A Most Discombobulating Gas
aka Metabolic Muddle 014
Imagine this – you are Captain at the Helm of an Emergency Departmental ship, critically ill patients floundering all over your very untidy deck, and you have a rudimentary knowledge of most of them. You have sorted out dispositions for most of the very unwell ones, and are awaiting intensive care beds to become available. You think that you have a modest handle on the teetering pathophysiology of those in your resus bay.
Just at that moment, a nurse hands you a blood gas on one of your patients. You glance at it, and your heuristic mind starts to spin; you jump up, piece of paper fluttering to the flight deck as you race around, seeking out the obviously near-terminal owner of the blood gas…
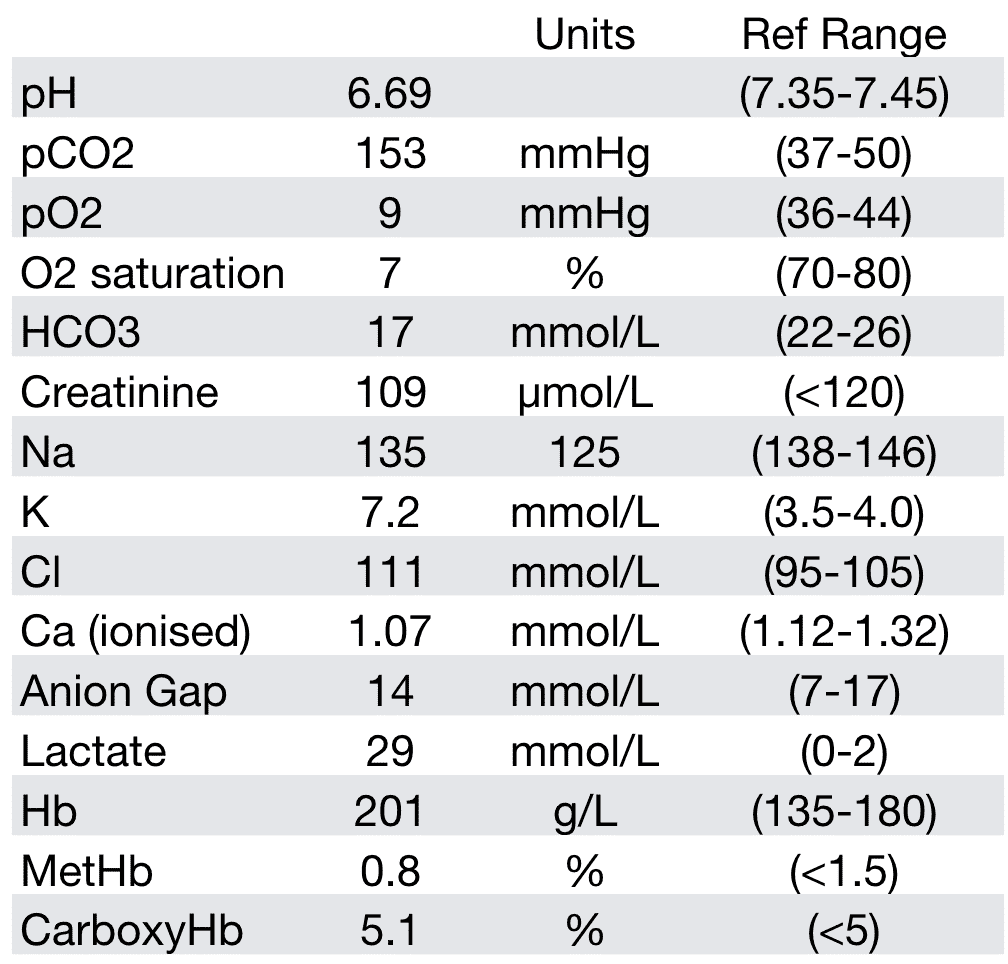
Here is the gas:
Questions
Q1. What is the lowest survivable pH in humans?
Answer
Try googling this one. At best, most sites will quote a pH of 6.8.
There is no acceptable answer. We probably all have anecdotal stories of apocryphal pHs – the post seizure patient, the ROSC after prolonged cardiac arrest, the toxicological conundrums. However there is no agreed lowest pH that is survivable.
Q2. In faithful Fellowship style, describe and interpret this gas.
Answer and interpretation
Description
- Gross acidaemia
- Respiratory and metabolic acidosis
- Anion gap = 7 – hey, what the…. With a lactic acid of 29!!!!
- Delta ratio = -0.71 – but! Difficult to interpret in setting of low-normal anion gap in first place
- Gross hyperkalememia, hypocalcemia
- Normal creatinine/sodium
- But damn! Look at that lactate!!
Interpretation
- WTF!
Q3. From where was this gas taken?
Answer and interpretation
This is a cavernosal gas.
You sigh with relief when you realize that the blood was aspirated from the corpus cavernosus of a patient with priapism.
Q4. What is the implication of this gas?
Answer and interpretation
gas is the clearest way of subdividing priapism into its two main subgroups:
- Ischaemic – pH < 7.25, pO2 60mmHg
- Non-ischaemic
Ischaemic priapism is exactly as defined – also described as a compartment syndrome of the penis, where there is failure of the veno-occlusive mechanism. It is also known as ‘low-flow’ priapism.
Causes
- idiopathic ~ 60%.
- The other 40% have a range of aetiologies that are generally vaso-occlusive (e.g. haematological disorders/malignancies) or mediated through alpha antagonism.
PHYSIOLOGY REMINDER:
The vascular response in the corpus cavernosum is complex and somewhat counterintuitive – although there is involvement of parasympathetics, nitric oxide ,VIP and prostaglandin E, detumescence is primarily controlled by adrenergic receptors. Catecholamines constrict smooth muscle, whilst the alpha2 (post-synaptic) receptors cause vasodilatation.
