Exogenous Calcium Embolism
aka Cardiovascular Curveball 010
A 62 y/o caucasian female (Mrs S) presented to the Emergency Department with sudden onset of dyspnoea and local back pain. The patient had sustained a compression fracture of the 5th lumbar vertebral body 2 months previously and had Percutaneous Vertebroplasty (PVP) performed 4 days prior to her ED presentation.
Mrs S complained of acute shortness of breath which came on suddenly after eating a light breakfast. She also complained of right sided chest pain, worse on inspiration. She denied any previous history of asthma, cardiac failure, COPD or recent respiratory illness.
Her past medical history includes Crohn’s disease (well controlled with infliximab and steroids) and osteoporosis (treated with Alendronate and Caltrate).
Baseline Examination and Investigations:
Examination of the lumbar region revealed the site of injection with no evidence of secondary infection or abscess formation.
- RS: RR 28, good air entry, BS vesicular with no evidence of pleural rub/ tracheal deviation. SaO2 96% on 8L of O2
- CVS: HR 128. No murmurs, parasternal heave or thrills.
- ABG: pH 7.51, pCO2 15, pO2 58
Q1. Interpret the Examination and Investigations
Answer and interpretation
- ECG: Sinus Tachycardia
- ABG: Respiratory alkalaemia with hypoxaemia
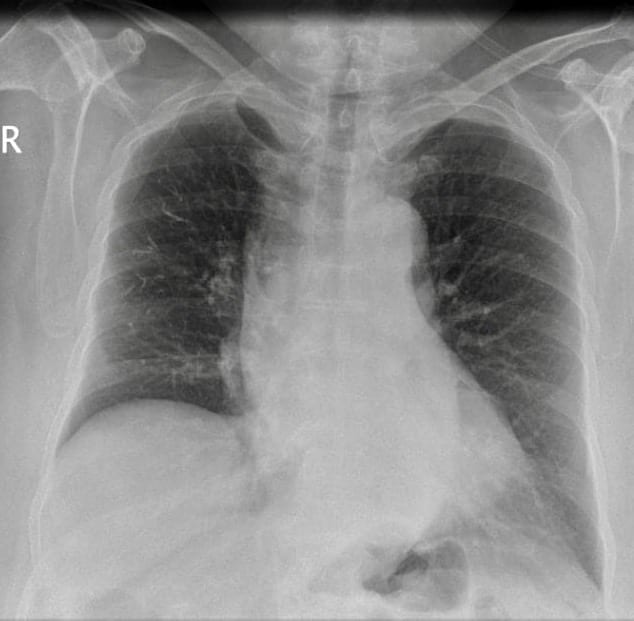
- CXR: Decreased vascular markings , dense tubular branching opacities in the right lung. No signs of consolidation or atelectasis.
Q2. What is your Differential Diagnosis?
Answer and interpretation
- Cement embolism secondary to PVP
- Pulmonary thromboembolism secondary to immobility after procedure
- Pneumothorax
Q3. What further Investigations are required?
Q4. What is the most likely diagnosis?
Curveball Answer
Cement embolism secondary to PVP for treatment of osteoporotic vertebral compression fractures mainly based on the CXR and CT findings.
Q5. Outline your management
Curveball Answer
- High flow oxygen via hudson mask to maintain SaO2 95%.
- IV morphine was titrated to relieve pain and she was started on anti-coagulation therapy: LMWH (clexane) 1mg/kg SC BD along with first dose of warfarin 10mg PO (subsequent daily doses titrated to achieve INR of 2.5-3.5).
- A surgical consult was sought to determine the possibility of cement fragment retrieval.
Learning Points
CEMENT EMBOLISM
Definition
- An embolus is a detached intravascular solid , liquid or gaseous mass that is carried by the blood to a site distant from its point of origin.
- 99% of all emboli originate from a dislodged thrombus, hence the term thromboembolism.
