Obstetric Bleeder
aka Ob-Gyn Obfuscation 001
A 32 year-old woman is referred to the ICU post caesarean section. She had an uneventful elective caesarian section 10 hours previously.
She has been referred because in the last 2 hours she has developed vaginal bleeding and oozing from her epidural site. Her vital signs are unremarkable except for a small oxygen requirement.
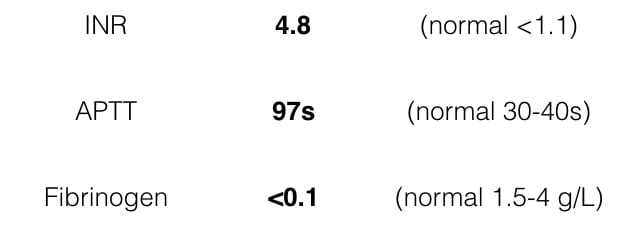
The following coagulation results are obtained:
Questions
Q1. Describe the results.
Answer and interpretation
- The INR is high, the APPT is high and the fibrinogen is very low.
- These results are consistent with disseminated intravascular coagulation (DIC).
Q2. What abnormality would you expect to see on a blood film?
Answer and interpretation
- In severe DIC there are fragmented red blood cells (schistocytes).
Q3. What is the differential diagnosis?
Answer and interpretation
In this case, potential pregnancy-related causes of DIC include:
- amniotic fluid embolism
- >pre-eclampsia
- HELLP syndrome
- post-partum haemorrhage
The fact that bleeding did not occur at the time of the caesarian section suggests that the problem has developed subsequently making amniotic fluid embolism the most likely diagnosis.
Other pregnancy-related causes of DIC (not relevant here) include:
- placental abruption
- septic abortion
- intrauterine death
The most important non-pregnancy related cause of DIC is:
- severe sepsis
Q4. How would you treat this coagulopathy?
Answer and interpretation
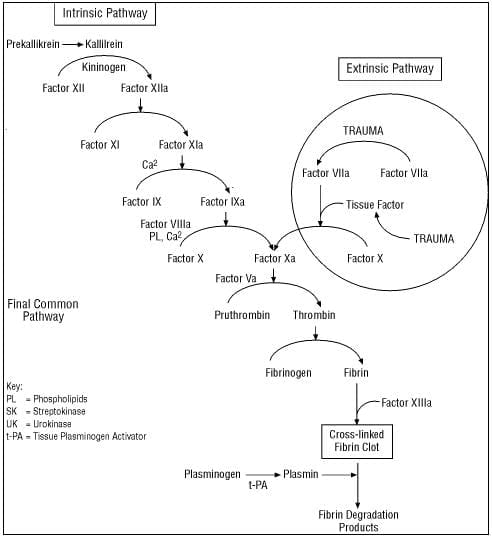
It turns out that knowing one thing about the coagulation cascade is useful:
- That one thing is that conversion of fibrinogen to fibrin is at the bottom of the cascade.
- That means that if the fibrinogen is low, the patient will not form clot until they get cryoprecipitate.
- Any patient with a coagulopathy who has a low fibrinogen should have their fibrinogen corrected as the first priority.
- The usual dose of cryoprecipitate is one unit of cryoprecipitate per 30 kg of body weight.
- In this case, the fibrinogen level is exceptionally low and administration of a greater dose than this would be appropriate.
- The patient should also receive fresh frozen plasma and may require platelets (depending on the platelet count).
References
- Bick RL. Syndromes of disseminated intravascular coagulation in obstetrics, pregnancy, and gynecology. Objective criteria for diagnosis and management. Hematol Oncol Clin North Am. 2000 Oct;14(5):999-1044. PMID: 11005032

CLINICAL CASES
Ob-Gyn Obfuscation
Intensivist in Wellington, New Zealand. Started out in ED, but now feels physically ill whenever he steps foot on the front line. Clinical researcher, kite-surfer | @DogICUma |