Meigs syndrome
Meigs syndrome is a rare, benign clinical triad defined by the presence of ascites, pleural effusion (typically right-sided), and a benign ovarian tumour (most commonly a fibroma, thecoma, or Brenner tumour) with complete resolution of the fluid collections following tumour resection.
First systematically characterised by American gynaecologist Joe Vincent Meigs in the 1930s, the syndrome has remained a key differential in the evaluation of suspected ovarian malignancy with serosal effusions.
Typically affecting postmenopausal women, Meigs syndrome presents with symptoms related to fluid accumulation: abdominal distension, early satiety, dyspnoea, or dry cough. On imaging, the findings may mimic advanced ovarian carcinoma, especially when elevated serum CA-125 is present, a known but misleading feature in this condition. Diagnostic confirmation is retrospective, made after histologic confirmation of a benign tumour and resolution of ascites and hydrothorax.
Variants include:
- Nonclassic Meigs syndrome: where the tumor is benign but not of the fibroma-like subtype (e.g., serous cystadenoma)
- Pseudo-Meigs syndrome: where a malignant pelvic tumor is present
- Incomplete or atypical Meigs syndrome: where either ascites or hydrothorax is absent
- Demons–Meigs syndrome: sometimes used synonymously, in recognition of earlier descriptions by French gynaecologist Albert Demons
Meigs syndrome is rare, comprising about 1% of surgically resected ovarian tumors. Awareness of the diagnosis is crucial in avoiding overtreatment and recognising potentially curable pathology masquerading as disseminated malignancy.
History of Meigs syndrome
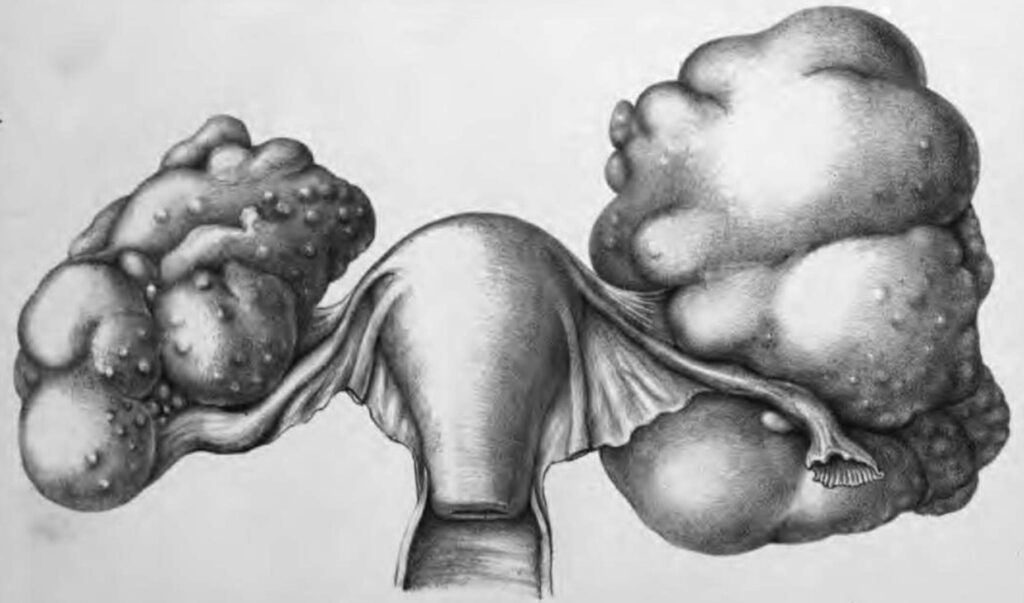
1866 – German gynaecologist Otto von Spiegelberg (1830-1881) first described a patient with fibroma, ascites and hydrothorax. Spiegelberg described a case of “Fibrom des Eierstockes von enormer Größe” (fibroma of the ovary of enormous size) in Monatsschrift für Geburtskunde und Frauenkrankheiten
1879 – Charles James Cullingworth (1841-1908) described a case of a 36 year-old woman with fibroma of both ovaries, ascites and a left pleural effusion who died from respiratory collapse. Autopsy confirmed bilateral ovarian fibromas and a large quantity of fluid in the peritoneal cavity and the left pleural cavity.
1887 – French gynaecologist Albert Jean Octave Demons (1842 – 1920) published on pleural effusions complicating ovarian cysts in Épanchements pleurétiques compliquant les kystes de l’ovaire. He noted that among 50 women with ovarian cysts, nine (≈18 %) had ascites and hydrothorax that resolved after cyst removal, the first recognition of the postoperative resolution of the fluid collection.
1888 – Giovanni Pascale (1859-1836) described ascites and associated hydrothorax in 3 of 21 patients with ovarian cysts. Following puncture of the cyst the fluid initially disappeared but returned. However, he noted that removal of the cyst caused permanent resolution of ascites and hydrothorax.
1900-1903 Demons published additional reports and commentaries in the Revue mensuelle de gynécologie, obstétrique, et pédiatrie de Bordeaux, further supporting the concept that pleural and peritoneal effusions secondary to benign ovarian tumours were cured by tumour excision. Although he never systematised these cases into a formal syndrome
1934 – American obstetrician/gynaecologist Joe Vincent Meigs (1892-1963) first referenced the condition of ovarian fibroma with ascites and hydrothorax describing three cases in his book Tumors of the Female Pelvic Organ.
Three patients with large cellular tumors had been in the medical ward, where because of fluid in the chest a diagnosis of tuberculosis had been made and their chests tapped. Paracentesis had been done more than three times in each case…An abdominal tumor was finally discovered and operation advised. A fibroma was found in each instance with fluid in the abdomen ; the tumor was removed and the patient promptly recovered.
Meigs 1934
1937 – Meigs and John W. Cass published a more detailed clinical series in Fibroma of the Ovary with Ascites and Hydrothorax, reporting seven cases of ovarian fibromas accompanied by ascites and hydrothorax. This was the first formal articulation of the syndrome as a distinct clinical entity.
A pelvic tumor, ascites, and hydrothorax occurred together in all seven cases…In each case the operative removal of the ovarian fibroma was followed by prompt and complete disappearance of both the abdominal and the thoracic fluids.
Meigs, Cass 1937
1937 – Jonathan E. Rhoads (1907–2002) and Alexander W. Terrell reviewed the global literature and coined the eponymous term Meigs’ syndrome in their article Ovarian fibroma with ascites and hydrothorax (Meigs’ syndrome)
1940s – The eponym “Meigs’ syndrome” came into generalised clinical usage with retrospective attribution to Meigs’ 1937 series. However, earlier related descriptions exist (e.g., Demons and Lemoine in 1902), and some authors distinguish Demons–Meigs syndrome to reflect this broader historical lineage.
1954 – Meigs formalises the triad and diagnostic criteria in his article Fibroma of the ovary with ascites and hydrothorax – Meigs’ syndrome and acknowledges historical timeline.
Classification Refinements (Post-2000)
Classic Meigs Syndrome
The original triad with resolution of effusions after tumour resection is required for diagnosis.
- Benign solid ovarian tumor (typically fibroma, thecoma, or Brenner tumor)
- Ascites
- Pleural effusion (commonly right-sided)
Incomplete / Atypical Meigs Syndrome
A benign pelvic tumour with either ascites or pleural effusion, but not both. Pleural effusion without ascites is especially rare but documented; these cases typically involve right-sided hydrothorax and are retrospectively diagnosed after resolution post-surgery.
Nonclassic Meigs Syndrome
Benign ovarian or pelvic tumours other than fibromas. These tumours still meet the resolution criterion but differ histologically from classic fibromas.
- Serous cystadenoma
- Mucinous cystadenoma
- Brenner tumor
- Granulosa cell tumour
Pseudo-Meigs Syndrome
Presentation mimics Meigs syndrome (ascites + pleural effusion + pelvic mass) but the underlying tumor is malignant, such as:
- Ovarian carcinoma
- Gastrointestinal or metastatic tumours involving the ovary
- Uterine leiomyoma (rare)
This entity is significant due to poor prognosis and the absence of fluid resolution post-surgery.