- Rare forms of emboli do occur including:
- Droplets of fat
- Bubbles of air
- Amniotic fluid
- Atheroslerotic (cholesterol) debris
- Tumour fragments
- Bone marrow
- Foreign bodies such as CEMENT
Pathophysiology
- Percutaneous vertebroplasty (PV) is an interventional radiologic procedure that involves injection of acrylic bone cement into a diseased vertebral body under fluoroscopic or CT guidance.
- The method was first described by Galibert in 1987 and has since become a standard treatment for osteoporotic vertebral compression fractures and osteolytic vertebral tumours.
- Because the cement is injected into the vertebral body under high pressure there is a high risk of it entering the perivertebral venous plexus (segmental vein), inferior vena cava and eventually into the pulmonary arteries.
- It may also induce a local inflammatory reaction at the vessel wall, leading to superimposed thrombosis on the surface of the cement and propagation of a thrombus down into the pulmonary tree.
Epidemiology
- A recent study has shown that cement embolism occurs more frequently than previously reported 6.8%. Current studies have shown that its incidence is as high as 23%.
- Cement leakage into the IVC is closely related to cement embolism.
Additional Case Report
An asymptomatic patient
- A 50-year-old female patient with an osteoporotic compression fracture of the second lumbar vertebra underwent PVP.
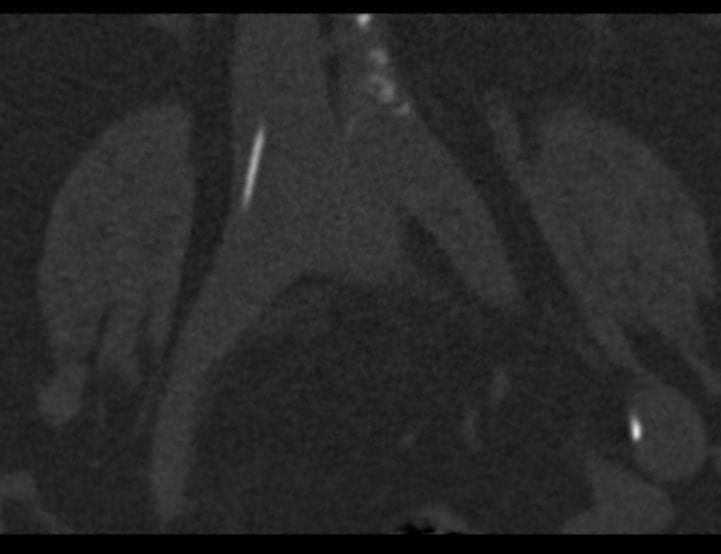
- Post-op abdo CT revealed small asymptomatic cement emboli in peripheral pulmonary arteries, along with a hook-shaped cement fragment in the inferior vena cava.
- Due to the risk that the large cement fragment could migrate to the pulmonary arteries, they were retrieved from the inferior vena cava through a surgical groin incision.
- The patient received anticoagulant treatment for 3 months and has been free of complaints after 1 year.
Conclusion
Close clinical follow-up, post-procedural CXR and CT scans if necessary, are important for the detection of pulmonary cement emboli at an early stage in post-PVP patients
References
- Kim, Y., Lee, J., Park, K., Yeom, J., Jeong, H., Park, J., & Kang, H. (2009). Pulmonary Cement Embolism after Percutaneous Vertebroplasty in Osteoporotic Vertebral Compression Fractures: Incidence, Characteristics, and Risk Factors Radiology, 251 (1), 250-259 DOI: 10.1148/radiol.2511080854
- C. Duran, M. Sirvanci, M. Aydogan et al. Pulmonary Cement Embolism: A Complication of Percutaneous Vertebroplasty. Acta Radiol 2007;48:854-859. [Reference]
- A. Baumann , J. Tauss, G. Baumannat el .Cement Embolization into the Vena Cava and Pulmonal Arteries After Vertebroplasty: Interdisciplinary Management. Eur J Vacs Endovacs Surg 2006; 31(5) : 558-561. [Reference]
CLINICAL CASES
Cardiovascular Curveball