Charles Miller Fisher
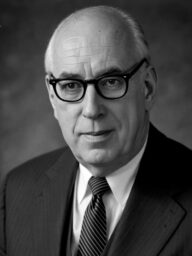
Charles Miller Fisher (1913-2012) was a Canadian neurologist.
C. Miller Fisher was one of the most influential figures in the clinical understanding and management of cerebrovascular disease.
Fisher’s pioneering work established many of the modern concepts underpinning stroke neurology. He was the first to describe transient ischaemic attacks (TIA) as stroke precursors (1952); elucidated the relationship between carotid artery stenosis and cerebral infarction; and demonstrated atrial fibrillation as a major source of cerebral embolism. He contributed seminal insights into lacunar strokes and their syndromes, cervical artery dissection, subarachnoid haemorrhage, and reversible cerebral vasospasm. His work advanced the use of anticoagulation in stroke prevention and enabled surgical interventions such as carotid endarterectomy.
Throughout his career, Fisher maintained an unwavering belief in clinical observation and pathological correlation, authoring over 200 publications. He described numerous neurological signs and syndromes, including Miller Fisher syndrome (a variant of Guillain–Barré syndrome), transient global amnesia (1958), ocular bobbing, one-and-a-half syndrome, and the Fisher grade for subarachnoid haemorrhage severity. His meticulous approach and mentorship helped define stroke as a primary neurological discipline.
Born in Waterloo, Ontario, Fisher graduated MD from the University of Toronto in 1938. During World War II, he served in the Canadian Navy and survived the sinking of HMS Voltaire, spending three and a half years as a German POW. After the war, he trained in neuropathology in Boston under Raymond Adams and later founded the first dedicated stroke service at Massachusetts General Hospital in 1954. Fisher continued to work well into his nineties and is remembered as a clinician, scholar, and mentor whose contributions transformed the field of stroke neurology.
Biography
- Born December 5, 1913 in Waterloo, Ontario, Canada
- 1935 – BA, Victoria University, Toronto
- 1938 – MD, University of Toronto
- 1938–1940 – Training at Henry Ford Hospital, Detroit, and Royal Victoria Hospital, Montreal
- 1940 – Volunteered for Canadian Navy; transferred to British Royal Navy
- 1941 – Aboard HMS Voltaire when sunk off Cape Verde; taken prisoner-of-war
- 1941–1944 – Prisoner in German POW camps
- 1945 – First publication: Marlag 1941–44 in Can Med Assoc J
- 1946 – Fellow at Montreal Neurological Institute under Wilder Penfield
- 1949–1950 – Neuropathology fellowship at Boston City Hospital under Raymond Adams
- 1950–1954 – Neuropathologist, Montreal General Hospital
- 1954 – Invited by Adams to Massachusetts General Hospital (MGH); established first dedicated Stroke Service
- 1956 – Described Miller Fisher syndrome (variant of Guillain–Barré syndrome)
- 1980 – Retired from professorship at MGH; remained active as Emeritus Professor at Harvard Medical School
- 1998 – Inducted into Canadian Medical Hall of Fame
- Died April 14, 2012 in Albany, New York, aged 98
Medical Eponyms
Miller Fisher syndrome (1956)
Miller Fisher syndrome (MFS) is a rare variant within the Guillain-Barré syndrome (GBS) spectrum, typically presenting with the triad of ataxia, areflexia, and ophthalmoplegia. It is considered part of the continuum of immune-mediated acute polyneuropathies, alongside GBS and Bickerstaff brainstem encephalitis (BBE).
Heel-Shin test (Heel-knee test) (1961)
In the legs, the heel–knee test with Fisher’s modification (tapping the shin with the heel of the other leg as well as running the heel down the length of the shin) is the only test in common usage
Fisher grade (1980)
Classification system for subarachnoid haemorrhage severity and vasospasm risk.
