Paracetamol-Induced Hepatotoxicity
aka Toxicology Conundrum 045
A 49-year old lady weighing only 40kg presents to a rural Australian ED approximately 10 hours after ingesting 10-12g of paracetamol (250-300mg/kg) with suicidal intent. The nearest tertiary hospital is 1600km away and aeromedical retrieval (if required) will take several hours to organise. Blood tests and N-acetylcysteine (NAC) are available.
Questions
Q1. How should this patient initially be investigated and managed?
Answer and interpretation
She has presented at >8 hours with an ingestion of >200 mg/kg, so NAC should be started on arrival.
- Bloods should be sent for ALT and paracetamol level.
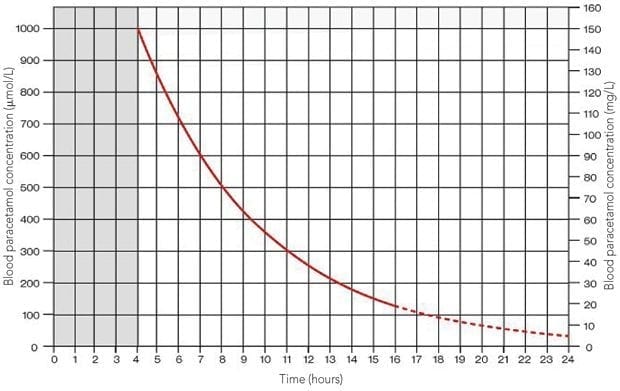
- The paracetamol level should be plotted on the nomogram (below).
- The need for ongoing NAC is determined by the timed paracetamol level.
The NAC infusion is commenced immediately on arrival. Initial bloods show a 10-hour paracetamol level of 182 mg/L and an ALT of 189.
Q2. How do these blood results inform management?
Answer and interpretation
- The 10-hour level of 182mg/L is well above the treatment line, so the NAC infusion should continue for a full course of treatment (minimum of 20 hours), with repeat ALT testing at the end of the infusion.
- If the ALT remains abnormal at the end of the 20-hour infusion, NAC is continued at a rate of 100mg/kg every 16 hours.
- ALT is checked every 12-24 hours until it begins to normalise.
- NAC infusion must continue until the ALT is stable or falling.
- As the ALT is abnormal, bloods should also be sent for coagulation profile, renal function and platelet count to monitor for impending liver failure. These additional markers should also be repeated every 12-24 hours during treatment.
By 56 hours post-ingestion, ALT has risen to 9000, with an INR of 2.5 and a platelet count of 200. She has some RUQ tenderness and nausea. You start to wonder whether you should consider aeromedical retrieval to a tertiary hospital.
Q3. How is paracetamol-induced hepatotoxicity defined?
Answer and interpretation
Paracetamol-induced hepatotoxicity is defined as a peak elevation in hepatic transaminases (ALT or AST) > 1000 IU/L in the context of paracetamol overdose.
This patient clearly has paracetamol-induced hepatotoxicity, along with evidence of impaired liver synthetic function (abnormal INR).
Q4. What are the indications for transfer to a liver transplant service?
Answer and interpretation
High-risk features mandating admission to a liver transplant centre are:
- INR >3.0 at 48 hours or >4.5 at any time.
- Oliguria or creatinine > 200 micromol/L
- Acidosis with pH < 7.3 after resuscitation
- Systolic hypotension with BP < 80mmHg
- Hypoglycaemia
- Severe thrombocytopenia
- Encephalopathy of any degree
Our patient has an INR <3.0 with normal renal function, pH, blood pressure, blood sugar and platelet count and no evidence of encephalopathy – so she does not meet criteria for transfer at this stage.
However, given that transfer to a tertiary centre may take several hours to organise, it would be useful to be able to predict whether this patient is likely to develop fulminant hepatic failure.
Q5. Is there any way of predicting the risk of hepatic encephalopathy in this patient?
Answer and interpretation
The risk of hepatic encephalopathy can be predicted by calculating the Schiodt score.
This scoring system uses three main factors to predict the risk of hepatic encephalopathy:
- (A) Time interval between paracetamol ingestion and commencement of NAC
- (B) INR
- (C) Platelet count
The Schiødt score is calculated: (A + B + C – 99) / 10
This score is then converted to a probability of developing hepatic encephalopathy.
For our patient, the point scores are as follows:
- Time to NAC of 10 hours gives (A) = 40
- INR of 2.5 gives (B) = 51
- Platelet count of 200 at 56 hours gives (C) = –30
Overall score = (40 + 51 – 30 – 99) / 10 = –3.8
This gives our patient an approximately 2-3% probability of developing hepatic encephalopathy.
Given that our patient is still relatively low risk, it is probably safe to leave them in the rural hospital for the time being. Serial blood tests and NAC infusion will need to continue until transaminases are falling and coagulopathy is improving.
Q6. What happened next?
Answer and interpretation
- The patient remained in the rural hospital on a NAC infusion.
- By 72 hours, ALT had fallen to 6000 and INR to 1.9
- By 84 hours, ALT had fallen to 3600, INR to 1.1 and she was feeling much better, with resolution of her RUQ tenderness and nausea.
- Following a further period of observation she was subsequently discharged to the care of psychiatry with no long term sequelae; ALT normalised over the following few days.
References
- Daly FF, Fountain JS, Murray L, Graudins A, Buckley NA; Panel of Australian and New Zealand clinical toxicologists. Guidelines for the management of paracetamol poisoning in Australia and New Zealand–explanation and elaboration. A consensus statement from clinical toxicologists consulting to the Australasian poisons information centres. Med J Aust. 2008 Mar 3;188(5):296-301
- Schiødt FV, Bondesen S, Tygstrup N, Christensen E. Prediction of hepatic encephalopathy in paracetamol overdose: a prospective and validated study. Scand J Gastroenterol. 1999 Jul;34(7):723-8 [PMID 10466885]

CLINICAL CASES
Toxicology Conundrum
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |
