Carlos Chagas
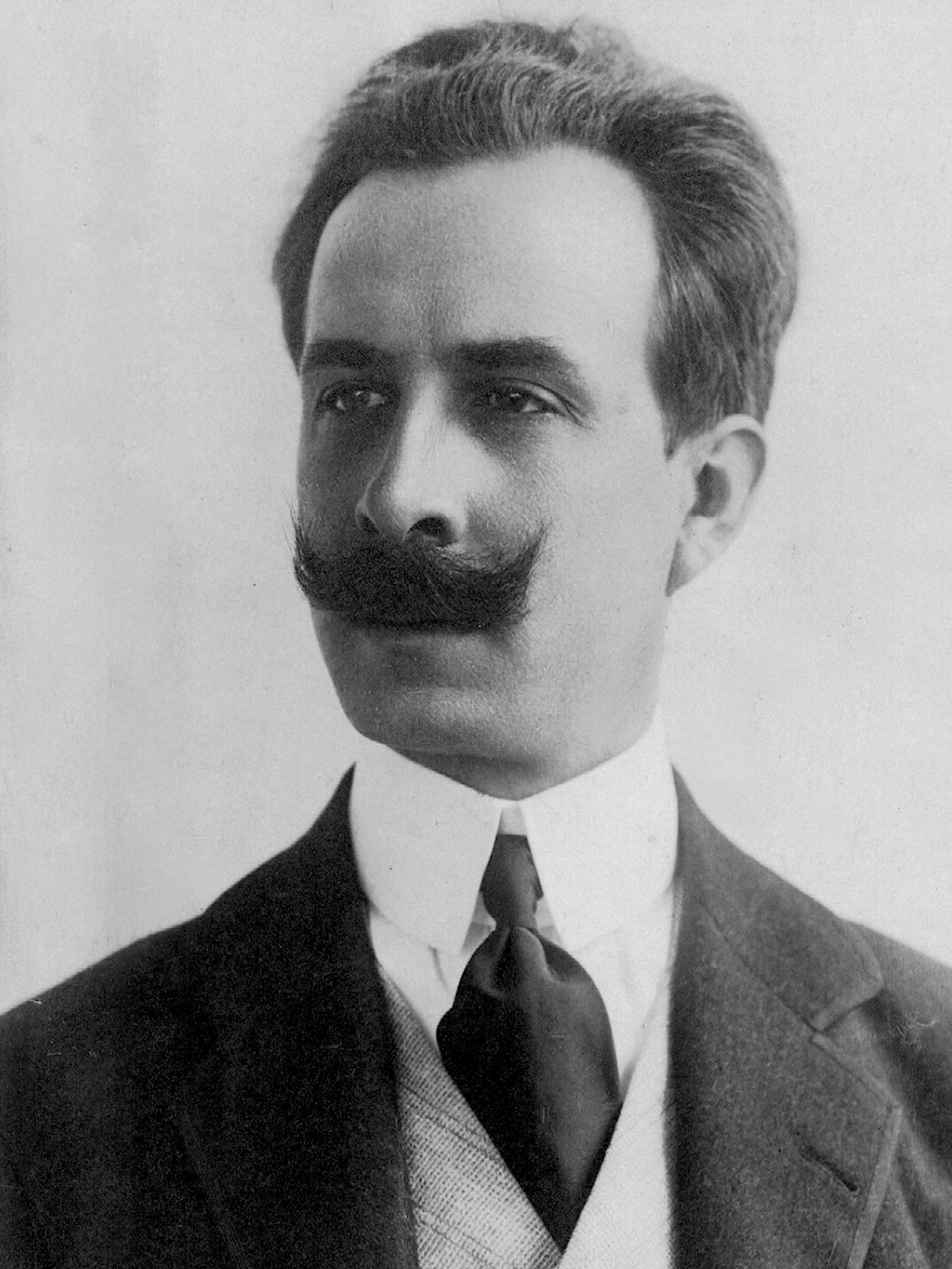
Carlos Justiniano Ribeiro das Chagas (1879–1934) was a Brazilian physician
Chagas helped define modern tropical medicine and public health in Brazil. Chagas combined laboratory parasitology with experience in rural disease control. He later directed the Oswaldo Cruz Institute and played a national leadership role in public health becoming a central figure in Brazil’s response to epidemic threats.
