi Y, Wespes E, Hatzimouratidis K; European Association of Urology. European Association of Urology guidelines on priapism. Eur Urol. 2014 Feb;65(2):480-9.
- Levey Bernie HR, Mulhall J. BMJ Best Practice: Priapism: (reviewed Mar 2021).
Fellowship Notes
Physician in training. German translator and lover of medical history.
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |

