BRASH syndrome
BRASH syndrome is an acronym for Bradycardia, Renal Failure, AV blockade, Shock, and Hyperkalaemia.
BRASH syndrome is a synergistic process created by a combination of hyperkalaemia and medications blocking the atrioventricular (AV) node. The most common precipitants are hypovolaemia and medications promoting hyperkalaemia or renal injury.
BRASH syndrome is fundamentally a synergistic process created by a combination of hyperkalemia and medications blocking the AV node. As such, BRASH syndrome lies at the center of a continuumranging from isolated hyperkalemia to an isolated overdose of an AV nodal blocking medication (e.g., beta-blocker intoxication)
Farkas et al 2020
Understanding and recognising the pathophysiology of BRASH syndrome as a distinct entity may improve patient outcomes. Treatment includes fluid resuscitation; hyperkalaemia therapies including intravenous calcium, insulin/glucose, beta agonists, diuresis; and management of bradycardia
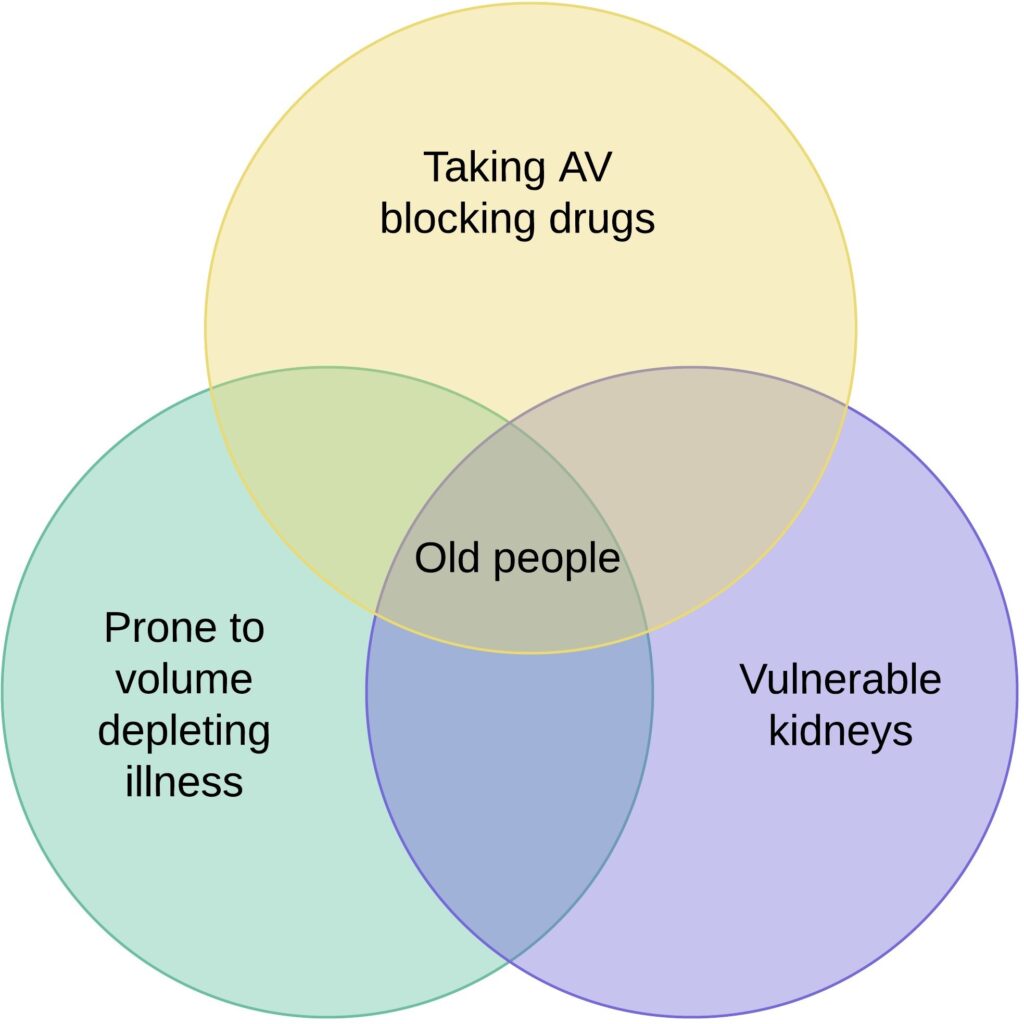
The population with the potential to develop BRASH syndrome is very large.
