Bartter Syndrome
Bartter syndrome refers to a group of renal tubulopathies characterised by hypokalaemic metabolic alkalosis, elevated renin and aldosterone levels, normal or low blood pressure and polyuria.
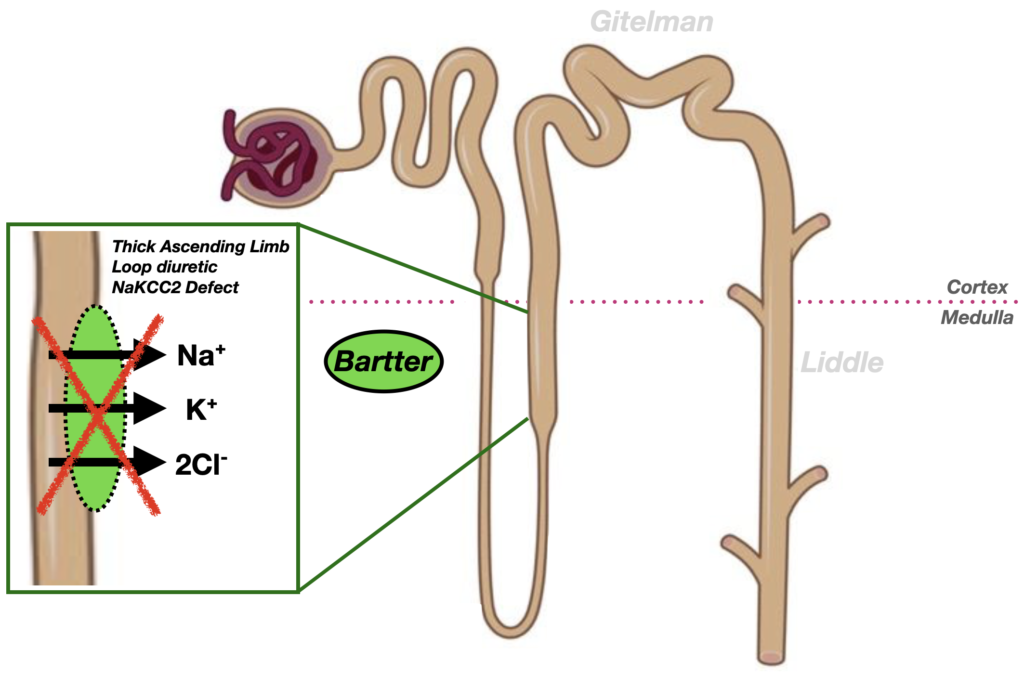
Classically, a defect in the NKCC2 co-transporter of the thick ascending limb causes renal salt wasting, leading to chronic volume depletion. This activates the renin–angiotensin–aldosterone system (RAAS), with juxtaglomerular hyperplasia (the cells which produce renin) and correspondingly high aldosterone levels. However, because the kidney cannot retain sodium, blood pressure stays normal, producing the hallmark of Bartter syndrome: hyperaldosteronism without hypertension. This is a pathophysiological mimic of the loop diuretic effect.
Hypercalciuria comes from a disruption of the normal calcium-reabsorption mechanism in the thick ascending limb (TAL). Reduced potassium recycling renders the tubule less positively charged, thus reducing the electrochemical drive to resorb calcium.
Pathophysiology and Classification: Subsequent genetic discoveries have classified Bartter syndrome into at least five types, each linked to transport defects in the thick ascending limb of Henle
- Type I – SLC12A1 (NKCC2)
- Type II – KCNJ1 (ROMK)
- Type III – CLCNKB
- Type IV – BSND (often with sensorineural deafness)
- Type V – MAGED2 (X-linked, transient antenatal form)
Clinical Subtypes:
- Classic Bartter syndrome – Onset in childhood with polyuria, growth failure, and salt craving.
- Antenatal Bartter syndrome – Polyhydramnios, postnatal severe hypokalaemia and metabolic alkalosis.
