Exophthalmos (Proptosis)
Exophthalmos, also known as proptosis, is an abnormal protrusion of the eyeball. It may indicate serious underlying pathology, including:
- Space-occupying lesions in the orbit or intracranial cavity
- Thyroid eye disease (TED)
Regardless of the cause, proptosis can compromise visual function and threaten ocular integrity.
Note: Some literature uses “exophthalmos” specifically for thyroid-related cases, using “proptosis” for all other causes.
Epidemiology
- In adults, Graves disease is the most common cause of unilateral or bilateral exophthalmos.
Pathology
Causes
Exophthalmos is broadly divided into:
1. Space-occupying lesions
| Category | Examples |
|---|---|
| Tumours | Orbital neoplasms |
| Trauma | Orbital fractures, retro-orbital haematomas |
| Infection | Orbital cellulitis, retro-orbital abscess |
| Vascular lesions | Cavernous sinus thrombosis, carotid-cavernous fistula, AVMs, hemangiomas, lymphangiomas |
| Coagulopathy | Retro-orbital haematomas (e.g. in anticoagulated patients) |
2. Endocrine
| Condition | Mechanism |
|---|---|
| Graves disease | Autoimmune orbital inflammation affecting fat and extraocular muscles; impaired venous outflow (e.g. superior ophthalmic vein) can worsen engorgement |
Complications
Complications may arise from either the underlying cause or the exophthalmos itself:
- Optic nerve compression: May cause irreversible vision loss from ischaemia
- Exposure keratopathy: Drying → corneal ulceration → secondary infection
Clinical Assessment
Key History
- Recent trauma
- Known thyroid disease
- Coagulopathy or anticoagulant use (e.g. warfarin, DOACs)
Examination Findings
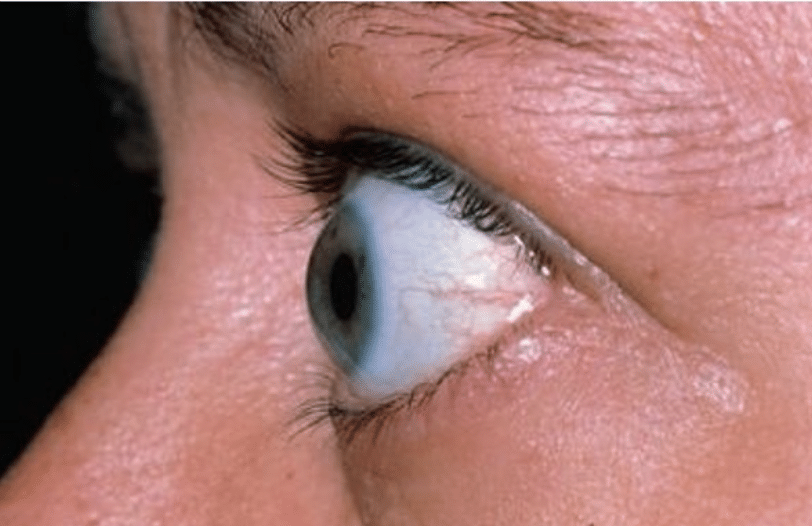
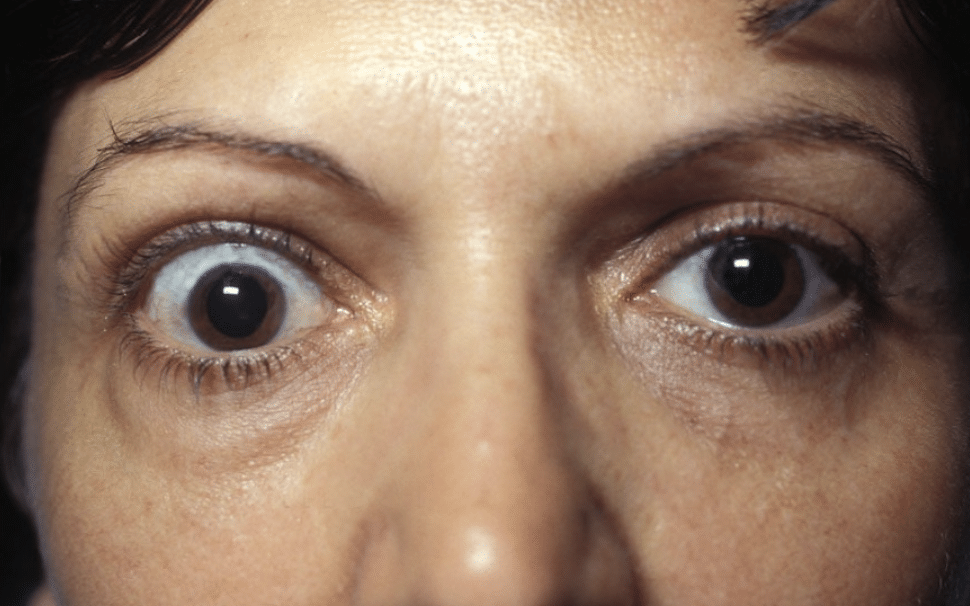
Protrusion of the globe may be obvious on inspection. A prominent feature is the visibility of the sclera above the cornea (which is normally hidden by the upper eye lid).
In more subtle cases, exophthalmos may be more apparent by observing the patient’s eye from the side or from above.