Pathophysiology
Hyperkalaemia and AV-nodal blocking medications (such as beta blockers, calcium channel blockers, digoxin, and amiodarone) can cause bradycardia. These two factors may function synergistically to produce more dramatic bradycardia than would be expected from either factor alone.
Most of our body systems are controlled by negative feedback loops, if something goes up we have mechanisms in place for it come down thereby maintaining homeostasis. BRASH syndrome is a confluence of events that lead to a positive feedback loop that if left untreated can result in death.
Bradycardia reduces the cardiac output; impairs renal perfusion; precipitates renal dysfunction; and exacerbates hyperkalaemia. Left unchecked, the vicious cycle of hyperkalaemia, bradycardia, renal dysfunction, and worsening hyperkalaemia may progress to multiorgan failure with shock, bradycardia, and renal failure – BRASH syndrome
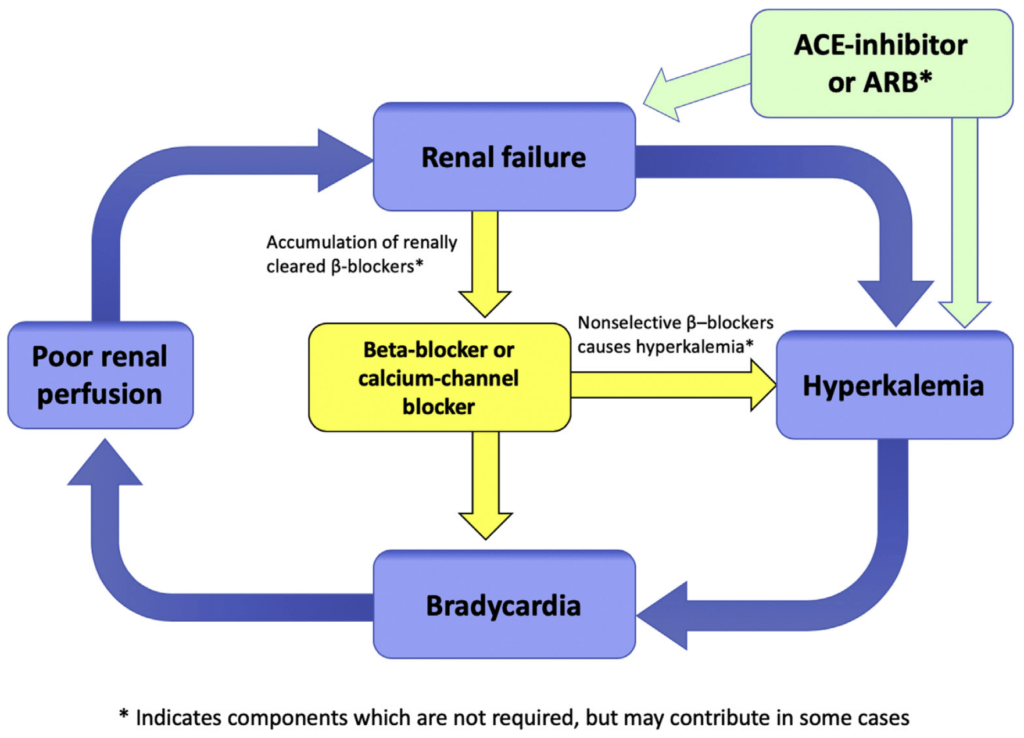
ACE = angiotensin-converting enzyme; ARB = angiotensin-receptor blocker.
BRASH (Bradycardia, Renal failure, AV blockade, Shock, and Hyperkalemia) pathophysiology.
Clinical presentation
Patients may present with a variety of symptoms ranging from asymptomatic bradycardia to multiorgan failure.
The most common presentation
Then become hypovolaemic for any reason such as a gastrointestinal illness. This hypovolaemia causes poor kidney perfusion, leading to an acute kidney injury that further prevents the normal excretion of AV blocking drug and potassium. The AV blocking drug then accumulates causing bradycardia and shock, leading to worsening kidney perfusion and the positive feedback loop is established.
