Dissociated Oxygen Saturations
aka Hematology Hoodwinker 004
One of the emergency residents has just taken an ABG on the 44 year-old woman in cubicle 3. Prior to her current presentation she had no known medical problems. The patient’s pulse oximetry reading is SpO2 98% on air.
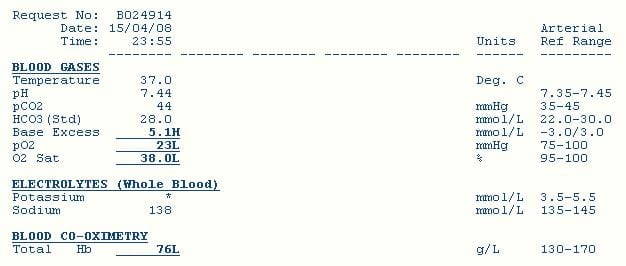
This is the arterial blood gas:
Questions
Q1. What are the possible explanations for the discrepancy between the pulse oximetry reading and the oxygen saturation on the arterial blood gas?
Answer and interpretation
Possible explanations for ‘pseudo-hypoxaemia’ include
- Equipment failure
— faulty pulse oximeter
— faulty blood gas analyser - Blood sample used was actually venous
- Blood sample taken from a site affected by localised hypoxemia, e.g. ischaemic limb
- Excessive oxygen consumption following blood sample collection (e.g. massive leukocytosis or thrombocytosis)
Dyshemoglobinemia can also cause a discrepancy between SpO2 and SaO2, but will not cause the decrease in measured PaO2 as seen in this case.
- In carbon monoxide poisoning SpO2 will read in the 90s despite high levels of COHb — but the PaO2 should still be high.
- In methemoglobinemia, the SpO2 plateaus at about 86% with increasing levels of MetHb, but again the PaO2 will not be decreased.
Q2. What other blood test would be particularly helpful?
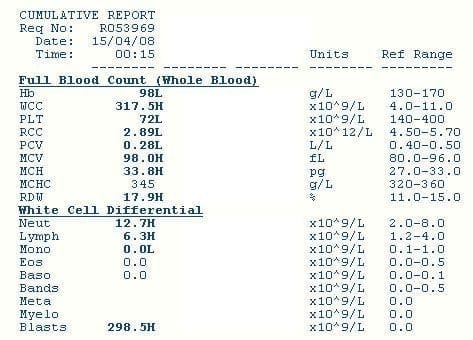
Q3. Describe the blood test result shown in Q2?
Answer and interpretation
The key findings are
- massive leukocytosis, due to a large number of blasts
- normocytic anemia (Hb 98 with normal MCHC), mild macrocytosis (MCV 98) and increased RDW (17.9)
- thrombocytopenia
Spurious hypoxaemia in this setting is also known as ‘leukocyte larceny’.
Q4. Interpret the blood test result shown in Q2? What is the likely underlying diagnosis?
Answer and interpretation
Acute myeloid leukemia
Hyperleukocytosis (>100 x 10E9/L) is almost always due to a hematological malignancy.
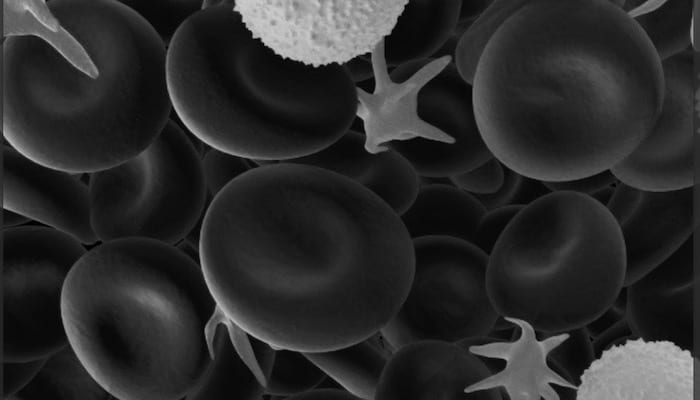
Blast cells in the blood suggest acute leukemia or a blast cell crisis. The presence of Auer rods in the blast cells would confirm the diagnosis of acute myeloid leukemia. Blast cell crisis occurs when chronic myeloid leukemia (CML) undergoes transformation into a more aggressive condition.
Blast cells are immature precursors of either lymphocytes (lymphoblasts), or granulocytes (myeloblasts). They do not normally appear in peripheral blood. They can be recognized microscopically by their large size and primitive nuclei (ie the nuclei contain nucleoli).
The anemia and thrombocytopenia is consistent with bone marrow failure.
Q5. What other complications is this patient at risk of?
Answer and interpretation
Potential complications include
- hyperviscosity syndrome due to massive leukocytosis (e.g. altered mental state, stroke, pulmonary leukostasis, renal insufficiency, and priapism)
- bleeding and disseminated intravascular coagulation (DIC)
- infections due to immune suppression
- syncope and ischemia due to anemia (decreased oxygen delivery)
- acute respiratory distress syndrome (ARDS) due to haematopoietic mediators, leukostasis and leukaemic cell lysis pneumopathy
- complications of treatment (e.g. chemotherapy side effects, tumour lysis syndrome, transfusion reactions, bone marrow transplant)
Note the possible respiratory complications of conditions that cause hyperleukocytosis — measured hypoxaemia may be real or spurious!
Q6. What are the treatment options?
Answer and interpretation
Management of hyperleukocytosis (>100 x 10E9/L in the context of AML) includes
- Treat the underlying condition (e.g. chemotherapy for AML) and subsequent complications such as tumour lysis syndrome
- Hydration
- Leukophoresis
- Avoid unnecessary blood transfusions
- Supportive care
Q7. How could the abnormal blood gas result be avoided?
Answer and interpretation
Abnormalities in PaO2, PaCO2 and pH may be mitigated in the presence of massive leukocytosis by
- processing the sample rapidly
- transporting the sample on ice
Note that massive leukocytosis can also result in pseudohypoglycemia due to ongoing glucose metabolism after a blood sample is collected.
References
- Cammalleri L, Malaguarnera M. Rasburicase represents a new tool for hyperuricemia in tumor lysis syndrome and in gout. Int J Med Sci. 2007 Mar 2;4(2):83-93. Review. PubMed PMID: 17396159; PubMed Central PMCID: PMC1838823.
- Chillar RK, Belman MJ, Farbstein M. Explanation for apparent hypoxemia associated with extreme leukocytosis: leukocytic oxygen consumption. Blood. 1980 Jun;55(6):922-4. PubMed PMID: 7378581. [fulltext]
- Lele AV, Mirski MA, Stevens RD. Spurious hypoxemia. Crit Care Med. 2005 Aug;33(8):1854-6. Review. PubMed PMID: 16096465.
- Mehta A, Lichtin AE, Vigg A, Parambil JG. Platelet larceny: spurious hypoxaemia due to extreme thrombocytosis. Eur Respir J. 2008 Feb;31(2):469-72. PubMed PMID: 18238952. [fulltext]
- Sacchetti A, Grynn J, Pope A, Vasso S. Leukocyte larceny: spurious hypoxemia confirmed with pulse oximetry. J Emerg Med. 1990 Sep-Oct;8(5):567-9. PubMed PMID: 2254603.
CLINICAL CASES
Hematology Hoodwinker
Intensivist in Wellington, New Zealand. Started out in ED, but now feels physically ill whenever he steps foot on the front line. Clinical researcher, kite-surfer | @DogICUma |

Wow . Thank you. Loved the way you presented and explained every abnormality with explanation