He is eponymously linked with Chagas disease. In 1908, while working at Lassance in Minas Gerais, Chagas identified a domestic triatomine bug (“barbeiro”), with a newly recognised protozoan parasite (Trypanosoma cruzi), and demonstrated human transmission. He documented the first recognised human case in a child and published internationally in Portuguese, German, and French
Biographical Timeline
- Born July 9, 1879 on a farm near Oliveira, Minas Gerais, Brazil.
- 1887 – Jesuit schooling (Itu, São Paulo)
- 1897 – Enters the Faculty/Medical School of Rio de Janeiro.
- 1902 – Began work at Manguinhos (Federal Serotherapeutic Institute) while preparing his medical thesis/dissertation; first close contact with Oswaldo Cruz and laboratory medicine.
- 1903 – Qualified as physician (Rio de Janeiro) and presented thesis on malaria haematology Estudos hematológicos no impaludismo.
- 1904 – Opens practice in central Rio. Serves as physician for the General Directorship of Public Health (DGSP) at Jurujuba Hospital, Niterói
- 1905 – Led malaria control campaign in Itatinga (São Paulo), Brazil’s first major successful anti-malarial campaign
- 1906 – Appointed Assistant, Instituto Oswaldo Cruz (IOC), Manguinhos.
- 1907–1908 – Coordinates malaria prophylaxis in Xerém; argues malaria transmission is largely intra-domiciliary, supporting insecticide-based control. Works along the Central Railway of Brazil; improvised lab in a train wagon at São Gonçalo das Tabocas (renamed Lassance in 1908).
- 1908 – Identifies trypanosomes in the intestines of Triatomine bugs (“barber bugs” or “kissing bugs”). He names the parasite Trypanosoma cruzi in homage to Oswaldo Cruz.
- 1909 (Apr 14) – First recognised human infection. Isolated T. cruzi in the blood of 2 year old girl Berenice Soares de Moura. Reported publicly at the National Academy of Medicine session (Oswaldo Cruz read Chagas’ work).
- 1910 – Admitted as full member of Brazil’s National Academy of Medicine (extraordinary position created).
- 1912 – Awarded the Schaudinn Prize (Hamburg) for protozoology/tropical medicine work.
- 1912–1913 – Leads expedition to the Amazon river valley to study regional sanitation conditions.
- 1913 – Nobel Prize first nomination.
- 1917 (Feb 14) – Appointed Director of the Instituto Oswaldo Cruz; holds post until 1934.
- 1918 – Organises Rio’s emergency hospitals and services to the Spanish influenza epidemic.
- 1920 – Director-General of DNSP. Order of the Crown of Italy
- 1921 – Second Nobel Prize nomination; receives Harvard honorary title
- 1922 – Member of the League of Nations Hygiene and Health Committee.
- 1923 – Helped expand public health training; associated with creation of the Anna Nery Nursing School. Commander of the Belgian Crown, Legion of Honour
- 1925 – Appointed Chair of Tropical Medicine at the Medical School of Rio de Janeiro. Hamburg’s Kümmel Prize (gold medal).
- 1925 – Participated in the Malaria Congress in Rome.
- 1926 – Implements IOC regimental reform, creating six scientific sections; further honours Order of Isabella the Catholic, and honorary doctorate at University of Paris
- Died suddenly on November 8, 1934 in Rio de Janeiro aged 55
Medical Eponyms
Chagas disease (American trypanosomiasis)
Synonyms: American trypanosomiasis; Trypanosoma cruzi infection
Causative organism: Trypanosoma cruzi (protozoan)
Classic vector: Triatomine (“kissing”) bugs (Triatominae)
Chagas disease (American trypanosomiasis) is a neglected tropical disease caused by the protozoan Trypanosoma cruzi. Contemporary estimates suggest ~6–8 million people are infected worldwide, with ~50,000 deaths/year, and ~65–100 million living at risk of infection.
Historically concentrated in Latin America, Chagas disease has increasingly become a concern in non-endemic regions because of population movement; in these settings, transmission is predominantly non-vectorial (e.g., blood transfusion, organ transplantation, and congenital transmission).
In endemic areas, triatomine bugs typically live in cracks of walls and roofs, feed at night (often on the face), and transmission occurs when infected bug faeces contaminate the bite site or mucous membranes.
The “barbeiro” (kissing bug) and a new parasite
1907 – While working in Lassance (Minas Gerais) on malaria control along the railway works, Chagas encounters a domestic triatomine bug (“barbeiro” or “kissing bug”) associated with poor rural housing and nocturnal biting.
1908 – Chagas identifies a haematophagous triatomine (Panstrongylus megistus) carrying a previously undescribed trypanosomatid. He later names it Trypanosoma cruzi honouring his mentor Oswaldo Cruz (1872-1917).
First human case (1909)
1909 – On April 14, 1909 Chagas diagnoses the first recognised human case A two year old girl, Berenice Soares de Moura, with parasites in peripheral blood
Berenice, zwei jährige. Sangue: Dia 14-4-09 — Tripanozómidas no sangue periférico…
He moved rapidly to alert international tropical medicine networks, publishing in Portuguese, German, and French outlets within the same year, then consolidating the lifecycle, morphology, and clinical entity in his longer Memórias do Instituto Oswaldo Cruz report with extensive illustrations.
Chagas illustrations (1909). Click to enlarge
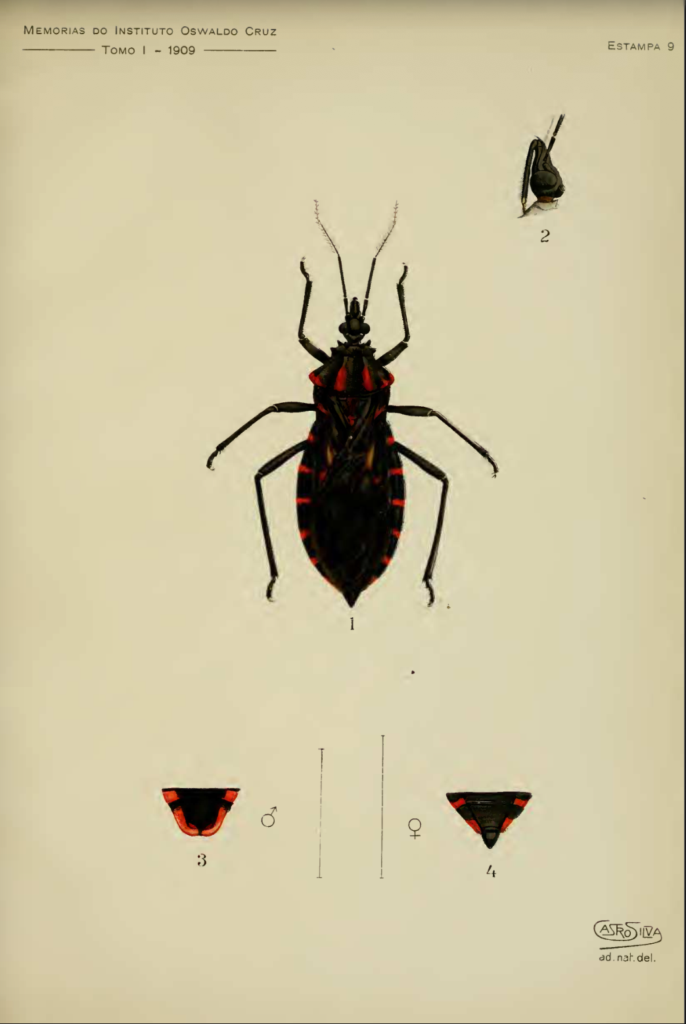
Estampa 9 – Triatomine “barbeiro” (kissing bug) vector of Trypanosoma cruzi; dorsal habitus with detail inset and sexually dimorphic terminal abdominal segments (♂/♀).
