Barlow syndrome
Barlow syndrome (primary billowing mitral leaflet syndrome (BMLS)) is an often-used and more often misused diagnosis. It is a condition characterized by the displacement of an abnormally thickened mitral valve leaflet into the left atrium during systole with auscultatory findings of a late systolic murmur with non-ejection (‘mid-late’) systolic click
Most commonly described as type of degenerative mitral valve disease characterized by thickened and redundant leaflet tissue that causes the mitral valve to appear swollen. This condition leads to the valve closing unevenly and billowing into the left atrium during the heart’s contraction, similar to a parachute effect.
Clinical examination: distinctive auscultatory findings of a late systolic murmur with non-ejection (‘mid-late’) systolic click
Symptoms include chest pain (severe, sharp, frequent and localised), palpitations, anxiety, as well as electrocardiographic changes (resting S-T and T-wave changes), arrhythmias, conduction defects, systemic emboli and autonomic disorders
ECG changes: The most common pattern is T-wave inversion in leads II, III and AVF. Prominent upright U-waves were also seen to be quite common, especially in the right precordial leads. Patterns are not specific and require differentiation from the ECG manifestations of ischaemic heart disease and hypertrophic cardiomyopathy. Arrhythmias may be supraventricular or ventricular, benign or malignant, symptomatic or asymptomatic
A benign course is usual, requiring only reassurance. They equally emphasised that the condition may on occasion be complicated by systemic emboli, infective endocarditis, progression to severe mitral regurgitation and arrhythmias. Sudden death presumed to be secondary to cardiac arrhythmia has been reported.
Of note, more than 32 other conditions were noted by Barlow to cause or be associated with mitral valve billow (MVB) or a non-ejection click and/or mitral regurgitant systolic murmur
History of Barlow syndrome
1887 – Paul Cuffer and Barbillon describe ‘un bruit surnuméraire assez intense sourd, médio-systolique avec un bruit systolique’ [a fairly loud, muffled, supernumerary mid-systolic murmur with a systolic murmur]
1892 – American paediatrician Dr John Price Crozer Griffith (1856-1941) reported three cases in which the murmur of mitral regurgitation was heard after the apex beat and the first sound of the heart, instead of synchronously with and following them. This finding was reviewed and expanded on in 1903 by Josiah Newhall Hall (1859-1939) who concluded that the murmur was caused by regurgitation through a diseased mitral valve, and was later in time than the apex beat because of a tardy contraction of the left ventricle
However, the pervading opinion until the early 1960s was that these murmurs were “innocent” and caused by pleuro-pericardial adhesions or extracardiac disease
1961 – Dr John Reid suggested that mitral regurgitation was the cause of midsystolic murmurs and that the click probably arose from sudden tautening of previously lax chordae
…cases of mid-systolic clicks initiating a murmur ending at the second sound have been described in the literature and have been ascribed similarly to pleuro-pericardial adhesions. It is argued that a possible explanation of this mid-systolic click is a snapping taut of a chordae tendineae during the later high-pressure phase of ventricular systole which, when resulting in mitral incompetence, is followed by a murmur that continues, like the murmur of mitral incompetence, at least to the second sound. The term ‘chordal snap‘ is proposed for mid-systolic clicks in which this explanation is thought operative.
1963 – John Brereton Barlow (1924-2008) and colleagues used cine-ventriculography, to demonstrate conclusively apical late systolic murmurs as being the result of mitral regurgitation. They concluded that the associated “clicks are likely to arise from an intracardiac cause”. Barlow wrongly ascribed the findings to fibrosed chordae due to rheumatic valve disease and recommended that patients be placed on antibiotic therapy against rheumatic fever
The original paper was rejected by the principal scientific journals of the time on the grounds that it was “too extreme to claim that the cause was due to the mitral valve mechanism” instead being published by the Maryland State Medical Journal. This led to the American Heart Journal publishing “The significance of late systolic murmurs”, with the description of auscultatory findings in seven patients, later that year.
1966 – John Michael Criley (1931-) correctly interpreted the mechanism of regurgitation as excessive posterior leaflet motion into the atrium during systole, a phenomenon he termed mitral valve prolapse
…a unique anatomical type of mitral regurgitation, recognized cine-angiographically, which occurs in association with a murmur in the latter part of systole or marked accentuation of a soft holosystolic murmur in late systole. Correlations of the cine-angiograms with phonocardiograms have provided a functional anatomical basis for the late onset of the murmur as well as the systolic click which was present in 3 of the patients.
1968 – Barlow demonstrated that the click originated in the mitral valvular complex. It was the result of billowing of one of the mitral leaflets, which in turn was the consequence of uneven distribution of tension in the chordal mechanism.
Evidence has previously been produced from this laboratory that apical late systolic murmurs denote mitral regurgitation, and that the commonly associated non-ejection systolic clicks also have an intracardiac, and probably chordal, origin. It has also been suggested that the association of these auscultatory features with a distinctive electrocardiographic pattern and a billowing posterior leaflet of the mitral valve constitutes a specific syndrome.
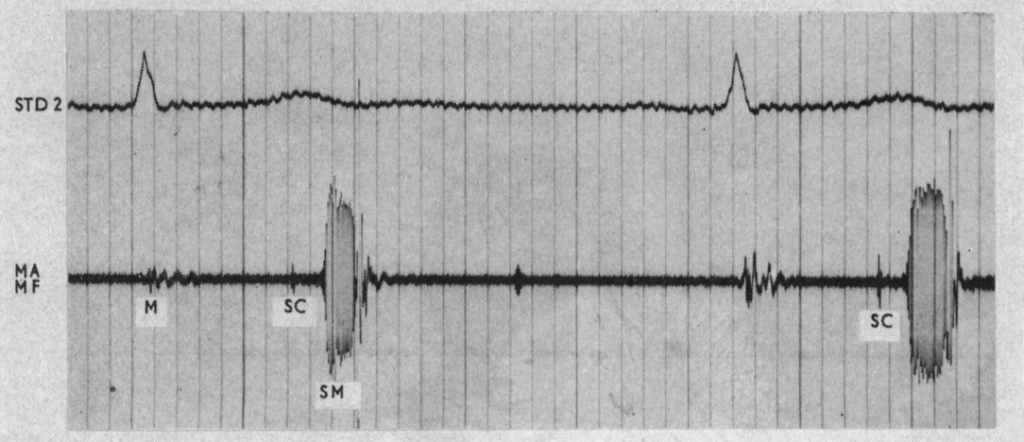
FIG. 2.-Phonocardiogram, recorded in mid-expiration, of a musical late systolic murmur in a 15-year-old girl. A non-ejection click is also present. Left ventricular cine-angiocardiography demonstrated mild mitral regurgitation and abnormal billowing of the posterior leaflet.
Abbreviations: MA=mitral area; MF=medium frequency; SM= systolic murmur; SC=systolic click; M=mitral component of first heart sound. The distance between the heavy vertical lines equals 0-20 sec. Barlow 1968
Barlow identified patients with specific auscultatory findings who displayed clinical abnormalities including ECG changes compatible with inferior myocardial ischaemia, and a variety of dysrhythmias. He also presented a case demonstrating pathologic correlation
A 39-year-old man with phonocardiographic confirmation of a late systolic murmur and non-ejection click, died suddenly while mowing a lawn: no cause of death was established at necropsy nor was any coronary artery abnormality detected. We later examined the mitral valve which had an extremely voluminous posterior leaflet and thin elongated chordae tendineae.
1980 – Alain Frédéric Carpentier and colleagues characterized the surgical lesions seen in Barlow syndrome. They were the first to differentiate BML from another category of mitral valve prolapse where there was no billowing or excess tissue.