In general, a difference of > 2 mm between a person’s two eyes is considered abnormal.
| Examination Area | Purpose / Possible Findings |
|---|---|
| Conscious state and orientation | Altered mental state may suggest serious intracranial pathology |
| Vital signs | Fever may indicate infection (e.g. orbital cellulitis) |
| Visual acuity and pupillary reflexes | ↓ Visual acuity, RAPD, or visual field deficits suggest compressive optic neuropathy |
| External inspection | Obvious globe protrusion; sclera visible above cornea |
| Side/profile view of eyes | Helps detect subtle proptosis |
| Chemosis and conjunctival vessel engorgement | Suggest orbital congestion from mass or venous obstruction |
| Eye movements (EOMs) | Pain on movement, diplopia, or ophthalmoplegia suggest muscle or nerve involvement |
| Fundoscopy | Look for optic disc swelling or pallor |
| Slit lamp exam | Assess for exposure keratopathy or corneal ulceration (if indicated) |
| Periorbital tissues | Swelling, erythema, or tenderness may indicate periorbital/orbital cellulitis |
| Cranial nerve exam | Involvement of CN III, IV, V1, or VI may indicate cavernous sinus pathology |
| Palpation and auscultation of the globe/orbit | Pulsations or bruit may indicate carotid-cavernous fistula |
| Thyroid signs | Tremor, lid lag, tachycardia, or goitre suggest thyrotoxicosis |
Investigations
Bloods
- FBC
- CRP
- U&Es, glucose
- TFTs
- Coagulation profile
Imaging
| Modality | Use |
|---|---|
| B-scan ultrasound | For intraocular pathology when direct view obstructed (e.g. hyphema, cataract) |
| CT orbit with contrast | Good for orbital/intracranial masses, retro-orbital infection, vascular lesions, and Graves’ orbitopathy |
| MRI/MRA | Superior soft tissue detail and vascular lesion identification (e.g. cavernous sinus thrombosis) |
Management
Directed at:
- Underlying cause
- Secondary ocular complications:
- Lubricating eye drops
- Eye protection
- Surgical orbital decompression if needed
Disposition
- All patients with exophthalmos require Ophthalmology review
- Further referral (e.g. ENT, Neurosurgery, Endocrinology) depending on cause
Appendix 1
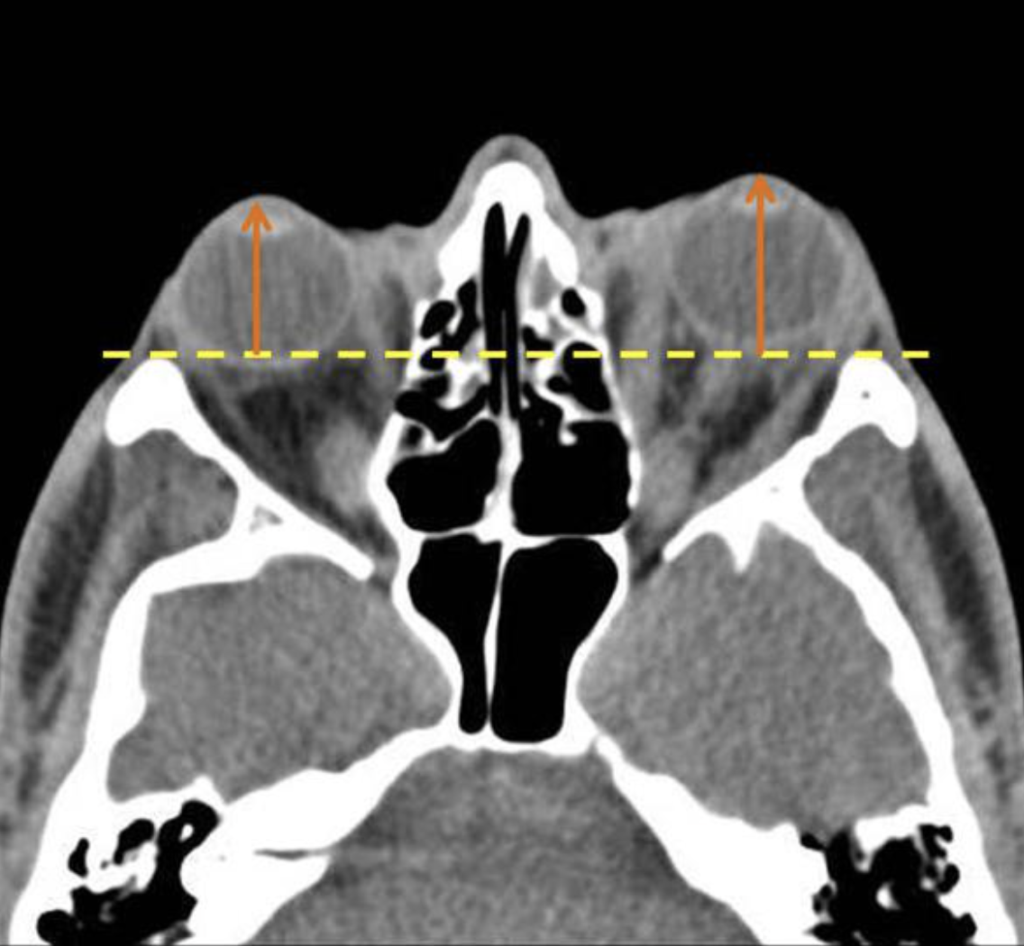
Axial CT images and at a level of the lens. If the distance from the anterior margin of the globe to interzygomatic line exceeds 21 mm, it is compatible with proptosis. In the case above the distance from anterior margin of the globe to interzygomatic line is 23 mm (right) and 25 mm (left). The findings are compatible with ocular proptosis due to thyroid ophthalmopathy.
Appendix 2
References
FOAMed
- Cadogan M. Graves disease. LITFL
Publications
- The Eye Emergency Manual, NSW Department of Health, 3rd ed. 2023
Fellowship Notes
Ba(Hons) Sheffield University, MBBS Newcastle University, MRCEM. UK Emergency Medicine doctor working in Australia |Stronger Medicine|
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |


