Troubling Tachycardia
aka ECG Exigency 010
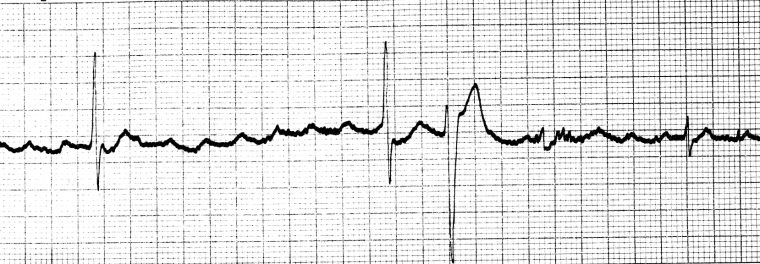
Another crazy night in the ED… One of the nurses hands you this ECG. “Can you take a look at this guy? He doesn’t look so well…”

Questions
Q1. What is the name of this rhythm?
Answer and Interpretation
This is an example of bidirectional ventricular tachycardia with
- Regular broad complex tachycardia
- The frontal-plane axis swings 180 degrees from left to right with each alternate beat
Q2. What are the two main causes of this dysrhythmia?
Answer and Interpretation
- Severe digoxin toxicity
- Familial Catecholaminergic Polymorphic Ventricular Tachycardia (CPVT)
Q3. What are the clinical and ECG features of Digoxin toxicity?
Answer and Interpretation
Digoxin toxicity
Clinical features
- GIT: Nausea, vomiting, anorexia, diarrhoea
- Visual: Blurred vision, yellow/green discolouration, haloes
- CVS: Palpitations, syncope, dyspnoea
- CNS: Confusion, dizziness, delirium, fatigue
Electrocardiographic Features
- Digoxin can cause a multitude of dysrhythmias, due to increased automaticity (increased intracellular calcium) and decreased AV conduction (increased vagal effects at the AV node)
- The classic dysrhythmia associated with digoxin toxicity is the combination of a supraventricular tachycardia (due to increased automaticity) with a slow ventricular response (due to decreased AV conduction), e.g. ‘atrial tachycardia with block’.
Other arrhythmias associated with digoxin toxicity are:
- Frequent VEBs (the most common abnormality), including ventricular bigeminy and trigeminy
- Sinus bradycardia or slow AF
- Any type of AV block (1st degree, 2nd degree & 3rd degree)
- Regularised AF = AF with complete heart block and a junctional or ventricular escape rhythm
- Ventricular tachycardia, including polymorphic and bidirectional VT
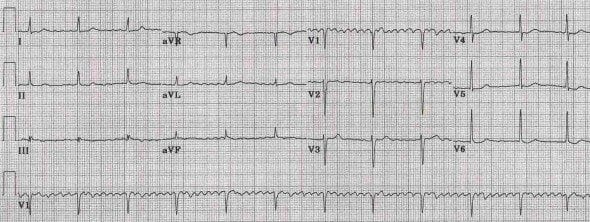
Examples of digoxin toxicity:

Q4. What are the clinical and ECG features of CPVT?
Answer and Interpretation
Clinical features
- An inherited arrhythmogenic disease characterised by episodic palpitations, syncope or cardiac arrest precipitated by exercise or acute emotion (i.e. catecholamine-triggered ventricular dysrhythmias)
- Onset during childhood (mean age: 7-9 years old)
- Family history of sudden cardiac death
- Ventricular arrhythmias reproducible on exercise stress testing
Electrocardiographic Features
- Bidirectional VT
- Polymorphic VT
- Ventricular fibrillation
CPVT Example
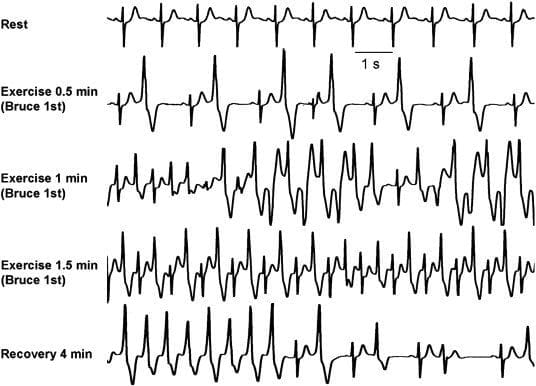
- Exercise stress test in a patient with CPVT.
- Progressively worsening ventricular arrhythmias are observed during exercise.
- Typical bidirectional VT develops after 1 minute of exercise with a sinus heart rate of approximately 120 beats per minute.
- Arrhythmias rapidly recede during recovery.
Q5. How are these conditions treated?
Answer and Interpretation
Digoxin
- The antidote for acute or chronic digoxin toxicity is digoxin-specific immune Fab (‘Digibind’)
- Initial empiric dosing of Digibind is 5 ampoules for acute overdose, 2 ampoules for chronic toxicity and up to 20 ampoules for cardiac arrest
- AV block may respond to atropine 0.6 mg IV bolus, repeated to a maxium of 1.8 mg (20 mcg/kg in children)
- Dysrhythmias may be treated with IV lignocaine 1mg/kg (max 100mg) over 2 minutes
- Hyperkalaemia is treated in the usual way with insulin and dextrose, sodium bicarbonate… however, IV calcium is (traditionally) contraindicated!
- DC cardioversion is unlikely to be successful in digoxin poisoning. Patients in cardiac arrest may require continuous CPR until Digibind can be sourced and administered.
Catecholaminergic Polymorphic Ventricular Tachycardia
- Beta blockers (e.g. propranolol) are used for suppression of catecholamine-triggered ventricular tachydysrhythmias.
- Electrical cardioversion / defibrillation may be required for haemodynamically unstable VT/VF, although patients often spontaneously revert to sinus rhythm.
- Implantable cardioverter-defibrillator (ICD) insertion is considered for primary or secondary prevention of cardiac arrest.
References
- Menduiña MJ, Candel JM, Alaminos P, Gómez FJ, Vílchez J. Bidirectional ventricular tachycardia due to digitalis poisoning. Rev Esp Cardiol. 2005 Aug;58(8):991-3. Spanish [PMID: 16053836] [Full text – English]
- Smith SW, Shah RR, Hunt JL, Herzog CA. Bidirectional Ventricular Tachycardia Resulting From Herbal Aconite Poisoning (Case Report). Annals of Emergency Medicine 2005; 45(1):100-101. [PMID: 15635326]
- Napolitano C, Priori SG, Bloise R. Catecholaminergic Polymorphic Ventricular Tachycardia. 2004 Oct 14 [updated 2009 Jul 7]. In: Pagon RA, Bird TC, Dolan CR, Stephens K, editors. GeneReviews [Internet]. Seattle (WA): University of Washington, Seattle (1993) [PMID: 20301466]
- Hampton, JR. The ECG In Practice, 6e
- Mattu A, Brady W. ECG’s for the Emergency Physician 1
- Mattu A, Brady W. ECGs for the Emergency Physician 2
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric, 6e
- Wagner, GS. Marriott’s Practical Electrocardiography 12e
Further Reading
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
CLINICAL CASES
ECG EXIGENCY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |
