James Kernohan
James Watson Kernohan (1896-1981) was a Northern Irish born, American neuropathologist
James W. Kernohan was born in County Antrim, Northern Ireland and trained at Queen’s University Belfast. He migrated to the United States in 1922, joining the Mayo Clinic where he became a central figure in anatomic pathology. His early collaboration with neurologist Henry Woltman (1889-1964) led to the first description of Kernohan–Woltman notch phenomenon. This paradoxical ipsilateral neurological deficit associated with cerebral peduncle compression during brain herniation, a concept that challenged conventional neuroanatomical assumptions at the time.
Kernohan was instrumental in the development of neuropathologic classification systems for brain tumors. His 1949 publication A Simplified Classification of the Gliomas, co-authored with Adson and colleagues, introduced a pragmatic, histologically grounded grading system for central nervous system neoplasms that significantly influenced neuro-oncology practice for decades. Beyond brain tumors, Kernohan contributed to the understanding of Hirschsprung disease, disc degeneration, and other systemic pathology. His major reference text, Tumors of the Central Nervous System (1952), became a foundational resource, bridging the disciplines of surgery, neurology, and pathology.
A prolific academic, Kernohan published more than 170 articles, 11 book chapters, and three books. He served as President of the Mayo Clinic Staff in 1952 and was twice elected President of the American Board of Pathology (1957, 1959). His dedication to the discipline continued beyond formal retirement in 1961, with a late-career appointment at the Barrow Neurological Institute and publications into the 1970s.
Biographical Timeline
- Born October 1, 1896 in County Antrim, Northern Ireland .
- 1920 – Graduated from Queen’s University Belfast with degrees in Medicine (M.B.), Surgery (B.Ch.), and Obstetrics (B.A.O.) .
- 1921 – Diploma in Public Health (D.P.H.) and a Bachelor of Science (B.Sc.), with First Class Honours, also from Queen’s University .
- 1921–1922 – Clinical Pathologist at Crichton Royal Institute, Dumfries, Scotland.
- 1922 – Migrated to the United States; became a Fellow in Pathology at the Mayo Graduate School of Medicine, Minnesota.
- 1924 – MD, University of Minnesota. Thesis: The Ventriculus Terminalis: Its Growth and Development.
- 1925 – Appointed Consultant in Anatomic Pathology at the Mayo Clinic.
- 1929 – Co-authored landmark paper with Henry Woltman (1889-1964) describing the paradoxical Kernohan–Woltman notch phenomenon.
- 1931 – Published first study on spinal tumours, marking his expansion into CNS tumor pathology.
- 1943–1955 – Served as Head of the Section of Anatomic Pathology at the Mayo Clinic.
- 1949 – Published seminal work A Simplified Classification of the Gliomas, proposing a four-tiered histological grading system for CNS tumours (astrocytomas, ependymomas, oligodendrogliomas, neuroastrocytomas).
- 1952 – President of the Staff of the Mayo Clinic. Co-authored the textbook Tumors of the Central Nervous System with Adson and Craig.
- 1957 – President of the American Board of Pathology (and again in 1959)
- 1961 – Retired from Mayo Clinic after nearly 40 years of service.
- 1962–1964 – Affiliated with Barrow Neurological Institute, Phoenix, Arizona.
- 1966 – Awarded Honorary Doctor of Science (D.Sc.) from Queen’s University Belfast.
- 1970s – Continued to publish in neuropathology well into retirement.
- Died on May 5, 1981 in Rochester, Minnesota.
Medical Eponyms
Kernohan-Woltman notch phenomenon (KWNP) (1928)
KWNP is a false localising sign that occurs in the context of transtentorial (uncal) herniation. The phenomenon results from compression of the contralateral cerebral peduncle (crus cerebri) against the tentorial edge, leading to motor weakness on the same side as the original lesion. This paradoxical presentation is contrary to typical neuroanatomical expectations.
1929 – Kernohan and Henry William Woltman (1889-1964) published “Incisura of the crus due to contralateral brain tumour” presenting a series of cases in which ipsilateral hemiparesis contradicted expected localising principles.
[There is] a discrepancy between the seat of the lesion and the side of the motor defect — which demands consideration in connection with a known mechanical distortion of midbrain structures.
Notching of the crus cerebri by the free margin of the tentorium could, we believe, explain the homolateral signs of the pyramidal tract noted in most of our cases
Kernohan & Woltman, 1929
The paper analysed autopsy-confirmed cases with supratentorial lesions, all showing a “notch” in the contralateral crus cerebri (cerebral peduncle). The authors attempted to rationalise clinical signs with pathological findings, correlating ipsilateral hemiparesis to contralateral peduncular damage, induced by transtentorial herniation.
The notch itself was interpreted as a result of the contralateral cerebral peduncle being compressed against the rigid tentorial edge by midline brain shift. Over time, this mechanical force led to demyelination and necrosis of descending corticospinal fibres, the structural basis of the paradoxical hemiparesis.
The phenomenon described is not merely of academic interest; it bears directly on problems of localisation, diagnosis, and surgical approach in cases of brain tumour.
Kernohan & Woltman, 1929
Kernohan’s Notch (Motor, Cerebral)
Over time, the indentation or groove on the cerebral peduncle formed by tentorial herniation came to be referred to independently as Kernohan’s notch. This term denotes the visible midbrain deformation found at autopsy or on imaging, regardless of whether a false localizing sign is observed clinically.
While the KWNP describes the clinical phenomenon, Kernohan’s notch is the pathological or radiological substrate. Recognition of this notch on MRI or CT can be crucial for interpreting signs of uncal herniation or increased intracranial pressure.
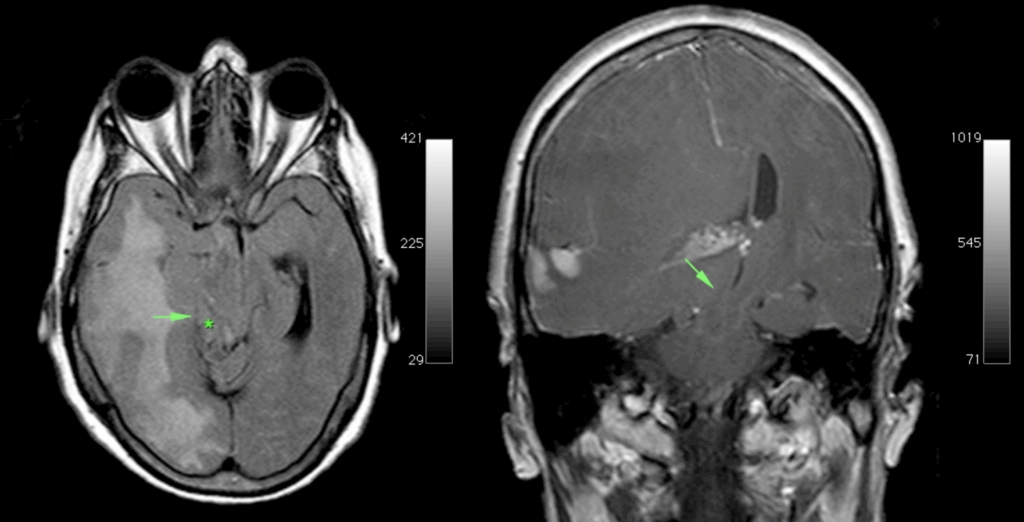
Mass effect of the tumour, with medial part (uncus) of the right temporal lobe (arrow) is herniating over the edge of the tentorium (*) compressing the mesencephalon against the free edge of the contralateral tentorium and causing a notch on the left side. Case courtesy of Erik Ranschaert, Radiopaedia.org, rID: 10967
Kernohan’s Notch (Optic)
Kernohan’s notch (optic) refers to a distinct pattern of indentation observed on the optic nerves or optic chiasm, produced by overlying arteries, particularly the anterior cerebral arteries, when these structures are displaced or compressed by pituitary tumors. This entity is pathologically distinct from the better-known Kernohan’s Notch phenomenon involving corticospinal tract compression and contralateral motor findings.
This refers to an indentation of the optic chiasm caused by pulsations from an adjacent arterial loop, often the internal carotid artery. Unlike the cerebral peduncle compression of KWNP, this optic variant is not associated with motor deficits. Instead, it reflects a chronic, pressure-related remodelling of the chiasm visible on imaging or autopsy, and serves as a subtle anatomical finding in neuro-ophthalmology.
1953 – Ophthalmologist C. Wilbur Rucker (1900-1991) and Kernohan described five cases in which suprasellar tumours (typically chromophobe adenomas) elevated the optic chiasm into the anterior vascular loop of the Circle of Willis. The anterior cerebral arteries, stretched taut by the tumour mass, created transverse grooves or “notches” across the optic chiasm or nerves, leading to characteristic field defects. Histological sections confirmed the notching correlated with myelin loss and optic atrophy in the affected regions.

