Airway – Tracheostomy emergencies
Procedure, instructions and discussion
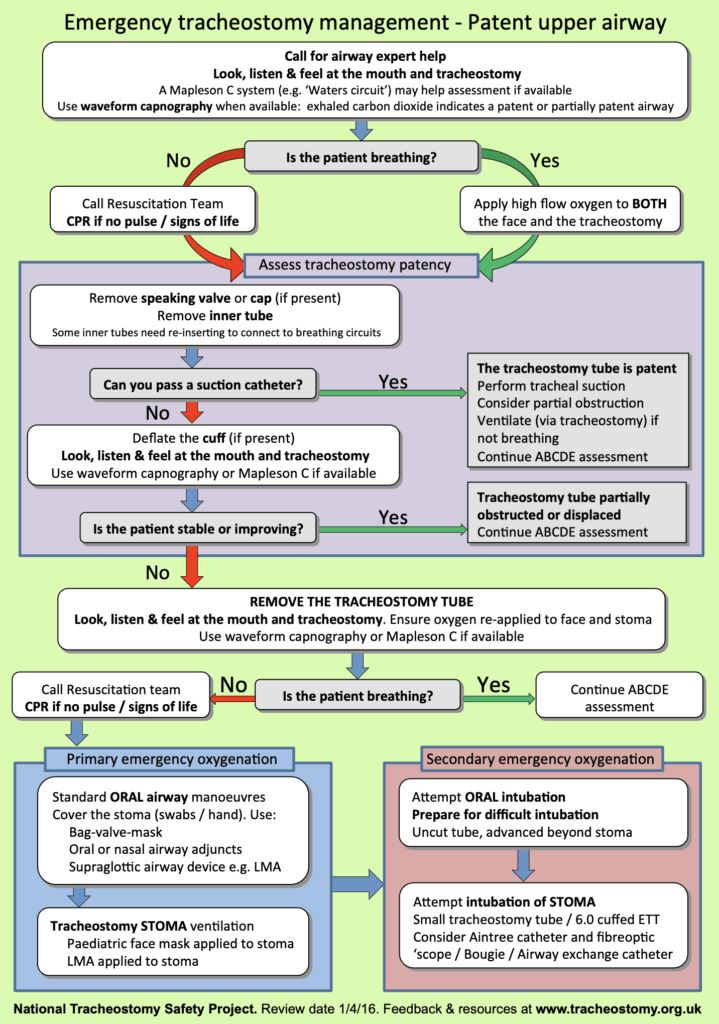
Tracheostomy emergencies for patients in respiratory distress or following accidental decannulation
Detailed written instructions and explanation are available in our Free App (iOS and Android). This video is hot off the press and we want your help improving it. Drop us a line with any suggestions
Instructions
Indications
- Respiratory distress
or
- Accidental decannulation
Contraindications (ABSOLUTE/relative)
- None
Informed consent
NOT REQUIRED
- Consent is not required.
- This is an emergency procedure to save a life
Potential complications (of tube replacement)
- Failure
- False passage (paratracheal, oesophageal)
- Trauma (trachea, brachiocephalic trunk, vocal cords, nerves, thyroid)
- Mucosal ulceration (cuff pressure)
- Infection
Infection control
- Standard precautions
- PPE: non-sterile gloves, N95 mask, protective eyewear or shield
Area
- Resuscitation bay prepared for a difficult airway
- Including waveform capnography (gold standard for assessing stoma ventilation)
Staff
- Team leader (working through the flowchart)
- Two airway clinicians (stoma and upper airway)
Equipment (bedside)
Ideally in a prepared box for use in tracheostomy emergencies
- Nurse call bell (patient may be unable to call for help verbally)
- Adult airway adjuncts, LMA and bag valve mask
- LMA size 2 (to be held over stoma to seal if required)
- Two tracheostomy tubes to replace blocked tube (same size and one size smaller e.g. Shiley 5 + Portex 6, 7, 8)
- Heat-moisture exchange device (to replace blocked heat-moisture exchange device)
- Spare inner cannula (to replace blocked cannula)
- Size 6 ETT (if tracheostomy tubes unavailable)
- Bougie
- Water-soluble lubricating jelly
- Suction catheters (10-14F, larger may be required for mucus plugs)
- Yankeur suction (oral suction)
- Sterile water (cleaning the suction tube)
- Tracheostomy mask, humidifier bulb and O2 connector
- 10 ml syringe for deflating and inflating tracheostomy cuff
- Scissors and stitch cutter (cutting tracheostomy sutures)
- Tracheal dilating forceps (may help open tract)
- Dressing pack, tracheostomy dressings and tape
- A fibreoptic scope if available (e.g. Ambu aScope)
Positioning
- Position of comfort, usually sitting up to prevent aspiration
Medication
- 0.9% Saline for nebulisation
Sequential treatment
Easily reversible respiratory problems (sputum plugging, malposition) cause mortality in tracheostomy patients. We advocate a sequential approach prior to tube replacement.
