Manfred Sakel
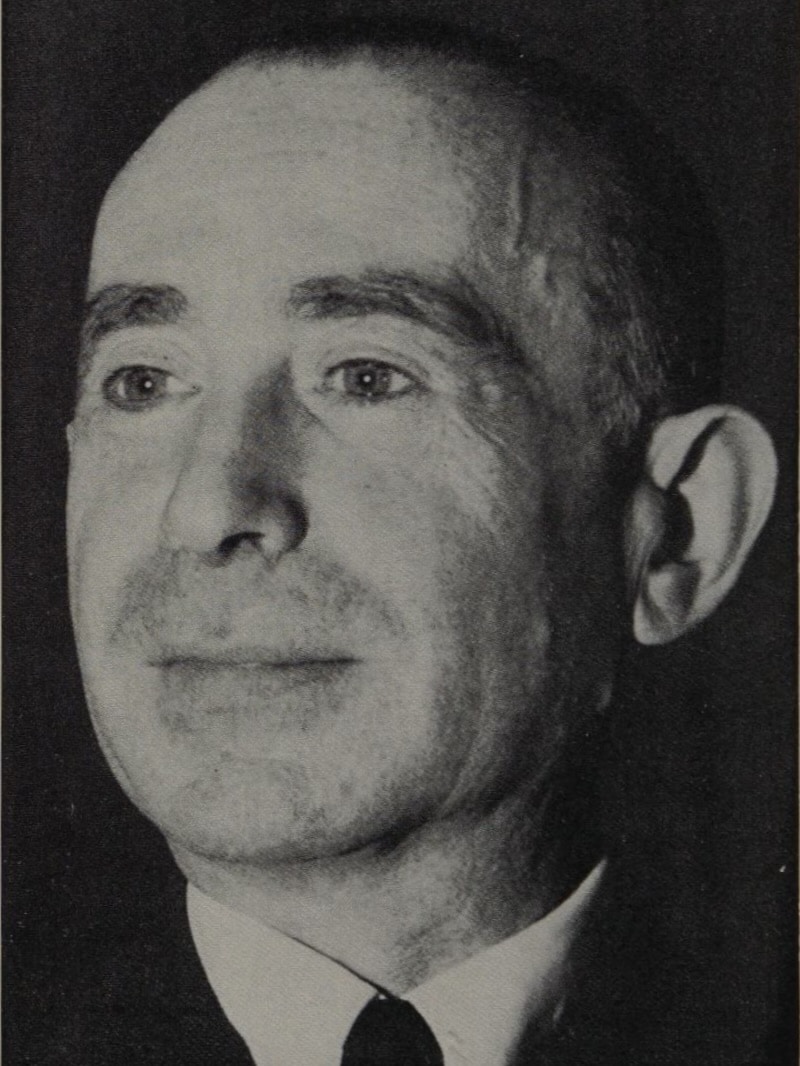
Manfred Joshua Sakel (1900-1957) was an Austrian neuropsychiatrist
Sakel developed Insulin Coma Therapy (ICT) in the 1930s, one of the earliest biological treatments for schizophrenia. Working in Vienna and Berlin, Sakel theorised that psychosis could be interrupted or reversed through controlled metabolic shock. His clinical observations of improved lucidity in patients undergoing insulin-induced hypoglycaemia shaped a somatic paradigm that would influence psychiatry for decades.
After emigrating to the United States in 1936 to escape antisemitism, Sakel continued to promote ICT at Harlem Valley State Hospital and in international lectures. His method was time-intensive and not without significant risk yet was widely adopted throughout the 1930s and 1940s, becoming a standard treatment in psychiatric institutions. ICT also helped to legitimise the broader field of biological psychiatry, laying conceptual groundwork for electroconvulsive therapy and psychopharmacology.
By the 1950s, ICT had fallen out of favour. The lack of controlled trials, inconsistent outcomes, high mortality (up to 2%), and logistical demands contributed to its decline. Sakel remained respected in psychiatric circles but watched his therapy become obsolete with the rise of antipsychotic medications and more refined neurobiological models. His legacy endures as a controversial but pivotal figure in the evolution of modern psychiatry.
