Echo basics: Tips and Tricks
Echocardiography tips and tricks on optimising your image, making measurements, recognising artefacts and controlling infection
Preparing to scan
Before you begin your scan, remember to ask yourself the following questions:
- Have you got the right equipment?
- Have you got the right patient?
- Have you entered the patient’s details accurately on the machine?
- Have you attached the ECG?
- Have you explained what you are going to do in a way your patient understands and gained verbal consent?
- Have you made allowances for any cultural/religious/language/disability/ individual patient preferences?
Optimising your image
Here are some tips you can use to obtain an optimal image:
Probe Frequency Adjustment
- Large patients: Use a lower scanning frequency to improve penetration.
- Small patients: Use a higher scanning frequency to enhance resolution.
Sector Width and Depth
- Adjust sector width and depth to visualise only relevant structures.
- Always readjust these parameters when changing the imaging window (e.g., from parasternal to apical, or apical to suprasternal views).
Gain Settings
- Avoid over-gaining the image, especially in well-lit environments.
- Use Time Gain Compensation (TGC) to enhance deeper structures:
- If your machine does not adjust automatically, ramp down the top 2–3 TGC sliders to reduce near-field echoes.
Focus and Zoom
- Align the focus with structures of particular interest.
- Use high-resolution zoom to improve visualisation of key anatomical areas.
Image Review Tools
- Use freeze and trackball functions to scroll slowly through image loops, allowing detailed examination.
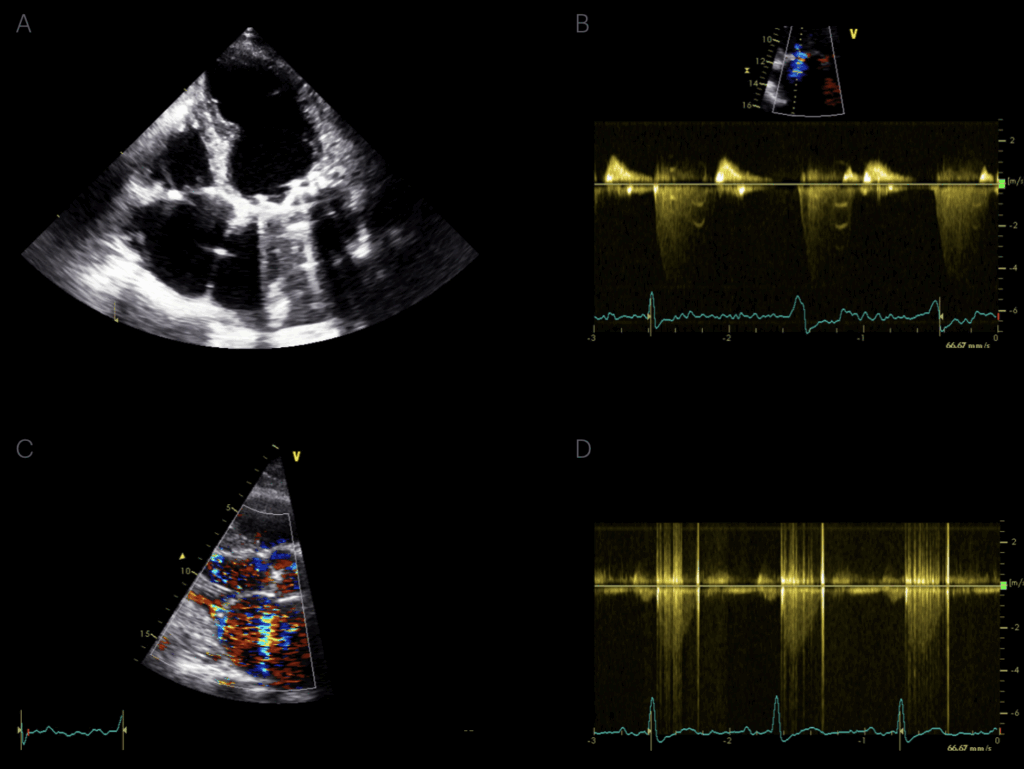
Doppler Optimisation
- Adjust velocity scale and sweep speed:
- Display 2–3 waveforms per image.
- Ensure waveforms occupy at least two-thirds of the y-axis for clarity.