- High flow oxygen
- Nebulised saline
- Remove speaking valve or cap
- Remove inner tube
- Suction
- Cuff deflation (allowing ventilation around tracheostomy)
- Tube removal and ventilation (without replacement)
- Tube replacement and ventilation (stomas >10 days)
Sequence
Respiratory failure (progress through steps until resolution)
- High flow oxygen to stoma and face
- Remove phonation or humidification cap and inner cannula
- Insertion suction catheter to stoma and assess for patency (patent if passes easily deeply into trachea)
- Ensure cuff deflated (allowing ventilation around a tracheostomy tube displaced against the tracheal wall)
- Remove outer cannula (sutures may need to be cut)
- Non-invasive ventilation (oral BVM or LMA and stoma oxygen by paediatric face mask or size 2 LMA held over stoma)
- Invasive ventilation (insert new tracheostomy tube or size 6 ETT over bougie or fibreoptic scope)
- Consider intubating via oral cavity with deep cuff placement beyond tracheostomy (not in laryngectomy)
- Surgical airway below existing tracheostomy (see surgical airway procedure)
Accidental decannulation (progress through steps until resolution)
- High flow oxygen to stoma and face
- Non-invasive ventilation (stoma and mouth oxygen, LMA and paediatric LMA to stoma)
- Invasive ventilation (insert new tracheostomy tube or size 6 ETT over bougie or fibreoptic scope)
- Consider intubating via oral cavity with deep cuff placement beyond tracheostomy (not in laryngectomy)
- Surgical airway below existing tracheostomy (see surgical airway procedure)
Post-procedure care
- Monitor in resuscitation bay
- Frequent saline nebulisers (reduce mucus viscosity)
- Urgent ENT and anaesthetic assessment
- If intubated tie tube (one finger space between tie and neck allowing for venous return)
- Check cuff pressure through pilot cuff
- Document procedures with size and type of tracheostomy placed
Tips
- Expect a leak around an uncuffed tracheostomy tube (close mouth and pinch nares to minimise)
- Percutaneous tracheostomies <10 days are impossible to replace (the dilated stoma tract tissues recoil)
- Laryngectomy patients have no connection between the mouth and lungs, airway management from above is futile
Discussion
We recommend a prepared box of equipment be available in each department, to be placed by the bed of tracheostomy patients in case of respiratory distress. This procedure guide is based on the flowcharts and approach produced and freely available at tracheostomy.org.uk. [PDF]
The principles of care for respiratory failure are the same as for other intubated patients. Apply the “DOPE” mnemonic in emergency situations (Displacement, Obstruction, Patient, Equipment). If the patient loses cardiac output, these steps should be followed alongside standard ALS treatment
Speaking valves can be used incorrectly and small humidifying devices (e.g. Swedish noses) and inner tubes can become blocked with secretions. Any such device attached to a tracheostomy tube should be removed in an emergency, which may resolve the obstruction. Passing a soft suction catheter will then confirm patency. If patent, the patient can be ventilated via the tracheostomy (inflate cuff or close mouth and nares to reduce leak). If not patent, the tracheostomy tube will need to be removed, followed by oronasal ventilation with or without another tracheostomy tube being placed.
Laryngectomy patents do not have an upper airway in continuity with the lungs. The principles of the algorithm are the same, without the conventional upper airway management steps. Patients with laryngectomies usually do not have a tracheostomy tube in situ, but may have other devices inserted into their airways to allow speech via the oesophagus (tracheo-oesophageal puncture ‘TEP’ valves). These devices should be left in place during resuscitation
References
- National Tracheostomy Safety Project. Manchester, UK: National Tracheostomy Safety Project; 2020
- McGrath BA, Bates L, Atkinson D, Moore JA; National Tracheostomy Safety Project. Multidisciplinary guidelines for the management of tracheostomy and laryngectomy airway emergencies. Anaesthesia. 2012 Sep;67(9):1025-41.
- Long B, Koyfman A. Resuscitating the tracheostomy patient in the ED. Am J Emerg Med. 2016 Jun;34(6):1148-55.
- Bontempo LJ, Manning SL. Tracheostomy Emergencies. Emerg Med Clin North Am. 2019 Feb;37(1):109-119.
- NSW Agency for Clinical Innovation. Care of adult patients in acute care facilities with a tracheostomy. Sydney: ACI; 2013. 91pp
- Hess DR. Tracheostomy tubes and related appliances. Respir Care. 2005 Apr;50(4):497-510.
- Kannan S, Birch JP. Controlled ventilation through a tracheostomy stoma. Anaesth Intensive Care. 2001 Oct;29(5):557.
- Ball DR, Paton L, Jefferson P, Caldwell D. Tracheostomy ventilation using a laryngeal mask as a ‘bridge to extubation’. Anaesthesia. 2010 Dec;65(12):1232-3.
The App
Emergency Procedures
Dr James Miers BSc BMBS (Hons) FACEM, Staff Specialist Emergency Medicine, Prince of Wales Hospital. Lead author of Lead author of Emergency Procedures App | Twitter | YouTube |
Dr John Mackenzie MBChB FACEM Dip MSM. Staff Specialist Emergency Prince of Wales Hospital; Consultant Hyperbaric Therapy POW HBU. Lead author of Emergency Procedures App | Twitter | | YouTube |