Left: Case 1 – Large pituitary tumour. Passing transversely across the anterior portion of the chiasm is a notch cut by the anterior cerebral and communicating arteries.
Middle: Case 2 – Chiasmal region at authopsy.
Right Case 2 – removal of anterior cerebral arteries to reveal notching of the chiasm. Rucker and Kernohan 1953
The Rucker and Kernohan study offered systematic clinicopathological correlation using autopsy material, visual fields, and detailed anatomical mapping. Their work demonstrated that these arterial notches can mimic or contribute to bitemporal hemianopia and other visual deficits, particularly in late-stage pituitary tumours. This optic variant of Kernohan’s notch remains an important differential consideration in neuro-ophthalmology, although rarely emphasized in modern texts.
Key Medical Contributions
Tumour Classification
1949 – James W. Kernohan and colleagues R.F. Mabon, H.J. Svien, and A.W. Adson proposed a simplified classification of gliomas based on histological anaplasia, marking one of the earliest efforts to systematically grade brain tumors. Published in both Proceedings of the Staff Meetings of the Mayo Clinic and Surgical Clinics of North America, their work emphasised observable cytologic and architectural features such as nuclear pleomorphism, mitotic activity, cellularity, and vascular proliferation as markers of tumour aggression.
They introduced a four-grade scale:
- Grade 1: Well-differentiated, slow-growing tumors.
- Grade 2: Moderately cellular tumors with some atypia.
- Grade 3: Anaplastic gliomas with high mitotic activity.
- Grade 4: Glioblastomas with necrosis and microvascular proliferation.
Kernohan’s schema provided clinicians and surgeons with a practical framework for prognosis and treatment planning especially critical in an era before MRI or molecular diagnostics. The concept of grading based on anaplasia formed the basis of glioma classification for nearly five decades.
Evolution in WHO Classification
In 1979 The World Health Organization (WHO) began formalising glioma classification. The 2007 WHO system still retained much of Kernohan’s four-tiered model, with refinements based on immunohistochemistry and imaging. However, the landscape shifted dramatically with the 2016 and 2021 WHO updates, which integrated molecular markers such as IDH mutation status, 1p/19q co-deletion, and MGMT methylation into diagnostic categories.
While modern glioma taxonomy has moved toward genotype-based diagnosis, Kernohan’s emphasis on morphological grading persists as a complementary tool, especially in settings where molecular testing is unavailable. His work continues to be cited in historical reviews of glioma pathology and reflects the enduring impact of Mayo Clinic–based neuropathology in establishing standards of care.
Major Publications
- Kernohan JW, Woltman HW. Incisura of the Crus Due to Contralateral Brain Tumor, Proceedings of the staff meetings of the Mayo Clinic 1928; 3(10): 69-70
- Kernohan JW, Woltman HW. Incisura of the crus due to contralateral brain tumor. Archives of Neurology and Psychiatry 1929; 21(2): 274–287 [Kernohan-Woltman notch phenomenon]
- Kernohan JW, Mabon RF, Svien HJ, Adson AW. A simplified classification of the gliomas. Proceedings of the staff meetings of the Mayo Clinic. 1949 Feb 2;24(3):71-5.
- Svien HJ, Mabon RF, Kernohan JW, Adson AW. A simplified classification of the gliomas, based on the concept of anaplasia. Surg Clin North Am. 1949 Aug;29(4):1169-87.
- Rucker CW, Kernohan JW. Notching of the optic chiasm by overlying arteries in pituitary tumors. Trans Am Ophthalmol Soc. 1953;51:77-92. [Kernohan’s Notch (Optic)]
References
Biography
- Bailey OT. James W. Kernohan. J Neuropathol Exp Neurol. 1972 Jan;31(1):155-6.
- Sayre GP. In memoriam: James W. Kernohan, M.D. (1896-1981). J Neuropathol Exp Neurol. 1982 May;41(3):337-9.
- Dahlin DC. James Watson Kernohan: 1896-1981. Surg Neurol. 1984 Feb;21(2):107-9.
- Haines DE, Lancon JA, Zubkov AY. James Watson Kernohan (1896–1981). J Neurol 2005; 252, 1558–1559
- Etienne D, Zurada A, Matusz P, Shoja MM, Tubbs RS, Loukas M. James Watson Kernohan (1896–1981: Frontiers in neuropathology. Clin Anat. 2012 May;25(4):527-9.