Thus – anything that opposes sympathetic flow, or blocks the adrenergic receptors risks preventing detumescence, and thus causing priapism:
- Systemic medications – antihypertensives, antidepressants, antipsychotics
- Intracorporeal injections
- Spinal injury – seen with other manifestations of neurogenic shock, again mediated through sympathetic blockade (although very uncommon to progress to ischaemic priapism)
- NO-mediated drugs, such as sildenafil (too much of a good thing!)
The implication of this gas is that irreversible corporeal damage occurs within 4-6 hours, thus requires emergency treatment.
Non-ischaemic priapism is the other major category of priapism. It is thought to be related to unregulated arterial inflow usually related to an arteriolar-sinusoidal fistula, often as result of trauma. Unlike ischaemic priapism, this tends to be non-painful
The third, uncommon, group in this classification is stuttering priapism.
Q5. Is there an alternative method for differentiating ischaemic from non-ischaemic priapism?
Answer and interpretation
Ultrasound
In the exponential world of ultrasound uses in the emergency department, colour flow doppler ultrasonography is also suggested for diagnostic purposes, looking for either absent or high flow.
Do any of our ultrasound gurus out there have any experience in this they may like to share?
Q6. How would you proceed to manage this patient?
Answer and interpretation
The aim of treatment is to evacuate anoxic blood, decompress the corpora cavernosa and achieve perfusion.
Most guidelines/articles/texts will take you through an escalating management algorithm for this, but bear in mind that you already have a corporal gas on this patient. You have already clinically suspected ischaemic priapism on history and examination, and have presumably anaesthetized the penis in order to aspirate blood.
However, we will briefly mention the conservative methods:
- Micturition, application of ice packs, gentle exercise, IV hydration and oxygen may have a role early on, but should not be relied upon. Oral sympathomimetics, although making intuitive sense, have little evidence for their efficacy.
Almost all of these patients will go onto requiring corporeal aspiration and injection.
- This is a simple procedure, and often delayed because of unnecessary discomfort (on behalf of the practitioner, not the patient).
- Penile anaesthesia is achieved easily by circumferential superficial infiltration at the base of the penis, or local infiltration at the site of needle placement.
- A 19 or 21G butterfly needle is then introduced next to the peno-scrotal junction at either the 3 or 9 o’clock positions to avoid hitting the neurovascular bundle. It is recommended to aspirate until fresh, red, oxygenated blood is aspirated, and detumescence (can be anywhere from 10ml to 100ml).
- The current recommendation for injecting alpha agonist is phenylephrine 200 micrograms, injected into the corpora once aspiration is finished, repeated every 5-10 minutes. If phenylephrine is not available, then metaraminol (1mg in 5ml of saline), or adrenaline (varying ranges throughout the literature – anywhere from 0.01-0.1mg, diluted from 1-5ml).
— Phenylephrine is preferred due to its much lower THEORETICAL risk of systemic cardiovascular effects.
— If one was to use metaraminol, or adrenaline, there is no documented frequency or risk of systemic effects, however it would be prudent to monitor the patient clinically, and reconsider its use in the patient with less than optimal coronary artery flow. - Recently intracavernosal injection of methylene blue has been advocated (with the curious adverse effects being penile burning and discolouration).
Here’s how they do it at Sinai:
Once detumescence has been achieved, it is recommended that all patients with ischaemic priapism be discussed with the Urology team.
The third-line treatment is surgical. If the above treatments fail, then surgical shunting is in order. Urology consultation is mandatory.
BUT – in true Life in the Fast Lane style, when we see a guideline, our spidey senses tingle. We are wary of dogmatic rules for decision making. Although internationally conceded guidelines all state that you need a gas to make a decision between high flow and low flow states of priapism, how often does a set of numbers REALLY make a difference? I talked to many a urological colleague of mine, whilst sculpting this post, and some of the more senior chaps (well my vintage, anyway) hadn’t seen a penile blood gas for many years. It was all a clinical decision. If the priapism was painful, had possible drug use/haematological precipitant as the aetiology, and required aspiration, it didn’t matter a squat what the PBG showed. If it resolved with aspiration, they just watch, if not, they went to theatre. Simple.
So, although the initial gas may be melodramatic, and an accepted part of a paper diagnostic algorithm, it is probably unlikely to be terribly helpful. Makes for impressive impact though.
References
Further Reading
Comprehensive video lecture from HQMEDED.com:
LITFL
Journal Articles
- Cherian J, Rao AR, Thwaini A, Kapasi F, Shergill IS, and Samman R. Medical and Surgical Management of Priapism. Postgrad Med J. 2006 February; 82(964): 89–94 PMC2596691
- Dean RC, Lue TF, Physiology of Penile Erection and Pathophysiology of Erectile Dysfunction . Urol Clin North Am. 2005 November; 32(4): 379–v. PMC1351051
- Tay YK, Spernat D, Rzetelski-West K, Appu S and Love C. Acute management of priapism in men. BJU Int. 2012 Apr;109 Suppl 3:15-21. PMID: 22458487.
- Traish A, Kim NN, Moreland RB, Goldstein I. Role of Alpha Adrenergic Receptors in Erectile Dysfunction Int J Impot Res. 2000 Mar;12 Suppl 1:S48-63. PMID: 10845765
- The Poison Review — Is that a jellyfish on your leg or are you just glad to see me? Priapism and Irukandji Syndrome
CLINICAL CASES
Metabolic Muddle
Emergency physician. Lives for teaching and loves clinical work, but with social media, she is like the syndromic cousin in the corner who gets brought out and patted on the head once in a while | Literary Medicine | @eleytherius | Website |