FFS: Asbestosis
Asbestosis is a form of pneumoconiosis caused by inhalation of asbestos fibres, resulting in slowly progressive, diffuse pulmonary fibrosis. It is part of the broader group of interstitial lung diseases and arises from occupational exposure to asbestos, a group of naturally occurring silicate minerals.
Three major disease entities related to asbestos exposure:
| Disease Type | Examples |
|---|---|
| Asbestosis | Chronic fibrotic lung disease |
| Pleural disease | Benign effusion, pleural plaques, diffuse pleural thickening |
| Malignant diseases | Small cell, squamous cell, adenocarcinoma, large cell carcinoma, mesothelioma |
All forms of asbestos are carcinogenic. The most deadly is crocidolite (blue asbestos).
Clinical Presentations
- Exacerbation of fibrosis → acute respiratory distress
- Complications: lung cancer, mesothelioma
- Pneumonia (common in fibrotic lung disease)
Emergency considerations:
Assess need for a limitations of care plan
Look for reversible causes (e.g. pneumonia, acute heart failure, ACS)
Geology and Exposure
Types of Asbestos Fibres
| Type | Form | Example | Notes |
|---|---|---|---|
| Serpentine | Coiled | Chrysotile (white) | >90% of commercial use |
| Amphibole | Straight/rigid | Crocidolite (blue), Amosite (brown), Tremolite, Actinolite, Anthophyllite | Crocidolite = highest risk of mesothelioma |
Asbestos fibres are microscopic and remain airborne for long periods, posing significant inhalation risks.
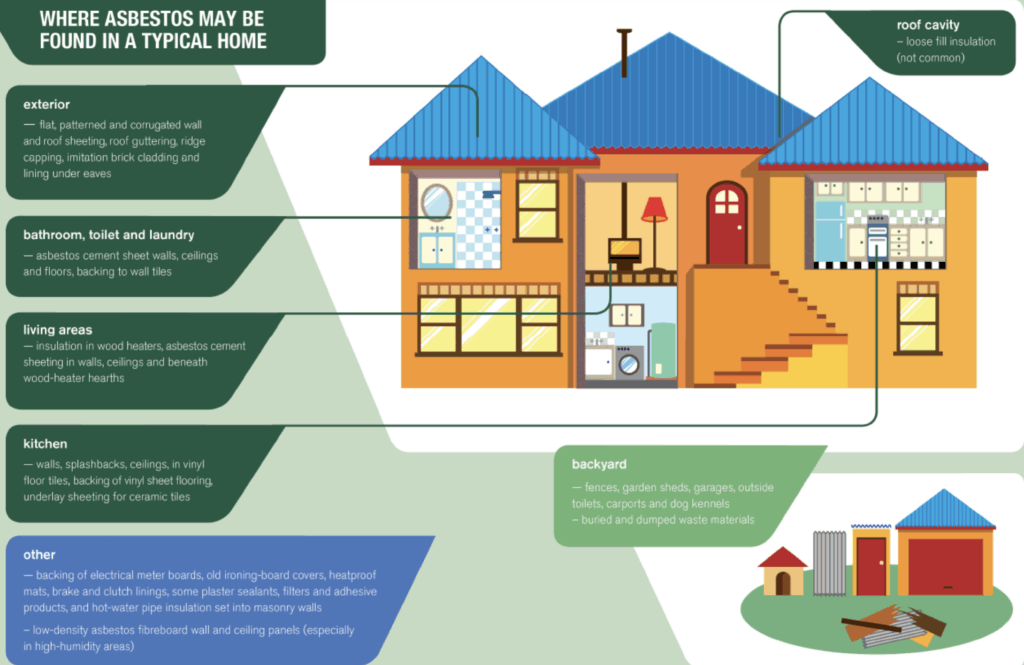
Asbestos Building Products
| Product Type | Risk Level | Examples |
|---|---|---|
| Friable | High (easily airborne) | Loose fill insulation, sprayed coatings |
| Bonded | Lower (fibres bound in cement) | AC sheeting, “fibro” |
Epidemiology
Risk is proportional to intensity, duration, fibre type, latency, and co-exposures (e.g. smoking).
Asbestos widely used in Australian buildings until late 1980s.
Total ban in Australia from 31 December 2003.
Pathology
Histological criteria:
- Asbestos (ferruginous) bodies
- Interstitial pulmonary fibrosis
Mechanism:
- Direct toxicity from fibres
- ROS and cytokine release
- Fibroblast proliferation and collagen accumulation
Amphibole fibres more toxic than chrysotile due to deeper lung penetration and poor clearance.