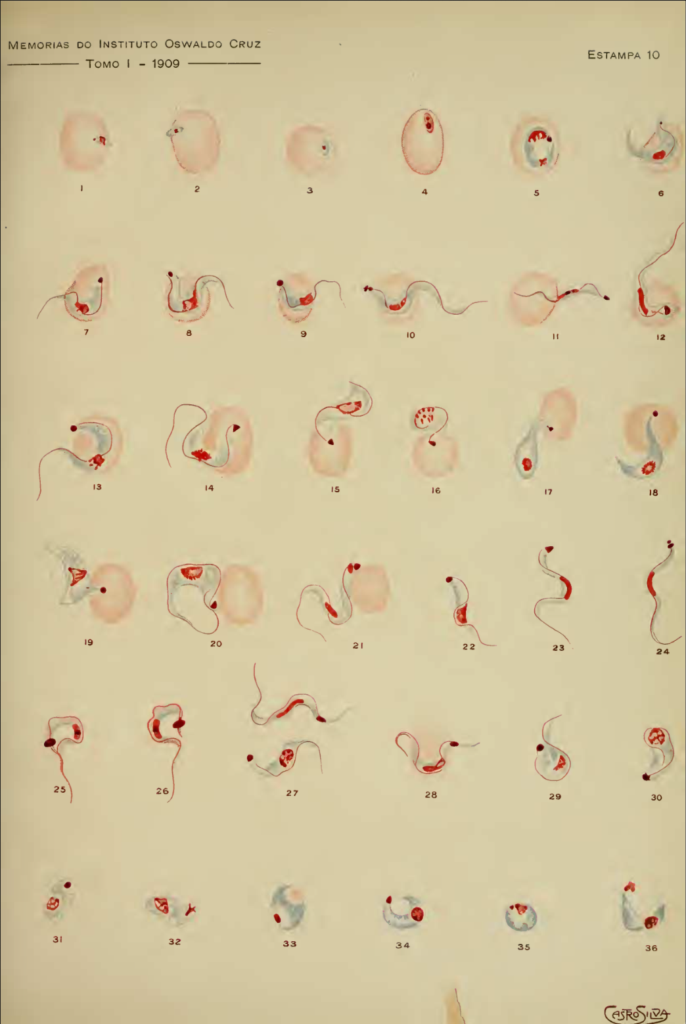
Estampa 10 – T. cruzi in peripheral blood: multiple examples of bloodstream forms showing variation in body curvature, nucleus/kinetoplast position, and free flagellum.
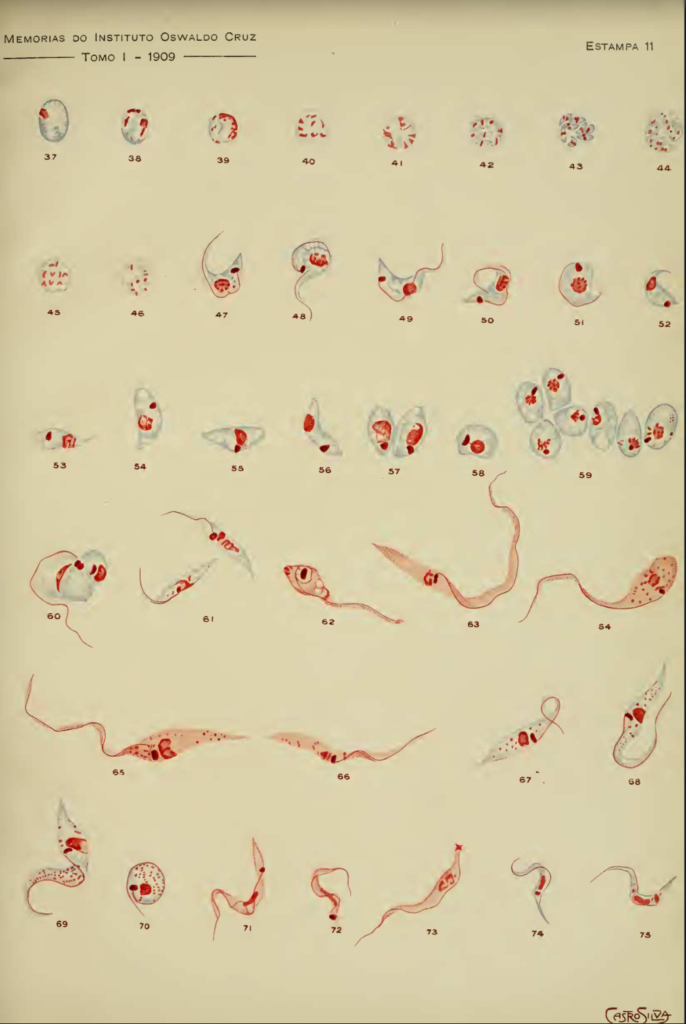
Estampa 11 – Developmental and dividing forms attributed by Chagas to the agent of “nova trypanosomiase humana,” illustrating morphological transitions and multiplication stages.