Archiving and Image Capture
- Archive high-quality clips using ECG triggering for timing.
- Use cycle select to ensure the best cardiac cycle is stored.
Making measurements
To help you make your measurements, here are some things to keep in mind:
Departmental Conventions
- Always use the same measurement conventions as the rest of your department to ensure consistency and reproducibility.
Reference Ranges
- Ensure the normal ranges you reference are:
- Appropriate for your patient population, and
- Based on the same measurement conventions (e.g. inner-edge vs leading-edge) as when the reference values were established.
Measurement Techniques
Parasternal Views
- Use a leading edge-to-leading edge convention by default.
- Left Ventricular Outflow Tract (LVOT):
- Typically measured inner edge-to-inner edge.
- Aortic Root:
- Historically measured leading edge-to-leading edge in systole.
- Increasingly measured inner edge-to-inner edge in diastole, depending on local protocols.
Doppler Velocities
- Avoid overestimating Doppler velocities:
- Trace the main body of the waveform.
- Ignore artifacts, particularly at the tips of the waveform.
Ejection Fraction (Simpson’s Method)
- Do not attempt Simpson’s EF if the endocardium is not clearly visualised.
- Poor visibility leads to unreliable measurements and should prompt alternative methods or views.
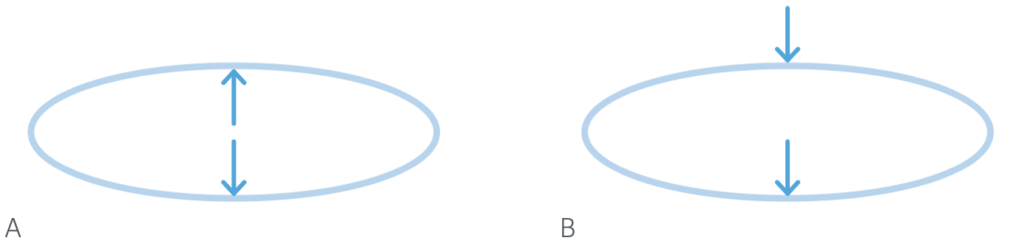
B. Leading edge to leading edge convention: top of an echo interface to the top of the interface below.
Recognising artefacts
An artefact can make it look like there is something present that isn’t there, or it may hide structures from being seen. If you suspect an artefact, try one of the following:
- Image from other views.
- Alter the machine settings.
- Observe whether it looks and moves physiologically.
Artefacts are particularly likely when there is material within the scanning zone which is unlike normal cardiac tissues, such as a pacing lead, replacement valve, air, or calcium. Typically, returning echoes are interpreted incorrectly because the normal assumptions about the behaviour of ultrasound in the body do not apply.
Controlling infection
This is an important component of performing an echo and will be informed by your institution’s policies and practice guidelines.
As a general rule, anything that touches the patient should be cleaned carefully after every scan. Some cleaning agents can damage ultrasound probes, so make sure you use a method the manufacturer supports and it’s good practice to routinely check the probe for damage before you use it.
This is an edited excerpt from the Medmastery course Echocardiography Essentials by Helen Rimington, PhD. Acknowledgement and attribution to Medmastery for providing course transcripts.
More echocardiography resources:
- Na, M. Echo Masterclass: Left Ventricular Strain. Medmastery
- Monteiro, C. Echo Masterclass: The Right Heart. Medmastery
- Eggett, C. Echo Masterclass: The Valves. Medmastery
- West, C. Echo Masterclass: Adult Congenital Heart Disease. Medmastery
- Naderi, H. Echo Masterclass: The Power of 3D Imaging. Medmastery
Radiology Library: Echocardiography basics
- Rimington H. Echo basics: Machines and probes. LITFL
- Rimington H. Echo basics: Tips and Tricks. LITFL
- Rimington H. Echo basics: Key concepts and Doppler modalities. LITFL
- Rimington H. Echo basics: Parasternal Views. LITFL
- Rimington H. Echo basics: Apical and Subcostal Views. LITFL
Echocardiography Essentials
Helen is a Consultant Cardiac Physiologist at Guy’s and St Thomas’ NHS Trust, in London (UK). She's also a co-author of Echocardiography: A Practical Guide for Reporting. | Medmastery

