Hunt-Hess Scale
Description
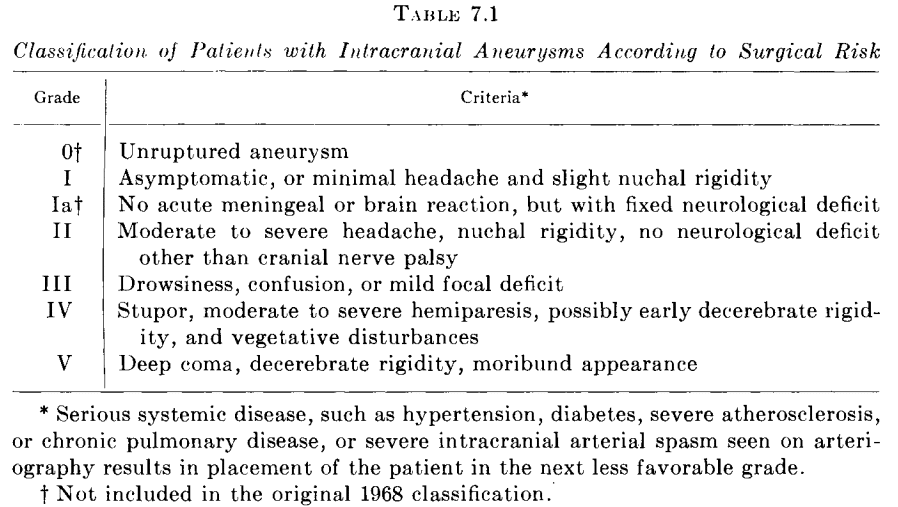
The Hunt-Hess Scale is a graded scale used to predict the rate of mortality based solely on the clinical features seen in a patient presenting with an aneurysmal subarachnoid haemorrhage.
| Grade | Characteristic | Mortality Rate1,2 |
| 0 | Unruptured aneurysm without symptoms | 0% |
| 1 | Asymptomatic or minimal headache with slight nuchal rigidity | 1-3% |
| 1a | No acute meningeal or brain reaction but with fixed neurological deficit | 1-3% |
| 2 | Moderate to severe headache, nuchal rigidity, no neurological deficits other than cranial nerve palsy | 3-5% |
| 3 | Drowsy, confused, or mild focal deficit | 9-19% |
| 4 | Stupor, moderate to severe hemiparesis, possible early decerebrate rigidity, and vegetative disturbances | 23-42% |
| 5 | Deep coma, decerebrate rigidity, moribund | 70-77% |
2. A key feature of the Hunt and Hess Scale is the requirement to increase a patient’s grade by one level in the presence of serious systemic disease or severe vasospasm on angiography. However, this rule is inconsistently applied, thereby affecting the interpretation of study results and possibly undermining prognostic value. Furthermore, only some qualifying diseases were defined in the initial study, and the level of severity necessary for upgrading is unclear.
History of the Hunt-Hess Scale
1956 – Edmund Harry Botterell, alongside William Lougheed, John Scott, and Stuart Vandewater graded the operative risk of 23 patients with cerebral aneurysms in their study on the use of hypothermia to minimize the effects of anoxia.
1968 – William Hunt, alongside his resident at the time Robert Hess, modified Botterell’s classification to determine the surgical risk in 275 patients presenting with aneurysmal subarachnoid haemorrhages.
It is generally agreed that the surgical risk in intracranial aneurysm is closely related to the patient’s condition at the time of surgery, as well as to other factors such as age, associated disease, and the location of the aneurysm…we have felt that the intensity of the meningeal inflammatory reaction, the severity of neurological deficit, and the presence or absence of significant associated disease should provide the best clinical criteria for the estimate of surgical risk.
Hunt, Hess 1968
1974 – Hunt, alongside Edward J. Kosnik, modified the 1968 classification to include the new grades ‘0’ and ‘1a’. The rule of increasing the grade of severity in the presence of serious systemic disease was also added.
Associated Persons
- Edmund Harry Botterell (1906 – 1997)
- William Edward Hunt (1921 – 1999)
- Robert McDonald Hess, Jr (1931 – 2019)
- Edward James Kosnik Jr. (1945 – 2018)
Alternative names
- Hunt and Kosnik Scale
- Modified Botterell Scale
Validity and Variability
The initial 12-year and 18-year study findings revealed substantially higher mortality rates for each grade than those seen in more modern-day studies. The differences in the mortality rates may be attributed to advances in the field of surgery.
Inter-observer variability is high, with the scale having an overall κ value of ~0.48 as according to a 2011 study with 103 paired assessments. The variability is higher than the Glasgow Coma Scale and the World Federation of Neurosurgical Societies Scale.
On the contrary, a 1998 comparison of the scale to the GCS and WFNSS on 185 patients showed that the Hunt and Hess Scale has the strongest predictive power for patient outcome at 6 months, with scores on the day of operation being of more prognostic value than scores observed immediately upon admission. However, sensitivities, specificities, and predictive values of almost all scale grades, in general, were poor.
References
- Botterell EH, Lougheed WM, Scott JW, Vandewater SL. Hypothermia, and interruption of carotid, or carotid and vertebral circulation, in the surgical management of intracranial aneurysms. J Neurosurg. 1956 Jan;13(1):1-42.
- Hunt WE, Hess RM. Surgical risk as related to time of intervention in the repair of intracranial aneurysms. J Neurosurg. 1968;28(1):14-20.
- Hunt WE, Kosnik EJ. Timing and Perioperative Care in Intracranial Aneurysm Surgery. Clin Neurosurg. 1974;21:79-89.
- Aulmann C, Steudl WI, Feldmann U. Validation of the prognostic accuracy of neurosurgical admission scales after rupture of cerebral aneurysms. Zentralbl Neurochir. 1998;59(3):171-80.
- Hacein-Bey L, Provenzale JM. Current imaging assessment and treatment of intracranial aneurysms. AJR Am J Roentgenol. 2011 Jan;196(1):32-44.
- Degen LA, Dorhout Mees SM, Algra A, Rinkel GJ. Interobserver variability of grading scales for aneurysmal subarachnoid hemorrhage. Stroke. 2011 Jun;42(6):1546-9.
- Lantigua H, Ortega-Gutierrez S, Schmidt JM, Lee K, Badjatia N, Agarwal S, Claassen J, Connolly ES, Mayer SA. Subarachnoid hemorrhage: who dies, and why? Crit Care. 2015 Aug 31;19(1):309.
eponymictionary
the names behind the name
Lewis is an RMO at Royal Perth Hospital. He is currently interested in critical care medicine.