Miller Fisher’s seminal study of 47 patients with aneurysmal subarachnoid haemorrhage (aSAH) was a retrospective, single-center study that graded the amount/distribution of subarachnoid blood, and recorded the rate of angiographic and clinical vasospasm. While angiographic vasospasm was common, thick subarachnoid haemorrhage (greater than 1 mm thick) correlated with a high rate of clinical vasospasm
| Fisher grade | Blood on CT* | Risk of vasospasm |
|---|---|---|
| I | No SAH detected | Low (range 0-21%) |
| II | Diffuse or vertical layer of subarachnoid blood < 1mm thick | Low (range 0-25%) |
| III | Localized clot and/or vertical layer within the subarachnoid space > 1mm thick | Low to high (range 23-96%) |
| IV | ICH or IVH with diffuse or no SAH | Low to moderate (range 0-35%) |
2001 – Claassen et al developed the Modified Fisher Grading Scale for Subarachnoid Hemorrhage (SAH)
Fisher test
CSF tap test in diagnosis of normal pressure hydrocephalus
Major Publications
- Fisher M, Adams RD. Observations on brain embolism with special reference to the mechanism of hemorrhagic infarction. J Neuropathol Exp Neurol. 1951 Jan;10(1):92-4.
- Fisher M. Occlusion of the internal carotid artery. AMA Arch Neurol Psychiatry. 1951 Mar;65(3):346-77.
- Fisher CM. Transient monocular blindness associated with hemiplegia. AMA Arch Ophthalmol 1952;47(2):167-203. [Transient Ischaemic Attack]
- Fisher CM. An unusual variant of acute idiopathic polyneuritis (Syndrome of ophthalmoplegia ataxia and areflexia). NEJM, 1956; 255: 57-65. [Miller Fisher syndrome]
- Fisher CM, Adams RD. Transient global amnesia. Transactions of the American Neurological Association. 1958;83:143–6. [Transient Global Amnesia]
- Fisher CM. A simple test of coordination in the fingers. Neurology. 1960; 10: 745-746.
- Fisher CM. An improved test of motor coordination in the lower limbs. Neurology. 1961; 11(4)Pt 1: 335-336. [Heel-Shin test]
- Fisher CM. Concerning recurrent transient cerebral ischemic attacks. Can Med Assoc J. 1962 Jun 16;86(24):1091-9.
- Fisher CM, Adams RD. Transient global amnesia. Acta Neurol Scand. 1964;40(Suppl 9):1–81.
- Fisher CM, Kistler JP, Davis JM. Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. Neurosurgery. 1980 Jan;6(1):1-9.
- Fisher CM. ‘Transient monocular blindness’ versus ‘amaurosis fugax’. Neurology. 1989 Dec;39(12):1622-4.
- Fisher CM. A career in cerebrovascular disease: a personal account. Stroke. 2001 Nov;32(11):2719-24.
- Fisher CM. Transient ischemic attacks. N Engl J Med. 2002 Nov 21;347(21):1642-3.
References
Biography
- Mohr JP, Caplan LR, Kistler JP. C. Miller Fisher: An Appreciation. Stroke. 2012;43:1739-1740
- Caplan LR, Mohr JP, Ackerman RH. In memoriam: charles miller fisher, MD (1913-2012). Arch Neurol. 2012 Sep 1;69(9):1208-9.
- Koroshetz WJ, Mohr JP, Caplan LR. C. In Memoriam: C. Miller Fisher, MD (1913-2012). Neurology. 2012;79(10):969-70.
- Kubicki K, Grzybowski A. Pioneers in neurology: Charles Miller Fisher (1913-2012). J Neurol. 2022 Mar;269(3):1727-1729.
Eponymous terms
- Estol CJ. Dr. C. Miller Fisher and the history of carotid artery disease. Stroke. 1996;27(3):559-66.
- Noioso CM, Bevilacqua L, Acerra GM, Della Valle P, Serio M, Vinciguerra C, Piscosquito G, Toriello A, Barone P, Iovino A. Miller Fisher syndrome: an updated narrative review. Front Neurol. 2023 Aug 24;14:1250774.
- Fisher Grading Scale for Subarachnoid Haemorrhage (aSAH). MD Calc
- Modified Fisher Grading Scale for Subarachnoid Haemorrhage (SAH) MD Calc
Eponym
the person behind the name
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | On Call: Principles and Protocol 4e| Eponyms | Books |
