Post-op Pacing Puzzler
aka ECG Exigency 011
It is night time in the surgical ICU and you are called to the bedside of a 72-year old gentleman who is day 2 post-op from a mitral valve repair, CABG x 3, maze procedure and resection of the left atrial appendage (for correction of severe mitral regurgitation and AF).
He still has A+V epicardial pacing wires in situ with AAI pacing set at 90 bpm but the nursing staff are concerned that his rhythm has become irregular. He also complains of some anterior sternal discomfort that is worse with deep breathing and coughing. He is otherwise stable with BP 130/70, MAP 95, clear chest, normal mental status and good urine output.
The nurse asks you: “Are you sure his pacemaker is working OK?”
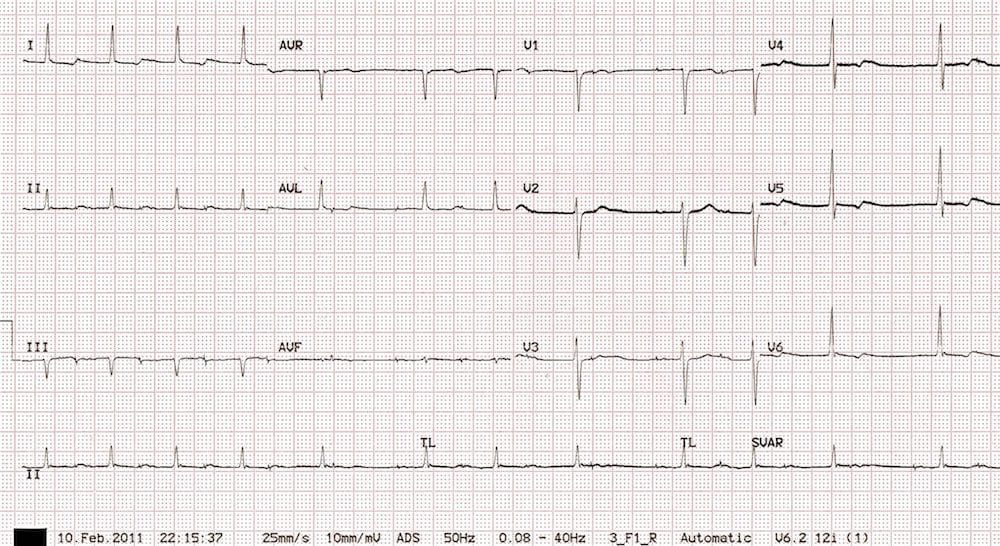
His ECG is shown below:
Questions
Q1. Describe the ECG.
Answer and Interpretation
The ECG shows:
- Atrial paced rhythm with atrial pacing spikes at around 90 bpm
- Narrow QRS (90 ms)
- Each pacing spike is followed by a small P wave, indicating 100% capture of the atria
- There are intermittent non-conducted P waves (dropped QRS complexes) with overall ventricular rate around 72 bpm
- The PR interval increases with each successive beat until a QRS complex is dropped
- PR interval is longest immediately before the dropped beats (460 ms) and shortest immediately after the dropped beats (240 ms)
- No acute ST changes to indicate ischaemia as the cause of his pain
Q2. What is the diagnosis?
Answer and Interpretation
Atrial paced rhythm with 100% atrial capture and second degree AV block with Mobitz I conduction (Wenckebach phenomenon).
Q3. What are the possible causes of this rhythm?
Answer and Interpretation
Wenckebach phenomenon is usually due to impaired conduction at the level of the AV node (unlike Mobitz II where the site of block is infranodal), and may be seen with the following conditions:
- Increased vagal tone (athletes, young children, painful stimuli)
- Valvular heart surgery (especially mitral valve surgery)
- AV nodal blocking drugs (beta-blockers, calcium channel blockers, amiodarone, digoxin)
- Inferior MI
- Congenital heart disease (e.g. Tetralogy of Fallot)
AV block following mitral valve surgery
- AV block is fairly common following mitral valve surgery, as the AV node lies close to the posterior leaflet of the mitral valve.
- In a study of 391 patients following mitral valve surgery (replacement or repair), the incidence of AV block was 23.5%.
- The most common type of AV block was first degree (in 18% of patients), followed by third degree (4%), with second degree block the least common (1.3%).
- A large proportion (44%) of these AV blocks are transient, resolving prior to hospital discharge.
Possible mechanisms for AV block following mitral valve surgery include:
- Direct damage to the AV conduction system during surgery
- Damage to the AV nodal artery causing ischaemia of the AV node
- Prolonged cross-clamp time causing ischaemia of the AV node
- Peri-operative use of AV-nodal blocking drugs
Q4. How would you manage this patient?
Answer and Interpretation
Management
- Withhold any AV nodal blocking drugs
- Correct any electrolyte abnormalities
- Treat his pain (most likely due to his recent sternotomy – but be on the lookout for any signs of myocardial ischaemia)
- Given that this patient is currently haemodynamically stable, there is no need to alter his pacemaker settings at present
- If hypotension developed secondary to a low heart rate, he could be switched over to VVI pacing to maintain cardiac output
- Permanent pacing would need to be considered if haemodynamically unstable AV block persisted beyond the first week post-op
Indications for permanent pacing would include:
- Progression to complete (third degree) AV block
- Development of Mobitz II AV block
- Persistent Mobitz I AV block with an inadequate ventricular rate (causing haemodynamic compromise)
- AF with a slow ventricular response
Q5. Can you guess what happened next?
Answer and Interpretation
- The patient remained in Mobitz I for the next 12 hrs without any drop in BP or deterioration to 3rd degree AV block.
- The following morning he was trialed off pacing and found to be in sinus bradycardia at 56 bpm with a first degree heart block (PR 240 ms); BP was stable at 130/80, so he was switched over to backup VVI pacing with the pacing wires capped after a further few hours.
- The first degree heart block was not present on his pre-op ECG.
- It appears that he had developed some post-op AV dysfunction that resulted in a first degree heart block at slower heart rates and progressed into Mobitz I when paced at a faster rate.
- At present, his first degree heart block persists but he is recovering well from surgery.
References
- Berdajs D et al. Incidence and pathophysiology of atrioventricular block following mitral valve replacement and ring annuloplasty. Eur J Cardiothorac Surg. 2008;34(1):55-61. PMID: 18482844.
- Meimoun P et al. Frequency, predictors, and consequences of atrioventricular block after mitral valve repair. Am J Cardiol. 2002;1;89(9):1062-6. PMID: 11988196.
Further Reading
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
CLINICAL CASES
ECG EXIGENCY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |

Great Case !
Thank You