Clinical Features
| System | Features |
|---|---|
| Respiratory | Progressive exertional dyspnoea, fine bibasilar crackles, clubbing |
| Pleural | Benign effusions, plaques, diffuse thickening |
| Cardiac | Cor pulmonale in advanced disease |
| Complications | Respiratory failure, lung cancer, mesothelioma |
Latency: Symptoms may appear 20–30 years post-exposure.
Investigations
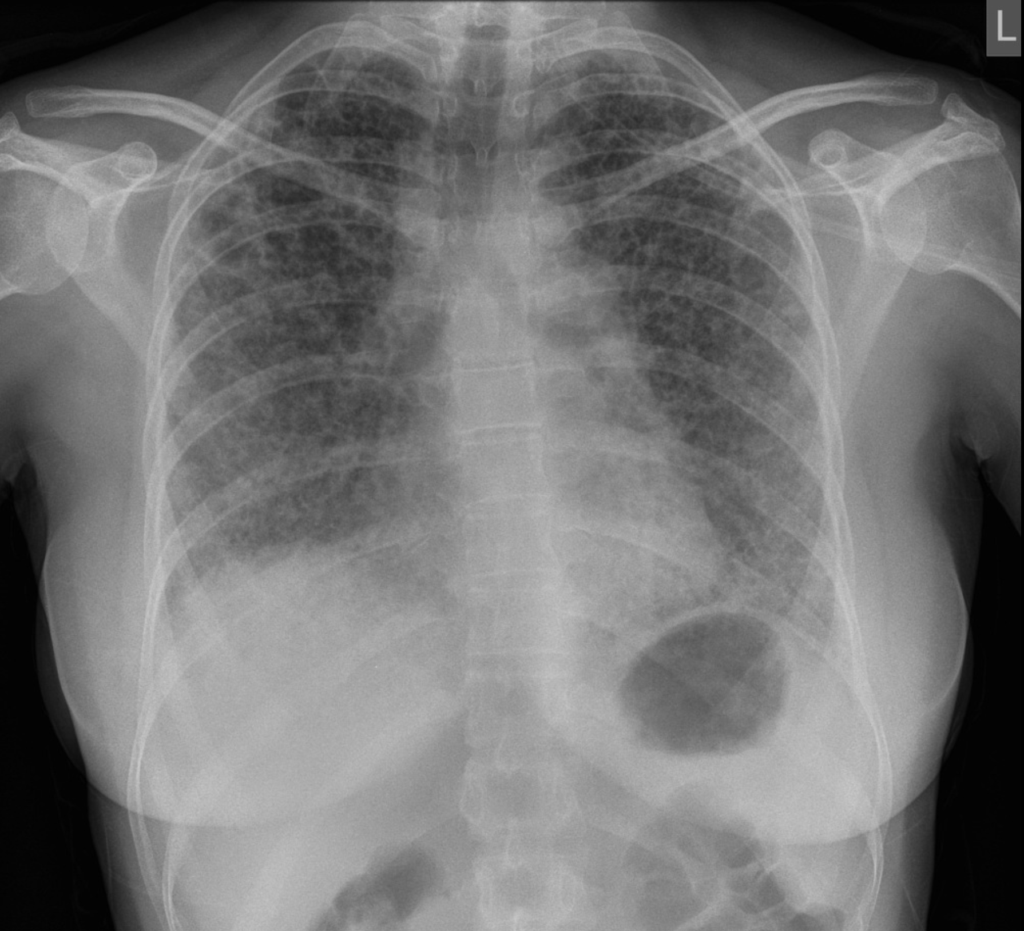
Imaging
| Modality | Findings |
|---|---|
| CXR | Basal reticular/nodular opacities, pleural plaques, “shaggy heart” sign |
| HRCT | Subpleural linear opacities, parenchymal bands, honeycombing, plaques |
Lung Function
- Restrictive pattern: ↓ VC, ↓ TLC, ↓ DLCO
- Early: exertional hypoxaemia
- Advanced: resting hypoxaemia
Others
- BAL: limited utility, may detect asbestos bodies
- Biopsy: rarely needed
Differential Diagnosis of Pleural Effusions
| Benign Effusion (BAPE) | Malignant Effusion |
|---|---|
| Small, unilateral, exudative | Often associated with cancer spread |
| Resolves over weeks to months | May require biopsy/thoracoscopy |
| Associated pleural plaques, atelectasis | Irregular septa, mediastinal involvement on CT |
Malignant Disease
| Malignancy | Notes |
|---|---|
| Lung cancer | Risk ↑ with smoking and amphibole exposure; multiplicative with smoking |
| Mesothelioma | 90% have confirmed asbestos exposure; most common = pleural mesothelioma |
Latency for mesothelioma: ~24 years
Exposure history and fibre type crucial to risk.