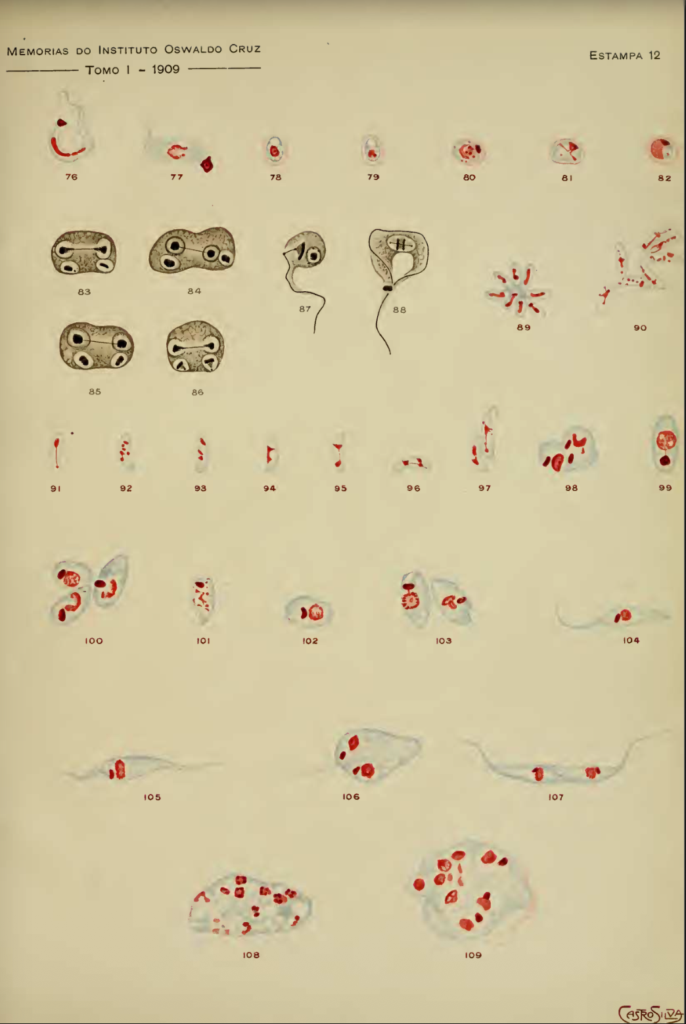
Estampa 12 – Schematic and stained preparations depicting intracellular groupings (“nests”) and additional developmental forms described in the account.
1935 – Cecilio Romana (1901-1997) described Romaña sign. Classic, early, and usually unilateral sign of acute Chagas disease, characterised by painless, often purplish swelling of the eyelids and surrounding tissues.
1960 – Governmental control programs begin in Latin America marking a shift from discovery to public health implementation).
1965-1972 – Nifurtimox (a nitrofuran) released by Bayer and Benznidazole (a nitroimidazole) released by Roche are introduced into Latin American
1991 – Southern Cone Initiative launched (Argentina, Bolivia, Brazil, Chile, Paraguay, Uruguay) targeting vector control and transfusion safety. This marked amajor turning point in incidence reduction.
1998 – World Health Assembly resolution commits to halting transmission by 2010
2019 (May) – 72nd World Health Assembly designates April 14 as World Chagas Disease Day.
2020 (April 14) – First global observance of World Chagas Disease Day framed as a chance to make visible a long-neglected disease, including its spread beyond Latin America via non-vector routes
Controversies
Not…The Nobel Prize
Chagas discovered a disease, its parasite, and its vector and yet the Nobel Prize never followed.
In reality there were four nominations over time, but only two (1913 and 1921) were officially registered at Karolinska
1913 nomination was made by Manoel Augusto Pirajá da Silva; the prize that year went instead to Charles Robwert Richet “in recognition of his work on anaphylaxis”
1920 nomination, by Manoel Augusto Hilário de Gouvêa of Rio de Janeiro. However, despite 42 nominations the 1921 Nobel Committee did not award the Medicine prize at all.
