Why so blue?
aka Toxicology Conundrum 053
A 40-year-old man presented to the emergency department with shortness of breath, chest pain and reported a pre-syncopal episode.
On questioning he reports increased lethargy, weakness, pallor and an occasional blue hue to his hands over the past two weeks. He has a past medical history of hypertension, unprovoked PE and SLE unresponsive to first line treatments for which he has recently started new medications.
Drug History: Prednisolone, Methotrexate, Dapsone and Hydroxychloroquine
Initial bedside observations
- T 36.5
- HR 85
- BP 155/90
- RR 18
- SpO2 85% on 8L via Hudson mask
- ECG Normal sinus rhythm
Radiology: His CXR was unremarkable
Questions
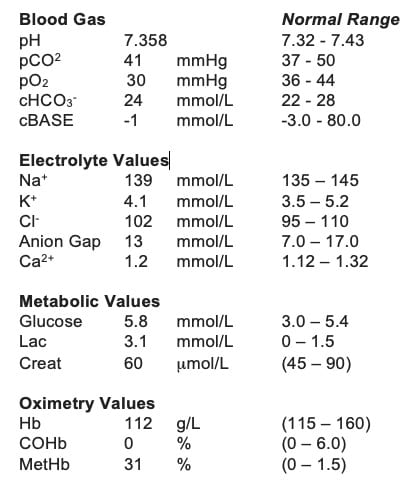
Q1. Here is the venous blood gas result on arrival. What does it show?
Answer
Methaemoglobinaemia
Q2. What are the clinical features of this condition?
Answer
- Cyanosis
- Symptoms of acute impairment of oxygen delivery to tissues (e.g. chest pain, dyspnoea, altered mental status and end organ damage)
- Chocolate brown blood on sampling
- Normal PaO2
- SpO2 85%
- Dizziness
- Fatigue
Q3. What is the initial management?
Answer and Interpretation
1) Asymptomatic and methaemoglobin level <20%:
- Stop causative agent
2) Methaemoglobin level >20%:
- Stop causative agent
- High flow oxygen
- Methylene Blue 1-2mg/kg IV slow push over 5 minutes
- Expect significant clinical improvement within 10 – 60 minutes
- Repeat dose of Methylene Blue between 30-60 minutes if still symptomatic and methaemoglobin level >20 (1)
Note: the methaemoglobin level is expressed as a percentage of the total haemoglobin level. Therefore this is relative based on the patient’s total haemoglobin level. If a patient has a raised methaemoglobin level but less than 20% and is symptomatic you may wish to treat on clinical grounds.
Q4. Are there any specific considerations in the management of this condition?
Answer and Interpretation
Yes.
Cumulative doses of Methylene Blue (>7mg/kg) can cause dyspnoea, chest pain and haemolysis. (2)
Methylene Blue is contraindicated in G6PD deficiency (a congenital cause of methaemoglobinaemia) and can result in acute haemolysis. (3)
In acquired methaemoglobinaemias secondary to drug ingestion, such as Dapsone, consider activated charcoal. Dapsone has active metabolites that undergo entero-hepatic circulation therefore you may require multiple-dose activated charcoal (MDAC).
Sulfhaemoglobin can cause similar symptoms and be erroneously detected as methaemoglobin by co-oximetry. Sulfhaemoglobinaemia will not respond to Methylene Blue.
Routine pulse oximetry is inaccurate in the presence of methaemoglobin. A high concentration of methaemoglobin, due to its absorption of both wavelengths of light used by standard pulse oximetry, will show oxygen saturations of 85% regardless of the true haemoglobin oxygen saturation. (4)
Q5. What is the likely cause in this patient?
Answer and Interpretation
Acquired methaemoglobinemia secondary to Dapsone.
Dapsone, known for its use in leprosy, is an antibiotic that blocks folic acid synthesis. It may also act and an immunomodulator for the treatment of skin diseases. (5)
Q6. What other commonly used medications can cause this?
Answer and Interpretation
There are many drugs that can cause methaemoglobinaemia but the most common or clinically important include(1)
- Dapsone
- Some local anaesthetic agents (e.g. prilocaine)
Other agents to be aware of:
- Aniline and aniline derivatives used in industry (e.g. aniline dyes, aminophenol, phenylhydroxylamine)
- Benzene derivatives (used as solvents)
- Nitrates / Nitrites (Amyl nitrate (‘poppers’), nitroglycerin, sodium nitroprusside, NO)
- Metoclopramide
Note: Drugs with oxidant properties such as benzocaine and dapsone are sometimes added to recreational drugs. Therefore, may be the cause of otherwise unexplained acquired methaemoglobinaemias. (6)
Q7. Other than medication what other causes are there?
Answer and Interpretation
Congenital.
- Cytochrome b5 reductase deficiency
- Haemoglobin M disease
Q8. What is the basis for this condition?
Answer and Interpretation
Methaemoglobinemia is the presence of excess methaemoglobin in the blood. Normal haemoglobin contains ferrous iron (Fe2+), methaemoglobin is formed when the ferrous iron in haemoglobin is oxidised to the ferric state (Fe3+). This is clinically important as methaemoglobin (Fe3+) is unable to reversibly bind oxygen. Furthermore, it increases the oxygen affinity of any remaining ferrous (Fe2+) haemes in the haemoglobin tetramer resulting in a left shift of the oxygen dissociation curve. (7)
In normal homeostasis, small amounts of methaemoglobin are formed by auto oxidation. These are cleared by NADH-dependant pathways catalysed by cytochrome b5 reductase. Methaemaglobinaemia results from either a congenital defect in the body’s normal clearance of methaemoglobin, or increased oxidation of haemoglobin by medication with oxidant properties. (1)
References
- Josef T Prchal, MD. Clinical features, diagnosis, and treatment of methemoglobinemia. UpToDate. November 2018.
- Coleman MD, Coleman NA. Drug-induced methaemoglobinaemia. Treatment issues. Drug Saf 1996; 14:394. [PMID 8828017]
- Rosen PJ, Johnson C, McGehee WG, Beutler E. Failure of methylene blue treatment in toxic methemoglobinemia. Association with glucose-6-phosphate dehydrogenase deficiency. Ann Intern Med 1971; 75:83. [PMID 5091568]
- Barker SJ, Tremper KK, Hyatt J. Effects of methemoglobinemia on pulse oximetry and mixed venous oximetry. Anesthesiology 1989; 70:112 [PMID 2912291]
- Australian Medicines Handbook Online. Dapsone. January 2019. https://amhonline.amh.net.au/chapters/anti-infectives/antibacterials/antimycobacterials/dapsone
- Falkenhahn M, Kannan S, O’Kane M. Unexplained acute severe methaemoglobinaemia in a young adult. Br J Anaesth 2001; 86:278. [PMID 11573675]
- Darling R, Roughton F. The effect of methemoglobin on the equilibrium between oxygen and hemoglobin. Am J Physiol 1942; 137:56.

CLINICAL CASES
Toxicology Conundrum
Chris is an Emergency Medicine Specialist with an interest in diagnostic and procedural ultrasound. He works at Sir Charles Gairdner Hospital in Perth, Western Australia. In addition to working in a tertiary Emergency Department he has experience in retrieval medicine with Royal Flying Doctor Service Western Operations, acute patient transport co-ordination with WA Country Health Service and in education as director of MedVault Education in Association with the Australian Medical Association WA.