- Berciano J, Gazulla J, Infante J. Haymaker and Kernohan’s Landry-Guillain-Barré syndrome paper: an essential contribution for accurate understanding of its early pathophysiology. Neurosciences and History 2025; 13(1): 48-70
Eponymous terms
- Adler DE, Milhorat TH. The tentorial notch: anatomical variation, morphometric analysis, and classification in 100 human autopsy cases. J Neurosurg. 2002 Jun;96(6):1103-12.
- Derakhshan I. Kernohan notch. J Neurosurg. 2004 Apr;100(4):741-2; author reply 742.
- Zafonte RD, Lee CY. Kernohan-Woltman notch phenomenon: an unusual cause of ipsilateral motor deficit. Arch Phys Med Rehabil. 1997 May;78(5):543-5
- Moon KS, Lee JK, Joo SP, Kim TS, Jung S, Kim JH, Kim SH, Kang SS. Kernohan’s notch phenomenon in chronic subdural hematoma: MRI findings. J Clin Neurosci. 2007 Oct;14(10):989-92.
- Derakhshan I. The Kernohan-Woltman phenomenon and laterality of motor control: fresh analysis of data in the article “Incisura of the crus due to contralateral brain tumor”. J Neurol Sci. 2009 Dec 15;287(1-2):296.
- Safavi-Abbasi S, Maurer AJ, Archer JB, Hanel RA, Sughrue ME, Theodore N, Preul MC. From the notch to a glioma grading system: the neurological contributions of James Watson Kernohan. Neurosurg Focus. 2014 Apr;36(4):E4.
- Derakhshan I. Letter to the Editor: Kernohan’s contributions to neurosurgery. Neurosurg Focus. 2014;37(4):E22
- Zhang CH, DeSouza RM, Kho JS, Vundavalli S, Critchley G. Kernohan-Woltman notch phenomenon: a review article. Br J Neurosurg. 2017 Apr;31(2):159-166.
- Carrasco-Moro R, Castro-Dufourny I, Martínez-San Millán JS, Cabañes-Martínez L, Pascual JM. Ipsilateral hemiparesis: the forgotten history of this paradoxical neurological sign. Neurosurg Focus. 2019 Sep 1;47(3):E7
- Laaidi A, Hmada S, Naja A, Lakhdar A. Kernohan Woltman notch phenomenon caused by subdural chronic hematoma: Systematic review and an illustrative case. Ann Med Surg (Lond). 2022 Jun 14;79:104006.
- Beucler N, Cungi PJ, Baucher G, Coze S, Dagain A, Roche PH. The Kernohan-Woltman Notch Phenomenon : A Systematic Review of Clinical and Radiologic Presentation, Surgical Management, and Functional Prognosis. J Korean Neurosurg Soc. 2022 Sep;65(5):652-664
- Carrasco-Moro R, Martínez-San Millán JS, Pascual JM. Beyond uncal herniation: An updated diagnostic reappraisal of ipsilateral hemiparesis and the Kernohan-Woltman notch phenomenon. Rev Neurol (Paris). 2023 Oct;179(8):844-865.
- Roy D, Chakravarty A. The Kinetics of Transtentorial Brain Herniation: Kernohan-Woltman Notch Phenomenon Revisited. Curr Neurol Neurosci Rep. 2023 Oct;23(10):571-580.
- Carrasco Moro R, Pascual Garvi JM, Vior Fernández C, Espinosa Rodríguez EE, Martín Palomeque G, Cabañes Martínez L, López Gutiérrez M, Acitores Cancela A, Barrero Ruiz E, Martínez San Millán JS. Kernohan-Woltman notch phenomenon: an exceptional neurological picture? Neurologia (Engl Ed). 2024 Oct;39(8):683-693.
- Negrão C, Silva MC, Machado M, Mourato M, Chumbo C, Tomás AR, Coutinho C, Monteiro AC, Matos C. Kernohan-Woltman Notch Phenomenon: A Case of Paradoxical Hemiparesis. Cureus. 2025 Jan 6;17(1):e76987.
Eponym
the person behind the name
BSc MD University of Western Australia. Interested in all things critical care and completing side quests along the way
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | On Call: Principles and Protocol 4e| Eponyms | Books |

