Funtabulously Frivolous Friday Five 304
Just when you thought your brain could unwind on a Friday, you realise that it would rather be challenged with some good old fashioned medical trivia FFFF, introducing the Funtabulously Frivolous Friday Five 304
Question 1
An 8 year old girl presents to your ED one month after an infection with Hand, Foot and Mouth disease (Coxsackievirus A16) with a particular body part falling off. What is she shedding?
Reveal the funtabulous answer
Her finger nails.
A rare but recognised complication of Coxsackie A16 is Onychomadesis (from the Greek Onyx for nail and madesis – ‘growing bald’). Onychomadesis is an acute, non-inflammatory, painless, proximal separation of the nail plate from the nail matrix. It occurs due to an abrupt stoppage of nail production by matrix cells, producing temporary cessation of nail growth (plus or minus subsequent complete shedding of nails).
Onychomadesis can present broadly: ranging from mild transverse ridges of the nail plate (Beau lines) to complete nail shedding. Onychomadesis may be related to systemic and dermatologic diseases, drugs (e.g. chemotherapeutic agents, anticonvulsants, lithium, retinoids), nail trauma, fever, or infection. The connection between onychomadesis and hand-foot-and-mouth disease was first described by Clementz in the year 2000.
Reference:
- Clementz GC, Mancini AJ. Nail matrix arrest following hand-foot-mouth disease: a report of five children. Pediatr Dermatol. 2000;17:7-11
Question 2
Your next patient is a 59 year old woman, currently on Norfloxacin for UTI. Which of the following is NOT a known side effect of fluoroquinolone antibiotics?
- Guillain-Barré syndrome
- DRESS syndrome
- Gastroparesis
- Interstitial nephritis
- Tendon rupture.
Reveal the funtabulous answer
Gastroparesis
Amongst the many adverse events noted from fluoroquinolone therapy, gastroparesis does not (yet) make a mention. Other GI effects include pseudomembranous colitis, pancreatitis, hepatitis, cholestatic jaundice, and elevated liver function tests.
The incidence of subjects reporting drug related adverse experiences in clinical trials was 3.4%, however the overall incidence is closer to 10.7%. Most adverse reactions occur within the first few days of therapy, the most common of which are either gastrointestinal or neurological: nausea 2.8%, headache 2.7% and dizziness 1.8%.
Unlike some of the first antibiotics discovered during the past century, the quinolone class of antimicrobial agents was not isolated from living organisms but rather, was synthesized by chemists. The prolific development of the quinolones began in 1962, when Lesher et al. made the accidental discovery of nalidixic acid as a by-product of the synthesis of chloroquine.
Reference:
- Andriole VT. The Quinolones: Past, Present, and Future. Clin Infec Dis. 2005;41(2):S113-119
Question 3
Name the disease from the following clues:
Reveal the funtabulous answer
Cushing Syndrome
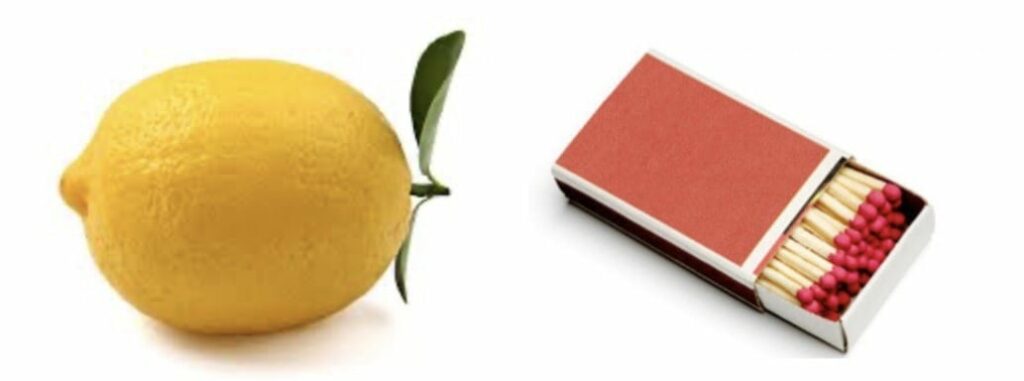
Although an unflattering and somewhat rude description, I remember being taught back in medical school that people with Cushing’s syndrome are meant to resemble a ‘lemon on matchsticks’ (also ‘lemon on toothpick’) to refer to their central adiposity and thinned arms and legs. Other common signs include:
- ‘Moon face’
- ‘Buffalo hump’
- Facial plethora
- Violaceous straie
- Proximal muscle weakness
- Easy bruising
It is worth noting the confusion that Cushing’s syndrome and Cushing’s disease are separate entities. Cushing’s syndrome refers to a clinical state characterized by excessive cortisol levels, whereas Cushing’s disease (far more rare) is specific for the same hypercortisolaemic state caused by a pituitary adenoma.
Other causes of raised cortisol include:
- Cortisol producing adrenal tumours.
- ACTH produced tumours at other sites.
- Exogenous steroid use. Less common causes of elevated cortisol levels.
- Pseudo-Cushing’s: chronically elevated cortisol due to: depression, alcohol abuse, anorexia nervosa or high estrogen levels.
Reference:
- UCLA – Cushing’s disease
Question 4
Speaking of matchsticks, what caused the women to strike in the Matchstick girls’ strike of 1888?
Reveal the funtabulous answer
‘Phossy jaw’, or osteonecrosis of the jaw from exposure to white phosphorous.
In the early 19th century, white phosphorous was added to matchstick heads to make them easier to ignite. The demand for the new ‘strike-anywhere’ matches was enormous, creating a profitable international industry. It also led to a new industrial disease that lasted until roughly 1906, when the production of phosphorous matches was outlawed by the International Berne Convention. The strike itself was caused by chronic poor working conditions in the match factory including fourteen-hour work days, poor pay, excessive fines, and the severe health complications of working with white phosphorus.
Phosphorus necrosis of the jaw, commonly called ‘phossy jaw’, was a genuinely horrible disease and overwhelmingly one of the poor. Workers in match factories developed unbearable abscesses in their mouths, leading to facial disfigurement and sometimes fatal brain damage. In addition, the gums developed an eerie greenish white ‘glow’ in the dark.

Reference:
- Royal College of Surgeons – “Phossy jaw” and the matchgirls: a nineteenth-century industrial disease
- Wikipedia – Phossy Jaw
Question 5
Why is ‘Phossy Jaw’ still relevant today?
Reveal the funtabulous answer
It still exists, in a form. BRONJ, or bisphosphonate (BP)-related osteonecrosis of the jaw.
BRONJ was first described only in 2003 by Marx et al. In general, intravenous nitrogen containing bisphosphonates shows higher incidence of BRONJ but a large variation ranging from 0.0% to 28% has been reported depending upon the specific type of bisphosphonate used, single or multiple BPs used concomitantly or sequentially, duration of therapy and the condition for which BPs were administered.
Oral BPs have also been associated with BRONJ, although at much lower percentage, not more that 4%.
Reference:
- Sharma D et al. Bisphosphonate-related osteonecrosis of jaw (BRONJ): diagnostic criteria and possible pathogenic mechanisms of an unexpected anti-angiogenic side effect. Vasc Cell. 2013; 5: 1
- Marx RE. Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg. 2003; 61(9): 1115-7
…and finally


FFFF
Funtabulously Frivolous Friday Five
Dr Mark Corden BSc, MBBS, FRACP. Paediatric Emergency Physician working in Northern Hospital, Melbourne. Loves medical history and trivia...and assumes everyone around him feels the same...| LinkedIn |