Major Publications
- Chagas C. Nova tripanozomiaze humana: estudos sobre a morfolojia e o ciclo evolutivo do Schizotrypanum cruzi n. gen, n sp, ajente etiolojico de nova entidade morbida do homem. Mem. Inst. Oswaldo Cruz 1909; 1: 159-218
- Chagas C. Nova especie morbida do homem, produzida por um trypanosoma (Trypanozoma cruzi). Nota prévia. Brazil-Médico. 1909; 23(16): 175.
- Chagas C. Neue Trypanosomen. Archiv für Schiffs- und Tropen-Hygiene. 1909; 13(4): 120-123
- Chagas C. Über eine neue Trypanosomiasis des Menschen. Archiv für Schiffs- und Tropen-Hygiene. 1909; 13(11): 351-353
- Chagas C. Nouvelle espéce de trypanosomiase humaine. Bulletin de la Société de Pathologie Exotique 1909; 2(6): 304-307
- Chagas C. Sobre as variações ciclicas do cariozoma em duas especies de ciliados parazitos: contribuição para o estudo do nucleo nos infuzorios. 1911
- Chagas C. Descoberta do Tripanozoma Cruzi e verificação da Tripanozomiase Americana: retrospecto historico. 1922
References
Biography
- Carlos Chagas. Memórias do Instituto Oswaldo Cruz 1934: 29
- Lewinsohn R. Prophet in his own country: Carlos Chagas and the Nobel Prize. Perspect Biol Med. 2003 Fall;46(4):532-49.
- Schapachnik E, Riera AR, Dubner S, Filho CF, Uchida AH, Ferreira C. Dr. Carlos Justiniano Ribeiro das Chagas (1879-1934): A giant of the Third World. Cardiol J. 2009;16(6):592-3.
Eponymous terms
- Romaña C. Acerca de un sintoma inicial de valor para el diagnóstico de la forma aguda de la enfermedad de Chagas. La conjuntivitis esquizotripanósica unilateral. (Hipótesis sobre la puerta de entrada conjuntival de la enfermedad). Mission de Estudios de Patologia Regional Argentina (MEPRA) 1935 22:16-28, 1935.
- Lewinsohn R. Carlos Chagas (1879-1934): the discovery of Trypanosoma cruzi and of American trypanosomiasis (foot-notes to the history of Chagas’s disease). Trans R Soc Trop Med Hyg. 1979;73(5):513-23
- Delaporte F. Romana’s Sign. Journal of the History of Biology 1997; 30(3): 357-366
- Jurberg C. Chagas: one hundred years later. Bull World Health Organ. 2009 Jul;87(7):491-2
- de Araujo-Jorge TC, Telleria J, Rios-Dalenz J. History of the Discovery of American Trypanosomiasis (Chagas Disease) In: American Trypanosomiasis, (ed. Telleira, Tibayrenc), 2010: 3-23
- Kropf SP, Sá MR. A descoberta do Trypanosoma cruzi e da doença de Chagas (1908-1909): medicina tropical no Brasil. Hist. cienc. saude-Manguinhos 2009; 16(suppl 1)
- Albajar-Viñas P, Dias JC. Advancing the treatment for Chagas’ disease. N Engl J Med. 2014 May 15;370(20):1942-3
- Lidani KCF, Andrade FA, Bavia L, Damasceno FS, Beltrame MH, Messias-Reason IJ and Sandri TL Chagas Disease: From Discovery to a Worldwide Health Problem. Front. Public Health 2019; 7: 166.
- Beucler N, Torrico F, Hibbert D. A tribute to Cecilio Romaña: Romaña’s sign in Chagas disease. PLoS Negl Trop Dis. 2020 Nov 12;14(11):e0008836.
- Patel V, Patel D, Patel G, K. Patel JK. Chagas Disease. Historical and Current Trends In: Rising Contagious Diseases: Basics, Management, and Treatments. 2024
Eponym
the person behind the name
MBBS, BMedSci (Hons) University of Nottingham.
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | On Call: Principles and Protocol 4e| Eponyms | Books |