From the Hip
aka Oncological Quandary 001
Consider a 16 year old who presents with a 3 week history of severe hip pain followed by increasing breathlessness and left sided chest pain.
Day 1: Hip Biopsy
- A biopsy is performed on a left hip lesion which reveal a small blue round cell tumour
Questions
Q1. What are the potential causes?
Answer and interpretation
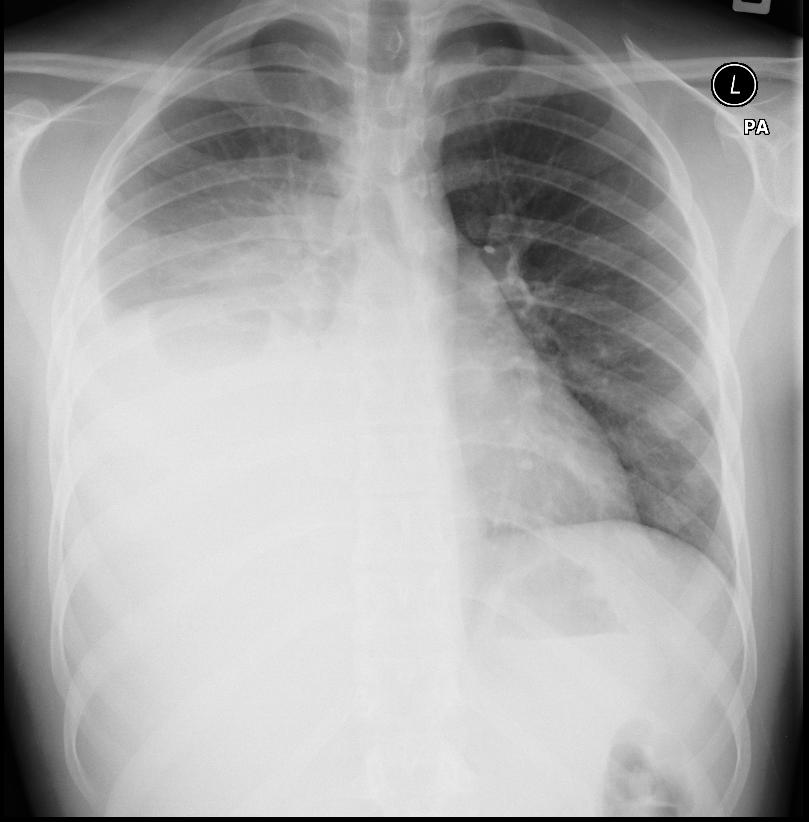
Potential causes of unilateral ‘white-out’ of a hemithorax:
- pleural fluid e.g. hemothorax, chylothorax, pleural effusion.
- complete collapse of one lung (e.g. due to obstruction of a main bronchus)
- dense consolidation of one lung
- an entire hemithorax full of cancer
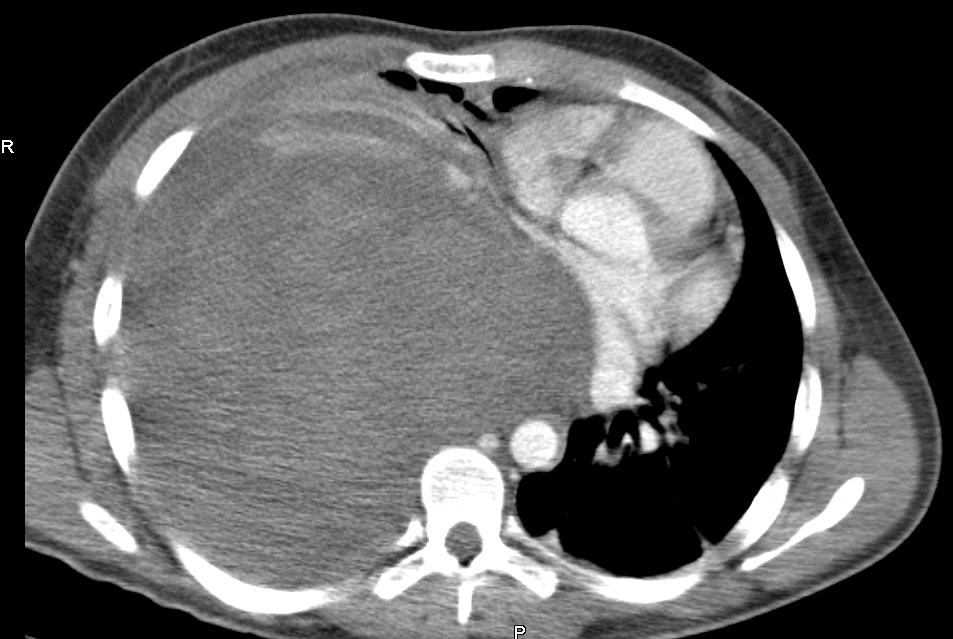
In this case the entire hemithorax is filled with cancer. A CT of the chest shows the tumour mass.
- The advice of the Medical Oncologist is that this tumour may respond to chemotherapy and there is a good chance of cure; however, it may take a week or more for the patient to respond to treatment.
- The patient is admitted to the Intensive Care Unit and symptoms of breathlessness continue to worsen.
Q2. How will you manage this?
Answer and interpretation
This a big problem!
- The chest X-ray reveals that the right lung is not aerated and the left main bronchus is significantly narrowed. Progressive breathlessness may indicate that the tumour is continuing to expand.
- Intubation is not likely to improve the situation if this is the case and, if the patient is up to it, you may need to have a difficult conversation about limitations of therapy.
- If the patient is going to be intubated, the risk of death around the time of intubation is significant as you may not be able to ventilate the patient. In addition, the CT scan reveals that the tumour is compressing the right ventricle.
- The risk of haemodynamic embarrassment at the time of intubation is significant. The patient, the patient’s family and staff need to know that the patient is likely to die around the time of intubation.

CLINICAL CASES
Oncology Quandary
Intensivist in Wellington, New Zealand. Started out in ED, but now feels physically ill whenever he steps foot on the front line. Clinical researcher, kite-surfer | @DogICUma |


ECMO would probably be something to consider. It might buy time, and also allow you to attempt one lung ventilation after passing a double lumen tube while keeping the patient oxygenated.
My thoughts precisely. Probably a VV ECMO with maintenance of reasonable left lung inflation while chemo has time to work. The difficult discussions still have to occur, however.