Biographical Timeline
- Born on June 6, 1900 in Nadvirna (then Austria-Hungary, now Ukraine) into a Jewish family.
- 1920 – Completed education at the First State College of Brno, Czechoslovakia.
- 1925 – Graduated MD from the University of Vienna.
- 1927–1933 – Chief physician at the private psychiatric Lichterfelde Hospital, Berlin. Developed interest in abstinence cures and began using insulin for morphine withdrawal, noting parallels with hyperthyroidism and the the calming effects of induced hypoglycaemia
- Early 1930s – Initiated crude animal experiments on insulin shock in his kitchen. Began applying insulin-induced hypoglycaemic comas to treat psychotic excitement, particularly schizophrenia.
- 1933 – Returned to Vienna as volunteer assistant at the university psychiatric service to collaborate with Prof. Otto Pötzl and formally develop insulin coma therapy (ICT).
- 1935 – Published early results of ICT; Prof. Pötzl and others endorse method.
- 1936 – Honoured with a degree from Colgate University. Emigrates to the United States following an invitation from Dr. Frederick Parsons; begins working at Harlem Valley State Hospital, NY.
- 1937 – ICT gains international recognition and is adopted in Switzerland (Müller), the U.S. (Cameron), Poland (Frostig), and Hungary (Benedek).
- 1937–1940s – Widely sought speaker; his technique evaluated by U.S. mental health commissions (notably praised in a 1944 TIME article for reducing hospital stays and increasing remission rates in schizophrenia).
- 1940s – IST used extensively worldwide, though controversial; later overtaken by electroconvulsive therapy (ECT) due to safety and efficacy.
- 1946 – Suffered a near-fatal heart attack; began withdrawing from public scientific life and focused on private practice.
- 1950s – Lived simply, continued charitable work, and planned to build a hospital.
- Died on December 2, 1957 of a sudden heart attack in New York City.
Medical Eponyms
Insulin Coma Therapy (ICT)
In the early 1930s, Sakel observed that small doses of insulin calmed agitated opioid addicts. When extended to psychotic patients, deeper insulin-induced hypoglycaemic states seemed to improve their mental clarity. He hypothesized this “shock” state could reset the diseased brain, a prevailing belief in early biological psychiatry.
The coma itself seems to break through the pathological processes of schizophrenia… the patient awakens with a changed state of consciousness, in many cases with striking improvement
Sakel 1935
Sakel first reported this in Wiener klinische Wochenschrift (1933) and refined the protocol in subsequent writings, culminating in his 1935 monograph Neue Behandlungsmethode der Schizophrenie. ICT quickly gained attention as a somatic intervention during a time when psychiatry sought physiological treatments to legitimise the field.
Clinical Theory of Shock Therapy
Sakel proposed that schizophrenia was the result of a toxic or dysfunctional brain state that could be “rebalanced” through metabolic shock. ICT aimed to simulate a life-threatening crisis, pushing the body into survival mode, which was believed to realign neural circuits.
Sakel proposed that the shock of hypoglycaemia induced a reorganisation of brain function, temporarily disrupting pathological neural circuits. He believed that by artificially producing a life-threatening state and then reversing it, the brain was physiologically “reset,” leading to psychic reorganisation. This fit within the broader “shock therapy” movement alongside fever therapy (Wagner-Jauregg) and chemical convulsion therapy (Meduna), embracing biological mechanisms for psychiatric disease.
Mechanism, Practice, and Outcomes
Insulin was administered in escalating doses to induce hypoglycaemia and coma. After 20–30 minutes, patients were revived with glucose. A full course involved 30–50 sessions. Outcomes were reported as:
- ~70% improvement rate (according to early proponents).
- Later assessments showed mixed efficacy, especially in chronic schizophrenia.
- Risks: mortality 0.5–2%, seizures, brain damage, prolonged hospitalisation.
ICT involved administering increasing doses of insulin to induce hypoglycaemia and coma. Comas were maintained for up to an hour and reversed using glucose. Treatment was delivered in prolonged courses, sometimes involving 20 to 50 sessions. Sakel reported up to 70–88% improvement in early-stage schizophrenia, although these figures were not universally replicated. Mortality ranged from 0.5% to 2%, primarily due to irreversible coma or complications. Despite risks, ICT became the gold standard for schizophrenia in the late 1930s and early 1940s, especially in Europe and the United States.
Controversy, Criticism, and Decline
From the 1940s onwards, doubts grew regarding the safety, efficacy, and scientific rationale of ICT. Studies failed to confirm long-term superiority over other treatments, and the intensive nursing demands and risk of fatal hypoglycaemia prompted criticism. The arrival of electroconvulsive therapy (ECT), pioneered by Cerletti and Bini in 1938, offered a quicker, safer, and less resource-intensive alternative.
By the 1950s, insulin coma therapy was largely replaced by ECT and, later, antipsychotic medications such as chlorpromazine. Sakel remained a strong proponent of ICT until his death in 1957, but by then, the method was rapidly vanishing from clinical use.
Major Publications
- Sakel M. Neue Behandlung der Morphinsucht. Deutsche medizinische Wochenschrift 1930; 1930; 56(42): 1777-1778
- Sakel M. Neue Behandlungsart Schizophreniker und verwirrter Erregter. Wiener klinische Wochenschrift. 1933; 46: 1372–1373.
- Sakel M. Schizophreniebehandlung mittels Insulin-Hypoglykamie sowie hypoglykamischer Shocks, Wiener Medizinische Wochenschrift 1934; 84: 1326-1327
- Sakel M. Neue Behandlungsmethode der Schizophrenie. 1935
- Sakel M. The pharmacological shock treatment of schizophrenia. 1938
- Sakel, M. Über die Einführung der sog. Schocktherapie und Poützl’s Verdienst um ihre Einführung. In: Urban, HJ., editor. Festschrift zum 70. Geburtstag von Prof. Dr. Otto Pötzl. Innsbruck, Austria: Tirol Graphik; 1947. p. 403-407.
- Sakel M. Schizophrenia. 1958 [Published posthumously]
- Sakel M. Epilepsy. 1958 [Published posthumously]
References
Biography
- DR. SAKEL IS DEAD; PSYCHIATRIST, 57; Originator of Insulin Shock Therapy for Schizophrenia –Had Treated Nijinsky. NYT December 3, 1957
- Manfred Sakel MD Vienna. Lancet. 1957; 270(7007): 1235
- Manfred Sakel. Br Med J. 1957 Dec 14;2(5058):1439–40.
- Manfred Sakel, M. D., 1900-1957. American Journal of Psychiatry, 1958; 115(3): 287-288
- Kolle K. Manfred Sakel. Dtsch Med Wochenschr. 1958 Feb 14;83(7):266.
Eponymous terms
- Frostig JP, Wortis J. Sakel’s pharmacologic shock treatment for schizophrenia: tentative directions and system of recording. Arch NeurPsych. 1938;39(2):219–231.
- KATZENELBOGEN S, ALEXANDER SIMON, ANNA R. COYNE, et al. PHARMACOLOGICAL TREATMENT IN SCHIZOPHRENIC PATIENTS. Ann Intern Med. 1940; 14: 393-405.
- Fink M. Meduna and the origins of convulsive therapy. Am J Psychiatry. 1984 Sep;141(9):1034-41.
- Peters UH. Die Einführung der Schockbehandlungen und die psychiatrische Emigration [Introduction of shock therapy and psychiatric emigration]. Fortschr Neurol Psychiatr. 1992 Sep;60(9):356-65.
- Shorter E. Sakel versus Meduna: different strokes, different styles of scientific discovery. J ECT. 2009 Mar;25(1):12-4.
- Gazdag G, Ungvari GS, Czech H. Mass killing under the guise of ECT: the darkest chapter in the history of biological psychiatry. Hist Psychiatry. 2017 Dec;28(4):482-488.
- Sabbatini RME. The History of Shock Therapy in Psychiatry. Cerebromente
Eponym
the person behind the name
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | On Call: Principles and Protocol 4e| Eponyms | Books |