Treatment
First, recognise the constellation of clinical findings and manage as a syndrome rather than treating the individual factors; understand that standard ACLS algorithms (without calcium..) may lead to unnecessary intervention with transvenous pacemakers; then break the cycle…
The most common error in managing BRASH syndrome is fixating on a single component of the syndrome (e.g., hyperkalemia) and focusing solely on management of that problem (e.g., emergent dialysis). Meanwhile, other aspects of the syndrome are overlooked (e.g., the patient might remain under-resuscitated, bradycardic, and malperfused)
Farkas et al 2020
Aim to treat hyperkalaemia, bradycardia, hypovolaemia (usually), and renal hypoperfusion,
Calcium: Management of moderate to sever hyperkalaemia; stabilizes the myocardium, which may drastically improve heart rate and cardiac output.
Fluid resuscitation: A patient with BRASH syndrome will usually be volume deplete, a good choice of fluid is ‘normal’ bicarb; made by adding 150mls of 8.4% Sodium Bicarbonate to 850mls of water for injection, giving 1L of isotonic fluid. [Note: some patients with BRASH syndrome may develop oliguric renal failure, fluid retention and volume overload. Assess fluid status on an individual basis]
Enhance potassium excretion: Diuresis with potassium-wasting diuretics such as frusemide or if anuric; dialysis.
Adrenaline: If calcium fails to resolve the bradycardia, adrenaline administration can increase heart rate and cardiac output and renal perfusion; and shift potassium intracellularly, improving hyperkalaemia. Isoprenaline is an alternative chronotropic agent and preferred over beta-agonists, such as dobutamine or dopamine.
The kidneys need to be perfused to excrete AV blocking drugs and potassium. If the patient is euvolaemic but still shocked then do not hesitate to start an inotrope such as adrenaline for its chronotropic and vasoconstricting properties. Don’t forget that these patients are usually on these drugs to treat their hypertension and will likely have a higher baseline blood pressure than the general population.
Consider:
- Other temporizing treatments for hyperkalaemia such as insulin/dextrose and salbutamol.
Clinical case
Ethel is 85 and is feeling generally unwell. She has not eaten or drunk much over the weekend and has had one vomit. Ethel’s background includes AF, hypertension, hypercholesterolaemia, macular degeneration and a TIA. Ethel’s medications include aspirin, metoprolol, Ramipril, and apixiban.
Ethel is unwell with an irregular HR at 44 BPM, BP 85/60, Temp 35.7, sats 94% RA. Her VBG and ECG on arrival:
References
Blogs and podcasts
- Farkas J. BRASH syndrome: Bradycardia, Renal failure, Av blocker, Shock, Hyperkalemia. Pulmcrit (Emcrit). 2016
- McLaren J. ECG Cases 10 – Hyperkalemia: The Great Imitator. Emergency Medicine Cases. 2020
- Helman A. 4-Step Approach to Bradycardia and Bradydysrhythmias. Emergency Medicine Cases. 2021
- McLaren J. ECG Cases 20 – Approach to Bradycardia and the BRADI Mnemonic. Emergency Medicine Cases. 2021
- Buttner R. Clinical case: ECG Case 120. LITFL
Journals
- Lee TH, Salomon DR, Rayment CM, Antman EM. Hypotension and sinus arrest with exercise-induced hyperkalemia and combined verapamil/propranolol therapy. Am J Med. 1986 Jun;80(6):1203-4
- Hegazi MO, Aldabie G, Al-Mutairi S, El Sayed A. Junctional bradycardia with verapamil in renal failure–care required even with mild hyperkalaemia. J Clin Pharm Ther. 2012 Dec;37(6):726-8.
- Farkas JD, Long B, Koyfman A, Menson K. BRASH Syndrome: Bradycardia, Renal Failure, AV Blockade, Shock, and Hyperkalemia. J Emerg Med. 2020 Aug;59(2):216-223.
Critical Care
Compendium
Dr Tom Cassidy MBBS FACEM. Emergency physician, Perth Australia. Father of two humans and whimsical lyricist. Special skills: relocating ECGs, reading toxidromes and interpreting dislocations | @tgpcassidy | LinkedIn |



That is a really great and helpful article and I love how the different components are pointed out in such a memorable way to improve specific treatment.
I just have one little comment regarding the following sentence:
“Isoprenaline is an alternative chronotropic agent and preferred over beta-agonists, such as dobutamine or dopamine.”
Pharmacologically, isoprenaline (isoproterenol) is a beta-agonist (beta1+2), and also a more selective one than dopamine which has a broader spectrum of receptors it is acting on compared to isoproterenol.