Demons–Meigs Syndrome
Used predominantly in French and Russian literature to credit Albert Demons alongside Joe Vincent Meigs. Funck-Brentano (1948) advocated renaming it to honour Demons
Associated Persons
- Otto von Spiegelberg (1830-1881)
- Charles James Cullingworth (1841-1908)
- Albert Jean Octave Demons (1842 – 1920)
- Joe Vincent Meigs (1892-1963)
References
Historical references
- Spiegelberg O. Fibrom des Eierstockes von Enormer Grösse. Monatsschrift für Geburtskunde und Frauenkrankheiten. 1866; 28:415-425.
- Cullingworth CJ. Fibroma of both ovaries. Transactions of the Obstetrical Society of London. 1880; 21:276-288
- Demons A. Épanchements pleurétiques compliquant les kystes de l’ovaire. Bulletins et mémoires de la société de chirurgie de Paris 1887;13:771–776
- Pascale G. L’idrotorace nelle cisti dell’ovaio. Archivio ed Atti della Società italiana di chirurgia. 1888; 5: 291
- Tait RL. On the occurrence of pleural effusion in association with disease of the abdomen. Medico-Chirurgical Transactions 1892; 75:109–118.
- Demons A. Discussion of Rocher. M. Louis. Revue mensuelle de gynécologie, obstétrique et pædiatrie de Bordeaux. 1900; 2: 274.
- Demons A. Sur un point de l’evolution clinique des fibromes de l’ovaire et les ligaments larges. Quinzième congrès de chirurgie, París: procés-verbaux, mémoires et discussions 1902; 1: 739– 40.
- Demons A. Revue mensuelle de gynécologie, obstétrique et pædiatrie de Bordeaux. 1903; 5: 184.
- Hoon MR. Fibroma of the ovary. Surg Gynecol Obstet 1923;36:247.
- Meigs JV, Cass JW Fibroma of the ovary with ascites and hydrothorax, with a report of seven cases. American Journal of Obstetrics and Gynecology 1937; 33: 249-267.
- Meigs JV, Cass JW. Fibroma of the ovary with ascites and hydrothorax, with a report of seven cases. American Journal of Obstetrics and Gynecology 1937; 33: 249-267.
- Rhodes JE, Terrell AW. Ovarian fibroma with ascites and hydrothorax (Meigs’ syndrome). Journal of the American Medical Association 1937; 109: 1684–1687.
- Funck-Brentano P. Comptes rendus de la Société française de gynécologie. 1948; 18: 178
- Meigs JV. Fibroma of the ovary with ascites and hydrothorax – Meigs’ syndrome. American Journal of Obstetrics and Gynecology. 1954; 67: 962-987
Additional references
- Lawlor MK. Meigs’ Syndrome. Proc R Soc Med. 1944 Jun;37(8):430.
- Clay AC, Johnston RN, Samson L. Meigs’s Syndrome. Br Med J. 1944 Jul 22;2(4359):113-4.
- Lurie S. Meigs’ syndrome: the history of the eponym. Eur J Obstet Gynecol Reprod Biol. 2000; 92(2): 199-204.
- Morán-Mendoza A, Alvarado-Luna G, Calderillo-Ruiz G, Serrano-Olvera A, López-Graniel CM, Gallardo-Rincón D. Elevated CA125 level associated with Meigs’ syndrome: case report and review of the literature. Int J Gynecol Cancer. 2006 Jan-Feb;16 Suppl 1:315-8.
- Lanitis S, Sivakumar S, Behranwala K, Zacharakis E, Al Mufti R, Hadjiminas DJ. A case of Meigs syndrome mimicking metastatic breast carcinoma. World J Surg Oncol. 2009 Jan 22;7:10.
- Krenke R, Maskey-Warzechowska M, Korczynski P, Zielinska-Krawczyk M, Klimiuk J, Chazan R, Light RW. Pleural Effusion in Meigs’ Syndrome-Transudate or Exudate?: Systematic Review of the Literature. Medicine (Baltimore). 2015 Dec;94(49):e2114
- Oncological Quandary 004 – Pulmonary Re-expansion. LITFL
Eponym
the person behind the name
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | On Call: Principles and Protocol 4e| Eponyms | Books |