1992 – Barlow had described a specific “auscultatory-electrocardiographic” syndrome characterized by a billowing leaflet, with protrusion of the leaflet body to the atrial side, above the annulus, without the significant regurgitation that characterizes prolapse. The differences can be clearly identified with the echocardiogram. Barlow very much disliked the term prolapse
…Criley et al. introduced in 1966 the term ‘prolapse’ of the mitral valve…We contend that attempts to asses so-called ‘mitral valve prolapse’ (MVP) based principally on variable echocardiographic criteria and with ongoing use of Criley’s terminology, are misleading and compound the present confusion… It is thus regrettable that the term is used even when the valve anomaly is mild, clinically silent, and functionally normal.
Variously called primary mitral valve prolapse (MVP), floppy valve, myxomatous leaflet, click-murmur, or Barlow syndrome, the term billowing mitral leaflet (BML) syndrome is preferred.
So-called ‘mitral valve prolapse’ ranges from an insignificant normal variant to an important and
potentially fatal cause of mitral valve disease. We must learn neither to overtreat the former nor to
be negligent in our neglect of the latter!
Associated Persons
- John Price Crozer Griffith (1856-1941)
- Josiah Newhall Hall (1859-1939)
- John (JVO) Reid (-2004)
- John Brereton Barlow (1924-2008)
- John Michael Criley (1931- )
- Alain Frédéric Carpentier (1933- )
Alternative names
- Mitral valve prolapse
- Billowing mitral leaflet syndrome (BMLS)
References
Historical references
- Cuffer P, Barbillion M. Nouvelles recherches sur le bruit de galop cardiaque. Archives générales de médecine 1887; 19: 129-149 and 301-319
- Crozer Griffith JP. Mid-systolic and late systolic mitral murmurs. The American Journal of the Medical Sciences 1892; 104(3): 285-294
- Hall JN. Late systolic mitral murmurs. Am J Med Sci 1903; 125: 663-666
- Reid JVO. Mid-systolic clicks. South African Medical Journal. 1961; 35(17): 353-355
- Humphries JO, McKusick VA. The differentiation of organic and “innocent” systolic murmurs. Prog Cardiovasc Dis 5:152-171, 1962
- Criley JM, Lewis KB, Humphries JO, Ross RS. Prolapse of the mitral valve: clinical and cine-angiocardiographic findings. Br Heart J. 1966 Jul;28(4):488-96
- Fontana ME, Sparks EA, Boudoulas H, Wooley CF. Mitral valve prolapse and the mitral valve prolapse syndrome. Curr Probl Cardiol. 1991 May;16(5):309-75.
- Carpentier A, Chauvaud S, Fabiani JN, Deloche A, Relland J, Lessana A, D’Allaines C, Blondeau P, Piwnica A, Dubost C. Reconstructive surgery of mitral valve incompetence: ten-year appraisal. J Thorac Cardiovasc Surg. 1980 Mar;79(3):338-48.
Eponymous term review
- Steinberg DL. Mid systolic click–late systolic murmur syndrome (Barlow’s syndrome): a review. J Med Assoc Ga. 1974 Mar;63(3):107-9.
- Anyanwu AC, Adams DH. Etiologic classification of degenerative mitral valve disease: Barlow’s disease and fibroelastic deficiency. Semin Thorac Cardiovasc Surg. 2007 Summer;19(2):90-6.
- Obel IW. Mitral valve billow and prolapse: a brief review at 45 years – with reference to : mitral valve billowing and prolapse : perspective at 25 years. Cardiovasc J Afr. 2009 Jan-Feb;20(1):24-6.
- Melnitchouk SI, Seeburger J, Kaeding AF, Misfeld M, Mohr FW, Borger MA. Barlow’s mitral valve disease: results of conventional and minimally invasive repair approaches. Ann Cardiothorac Surg. 2013 Nov;2(6):768-73.
- Mestres CA, Piñón MA, Quintana E. Commentary: The Barlow valve: Understanding disease and symmetry. JTCVS Tech. 2021 Oct 9;10:66-67.
eponymictionary
the names behind the name
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | On Call: Principles and Protocol 4e| Eponyms | Books |
