ICE 007: Abdominal pain investigations
A 57 year old man presents to the ED with 18 hours of severe upper abdominal pain, fever, nausea and vomiting. He looks jaundiced, his HR is 120bpm, BP 110/60, RR 22 and his temperature is 37.8oC. He is tender and guarded in his right upper quadrant on abdominal palpation.
Questions:
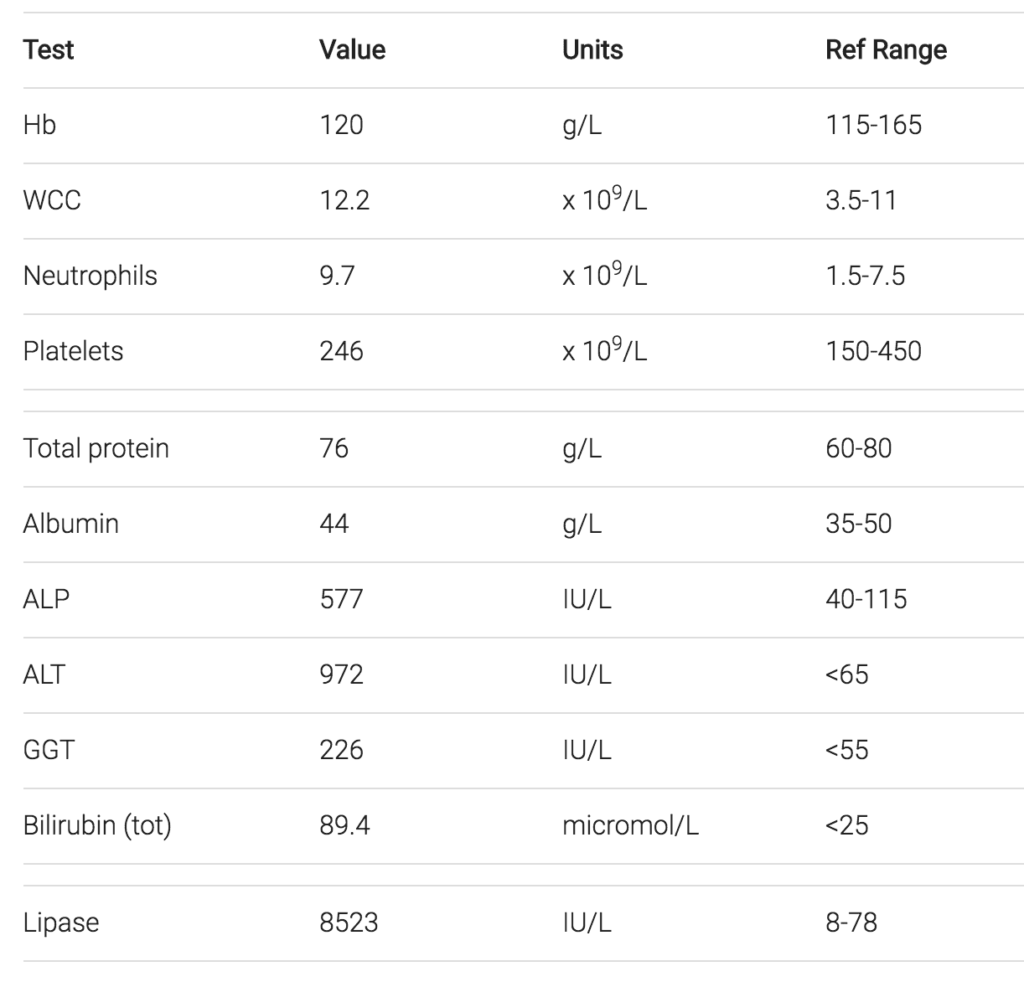
- Describe the blood test results
- What is the most likely diagnosis?
- What treatment is required in ED?
- What ongoing management is required?
Reveal the ICE answer
The bloods show a mild neutrophilia, grossly elevated lipase and substantially deranged liver functions tests. His jaundice is confirmed biochemically and the pattern of LFT derangement with all of the ALP, ALT and GGT elevated is a mixed one (suggesting both hepatitic and obstructive changes)
The most likely diagnosis given the clinical context is gallstone pancreatitis & ascending cholangitis due to a stone obstructing the lower biliary tract. An important differential is severe alcoholic pancreatitis.
In ED this patient needs;
- Aggressive IV fluid resuscitation
- Nil by mouth and NG tube
- Analgesia – titrated IV morphine or fentanyl
- Antibiotics – parenteral broad spectrum, for example “triple therapy” amoxycillin /gentamycin / metronidazole
It is essential that his ongoing management be in a centre that can perform an ERCP as relief of his biliary obstruction is critical in resolution of the illness. The severity of such a presentation should not be underestimated. There is a significant mortality and a range of potential complications such as pancreatic pseudocyst formation.

ICE CASES
Ian’s clinical emergencies
emergency physician keen on medical education and cycling