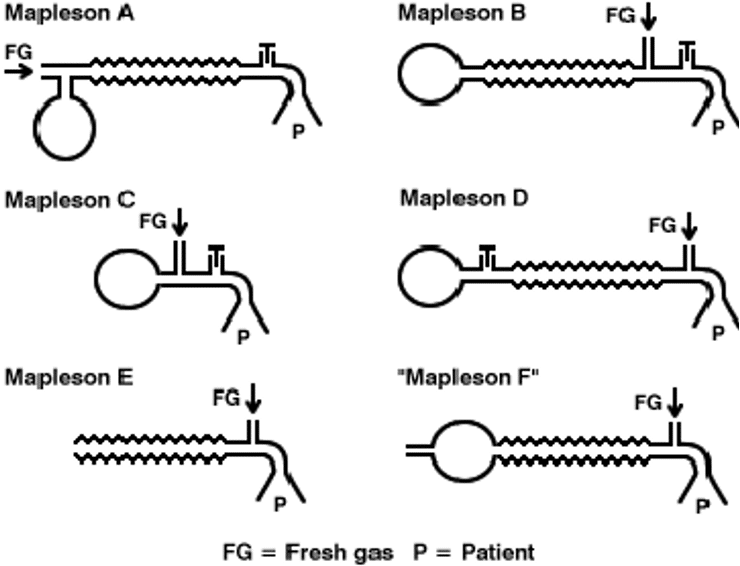
Mapleson Circuit
Description
The Mapleson Circuit Systems are used for the delivery of oxygen and anaesthetic agents and the removal of carbon dioxide during general anaesthesia.
Components include breathing tube, adjustable pressure limiting valve, reservoir bag, fresh gas flow and patient connection.
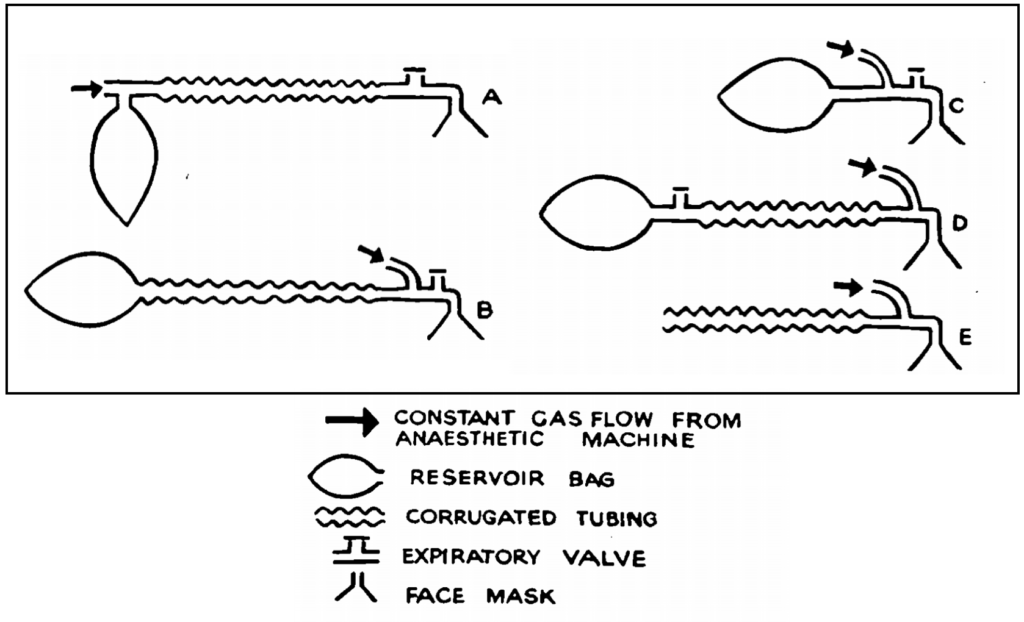
In 1954, William Wellesley Mapleson (1926 – 2018) described five breathing circuits: A, B, C, D and E. A 6th circuit ‘the Jackson Rees modification of Ayre’s T-piece (F)‘ was later added in a paper by Willis, Pender and Mapleson in 1975.
Each circuit has functional benefits in various situations. For example the Mapleson A is the circuit of choice for spontaneous respiration in adults; the Mapleson D best for controlled ventilation; whilst the Mapleson E and F are most suited for neonates and paediatric patients.
History of the Mapleson Circuit Systems
1954 – Mapleson’s landmark paper classified anaesthetic breathing circuits and gave rise to the nomenclature of Mapleson circuits A, B, C, D and E. This classic paper was initially regarded as a minor theoretical study by Mapleson who was awaiting volunteers for another neuromuscular relaxant study.
1975 – Willis, Pender and Mapleson described the Mapleson F, a modification of Mapleson E using the Jackson Rees modification of Ayres T-Piece during spontaneous respiration.
MAPLESON A (also Magill system)
- Fresh gas flow enters near the reservoir bag at the machine end and the expiratory valve is positioned at the patient end
- The patient inhales fresh gas and the valve is closed during inspiration
- When the patient exhales, expired gas flows through the tubing and into the reservoir bag until the bag fills and the resultant pressure causes the expiratory valve to open
- The expired air is vented into the atmosphere which is further ‘pushed’ by the continuous fresh gas flow during the expiratory pause
- This minimises rebreathing of expired air
- This circuit functions best when the fresh gas flow equals the minute ventilation and dead space gas (free of CO2 as does not take part in gas exchange) is allowed to be rebreathed
- It is the best circuit for the spontaneous breathing patient because of minimal rebreathing
- Main disadvantages include the proximity of the valve to the patient which makes it largely inaccessible during surgery and its constant evacuation of gases into the theatre environment
- Lacks modification added an expiratory limb which facilitated the scavenging of gas to prevent theatre pollution
MAPLESON B and C
- These are similar circuits with the fresh gas flow and expiratory valve located at the patient end and the reservoir bag at the machine end
- The corrugated tubing is absent in Mapleson C; it is a ‘shortened’ version of Mapleson B
- Fresh gas flows and fills the reservoir bag and tubing.
- The patient inhales the fresh gas and expires into the reservoir tubing. During the expiratory pause, the fresh gas flow continues to fill the bag which now also contains the expired gas and as the pressure within the bag rises, the expiratory valve opens and these are vented into the atmosphere
- When the patient takes the next breath, it is both of mixed and fresh gas
- Fresh gas flow must be equal to peak inspiratory flow rate to prevent rebreathing as such, both these circuits require high gas flow and produce high theatre pollution
MAPLESON D
- Fresh gas flows from the machine end and connects to an Ayre T-piece at the patient end
- The T-piece has an extra limb of corrugated tubing which connects to the reservoir bag and the expiratory valve
- Patient inhales gas from the tubing and fresh gas flow
- Expired gas fills the tubing and fresh gas flow pushes this expired gas into the bag inflating it
- When the bag is sufficiently distended, the pressure causes the APL valve to open and the gas is vented into the atmosphere
- FGF needs to be 2-3 times the minute volume to prevent rebreathing
- The Bain modification of this circuit includes a ‘tube within a tube’
- Fresh gas flows in a tube that runs coaxially inside the corrugated tubing to the patient
- When the patient exhales, the expired air flows back into the corrugated tubing and into the reservoir bag
- When the bag is full, the valve opens and excess gas is vented into the atmosphere
- During the expiratory pause, fresh gas flow continues and fills the proximal portion of the corrugated tube. This “pushes” the expired gas up the tube and into the bag
- On the next breath, the patient breaths fresh gas and the mixed gas in the corrugated tube
- If the fresh gas flow rate is high (1.5-2x minute volume) then the patient will inspire only fresh gas from the corrugated tube
- This is the most efficient system for controlled ventilation
MAPLESON E
- Derived from the Ayre T-piece used in Mapleson D circuit and functions on the same principle as Mapleson D
- The primary difference is in the length of the tubing that is increased to be greater than the patient’s tidal volume
- For spontaneous ventilation, the expiratory limb is open to the atmosphere
- It has no valves so there is no resistance to airflow nor points for possible mechanical failure
- Rebreathing is dependent on the fresh gas flow, patients minute volume and capacity of the expiratory limb
- Its main use is in paediatric patients
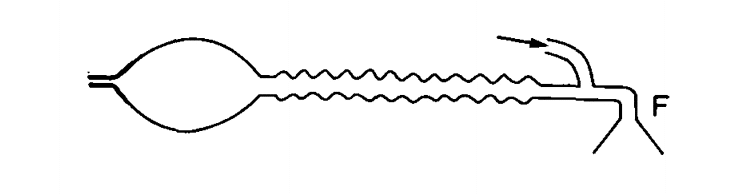
MAPLESON F
- Jackson Rees modification of the Mapleson E system
- A 500ml bag is attached to the expiratory limb. A hole in the tail can be occluded by a finger to direct gas flow to the patients’ lungs and provide pressure in controlled ventilation. The elasticity of the bag provides a ‘pressure buffering effect’ and prevents barotrauma; a problem often seen in Mapleson E due to overinflation
- The bag can also be fitted with a PEEP valve and converts the valveless system into one with a valve
- Observation of the bag during spontaneous ventilation helps in assessing and monitoring respiration.
- The system functions similar to a Mapleson E albeit with the added bag on the expiratory limb
- Fresh gas and expired gas mix in the bag during expiration
- FGF pushes the expired gas down the limb and into the bag during expiratory pause
- During the next inspiration, fresh gas is inhaled both from the FGF and from the expiratory limb of the circuit (now replaced with fresh gas)
- High fresh gas flows are required to prevent rebreathing (2.5-3x minute volume)
- Gases are vented into the atmosphere; scavenging is not possible
Associated Persons
- William Wellesley Mapleson (1926 – 2018)
- Thomas Philip Ayre (1901 – 1979)
- Gordon Jackson Rees (1918 – 2001)
Alternative names
- Mapleson Circuits
- Mapleson Breathing Circuits
References
Historical references
- Mapleson WW. The elimination of rebreathing in various semi-closed anaesthetic systems. Br J Anaesth. 1954; 26(5): 323-332 [reprint Br J Anaesth. 1998; 80(2): 263-269.]
- Mapleson WW. Theoretical considerations of the effects of rebreathing in two semi-closed anaesthetic systems. Br Med Bull. 1958; 14(1): 64-68.
- Willis BA, Pender JW, Mapleson WW. Rebreathing in a T-piece: volunteer and theoretical studies of the Jackson Rees modification of Ayre’s T-piece during spontaneous respiration. Br J Anaesth. 1975; 47(12): 1239-1246.
Eponymous term review
- Kaul TK, Mittal G. Mapleson’s Breathing Systems. Indian J Anaesth. 2013; 57(5): 507-515.
eponymictionary
the names behind the name
Emergency registrar at Sir Charles Gairdner Hospital, Perth


Hi from the past!
How its possible for the Mapleson E circuit to have overinflation if there is no reservoir or APL valve? Unless there is such a high FGF that it exceeds the escape capacity of the corrugate tube.
why can’t the “used” air be scanvenged from the opening at the bag in the Mapleson F?
Thank you very much!
Hi
This excerpt from Kaul & Mittal (2013) explains it:
Barotrauma can occur during controlled ventilation in Mapleson E, due to overinflation. This is because anaesthetist does not have the feel of the bag during inflation. Pressure buffering effect of the bag is absent. This problem is not seen with Mapleson F as there is a bag in the system.
https://europepmc.org/article/PMC/PMC3821268
Cheers
Chris