Management
General Principles
- No curative treatment
- Focus on prevention, support, and complication management
Prevention
- Cease exposure
- Cease smoking
- Vaccinate (influenza, pneumococcus)
Supportive
- Oxygen therapy for hypoxaemia
- Specialist respiratory follow-up
ED Management of Acute Respiratory Distress
| Step | Approach |
|---|---|
| Oxygenation | High-flow O₂; consider HFNO or CPAP |
| NIV | CPAP preferred unless T2RF present |
| Intubation | Consider if failing NIV; use restrictive ventilation strategy |
Ventilation Strategy (Restrictive Pattern):
- Low Vt (4–6 mL/kg IBW)
- High frequency (18–25 bpm)
- High I:E ratio (>1:1)
- PEEP 10–20 cmH₂O
- FiO₂ ≥ 0.6 initially, titrate to SpO₂ ≥ 88%
- Permissive hypercapnia acceptable
- Avoid fluid overload; use vasopressors if hypotensive
Appendix 1
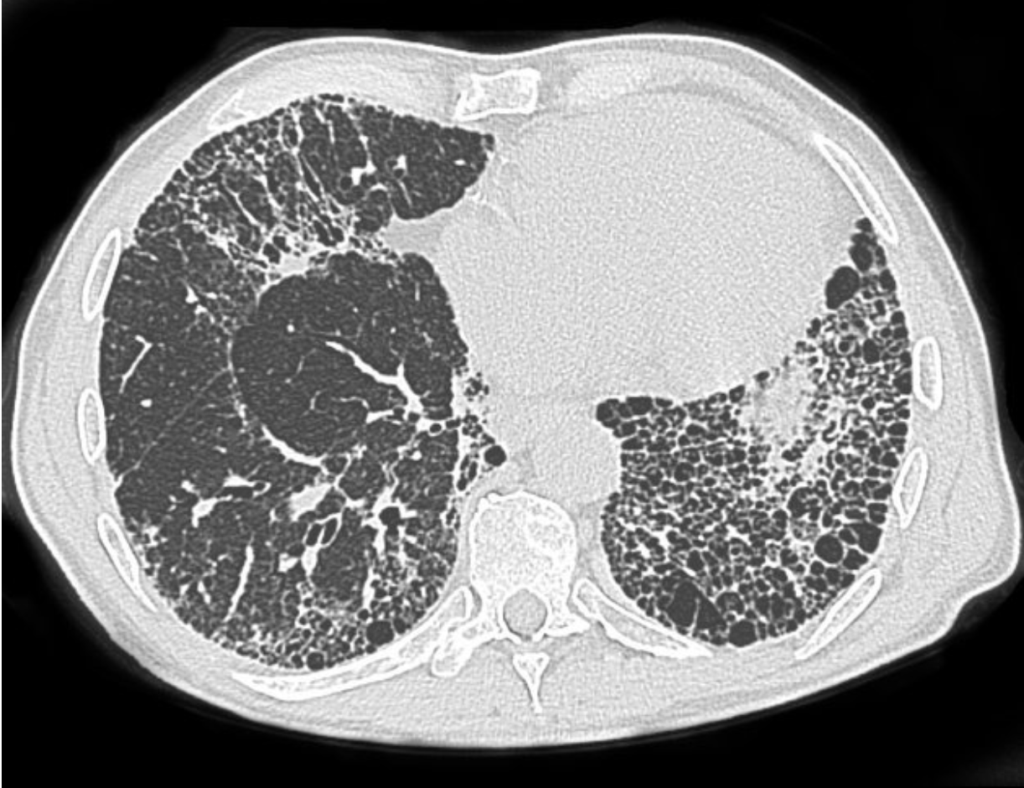
Appendix 2
References
FOAMed
- Brims F. CXR Case 128. LITFL
Resources
- National Association of Testing Authorities (NATA)
- Australian Asbestos Network
- Asbestos Diseases Society of Australia
- Better Health Channel
- Dust Diseases Board (NSW)
- Asbestoswise
Fellowship Notes
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |

