Medical education challenge
Medical education challenge: teaching small groups of diverse learners
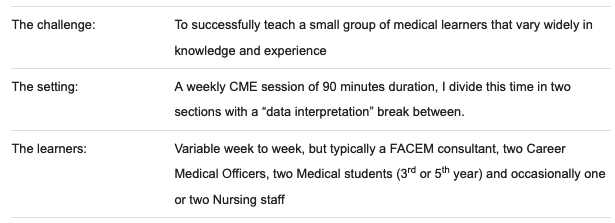
Medical education both undergraduate and postgraduate mostly takes place in small group settings with less than 20 learners, and those of us who teach regularly become comfortable in this setting and proficient in the techniques and skills to make it effective. There is a large education evidence base in a range of disciplines that supports this learning format and it’s popular with learners. Over the last decade, most of my medical teaching has been in small groups and focused on two areas, guiding ACEM trainees to completion of their emergency physician training, and coordination of Continuing Medical Education sessions for medical staff in a large tertiary urban ED. These were both very homogeneous groups of learners – all medical, all on a similar career path to ACEM Fellowship and most from a first world medical training background in either Australia or the UK.
But my career move to a smaller private urban ED earlier this year has presented several new challenges, one of which I want to discuss here with a view to my approach so far, and to seek contributions from readers who may have other better techniques.
This challenge is commonly encountered in interprofessional teaching and I’ll just elaborate some of the education considerations when planning the session. To some degree it must always be a compromise compared with presenting material to learners at the same level, but there are some unique benefits too.
- Inclusiveness for all participants, aiming to value input from all levels of learner, and to minimise barriers to them making contributions.
- Good topic selection, to optimise suitability and relevance as there are widely varying ages, experience and endpoints of learners
- Flexibility in teaching methods to accommodate a range of learning styles
- Careful content and pace considerations, to try and achieve balance with new / known and simple / complex material.
I’ve found very little published data on planning and conducting sessions in this area of medical education although I believe it to be a challenge for many of us. An article by Certain et al in 2011 is a well-written review in the clinical setting of ward rounds but in the slightly less dynamic setting of a CME session, I’ve found the following to be most useful and successful so far.
- Case-based studies, where we dissect a patient presentation in terms of diagnosis, clinical reasoning, investigation strategies and outcomes. These can be selected to highlight a serious or rare presentation, or explore in detail a common less acute one, with questions pitched at different levels. They might have a predominant focus on the treatment or investigation as a key theme. In these I try to encourage the learners to be their own teachers, so my role becomes more facilitator than educator. “Why?” and “How?” questions work well here as they encourage flow of questions and exchange of experience. Medical students who have most recently done basic medical sciences can often provide that underpinning to discussions, where more advanced learners provide detail around their knowledge and accumulated experiential wisdom.
- FOAM, Free Online Access to Meducation, is a great way to add some “colour and oomph” to CME by using some content from the rapidly expanding online community of international educators within your session – multiple ways to do this including video, images, powerpoints etc. We’re just at the beginning of knowing how best to incorporate these but I regularly use material from LITFL and many others that have content applicable to all stages of learner. Its a great way to achieve high quality education when you have limited time for lesson preparation, and there’s the huge bonus of showing your students how and where to go exploring for themselves in their own time.
- Investigation analysis, always popular and relevant, and a key component of most sessions I teach. It can be as simple as ECG or blood gas interpretation or as organised as a Radiology review hour. Questions can be targeted at multiple levels to both establish adequate basic background understanding through to high end and emerging concepts. (so if we take a blood gas as an example, might explore basic approach first, then touch on HH equation and strong iron difference for higher level learners…)
- Procedure and Equipment reviews, wherein we explore both standard and evolving techniques and technology. In regard to the latter, younger students are often better equipped to contribute, and are vital in demonstrating to older learners how to incorporate new techniques into their education and practice. Role play and simulation are great for learning about equipment, helping to break down barriers between learners and fostering more cohesive and functional teams
- Journal club, discussion of evidence, and the techniques/pitfalls in its interpretation. These can be great to teach initially how to find and assess/use data, then building to review new and important articles, and to talk around implementation of emerging practices, guidelines and recommendations.
For now I think this is working in my setting, but I’m going to throw it to you and await your tips and tricks! Hopefully you’ll have some other exciting techniques to share.
emergency physician keen on medical education and cycling

Thanks Trevor, those are some great tips!