Therapeutic Development:
Initially treated with potassium and sodium supplementation plus spironolactone, the condition was later found to improve with prostaglandin-inhibiting NSAIDs (e.g. indomethacin). Current management centers on tailored electrolyte replacement, prostaglandin blockade, and long-term growth monitoring in children.
Bartter’s identification of this paradoxical form of normotensive hyperaldosteronism fundamentally altered understanding of renal sodium handling and volume regulation. The syndrome remains a key model for salt-losing nephropathy and has illuminated the roles of renal transporters in genetic hypertension and electrolyte disorders.
Summary
Bartter syndrome affects the thick ascending limb of the loop of Henle, where a defect in the Na⁺-K⁺-2Cl⁻ cotransporter (NKCC2) leads to NaCl wasting, hypokalaemia, metabolic alkalosis, and hypercalciuria, a profile mimicking loop diuretic effect.
History
1962 – First described in 1962 by Frederic Crosby Bartter (1914-1983) and colleagues, the condition fundamentally challenged prevailing models of sodium and volume regulation. Bartter et al. published Hyperplasia of the juxtaglomerular complex with hyperaldosteronism and hypokalemic alkalosis. A new syndrome.
We have described two patients who appear to represent examples of a new syndrome characterized by hyperplasia of the juxtaglomerular complex of the kidney, secondary hyperaldosteronism, hypokalemic alkalosis, and normal or low blood pressure…
Bartter, 1962
Despite striking activation of the renin-angiotensin-aldosterone system, both patients remained normotensive and showed no evidence of increased vascular reactivity.
Comparative Context:
Comparison of Bartter, Gitelman and Liddle syndromes
| Feature | Bartter Syndrome | Gitelman Syndrome | Liddle Syndrome |
|---|---|---|---|
| Defect location | Thick Ascending Limb of Loop of Henle | Distal Convoluted Tubule | Collecting Duct (ENaC channel) |
| Transporter affected | NKCC2 (Na⁺-K⁺-2Cl⁻ cotransporter) | Na⁺-Cl⁻ cotransporter (SLC12A3) | Epithelial Na⁺ Channel (ENaC; SCNN1B/SCNN1G) |
| Pathophysiologic mimic | Loop diuretics (lose Ca²⁺) | Thiazide diuretics (preserve Ca²⁺) | Aldosterone excess (but low aldosterone) |
| Serum potassium (K⁺) | ↓ Hypokalaemia | ↓ Hypokalaemia | ↓ Hypokalaemia |
| Serum bicarbonate (HCO₃⁻) | ↑ Metabolic alkalosis | ↑ Metabolic alkalosis | ↑ Metabolic alkalosis |
| Serum magnesium (Mg²⁺) | Normal or mildly ↓ | ↓ Hypomagnesemia | Normal |
| Urinary calcium | ↑ Hypercalciuria | ↓ Hypocalciuria | Normal |
| Blood pressure | Normal or low | Normal or low | ↑ Hypertension |
| Renin | ↑ Elevated | ↑ Elevated | ↓ Suppressed |
| Aldosterone | ↑ Elevated | ↑ Elevated | ↓ Suppressed |
| Age of onset | Neonatal/Childhood | Childhood/Adolescence | Childhood/Adolescence |
| Response to treatment | NSAIDs (↓ prostaglandins), K⁺, spironolactone | Mg²⁺ and K⁺ supplementation, ± NSAIDs | Amiloride or triamterene (ENaC inhibitors) |
Associated Persons
- Frederic Crosby Bartter (1914-1983) | Bartter Syndrome
- Grant Winder Liddle (1921-1989) | Liddle Syndrome
- Hillel Jonathan Gitelman (1932-2015) | Gitelman Syndrome
References
Historical references
- Bartter FC, Pronove P, Gill JR Jr, MacCardle RC. Hyperplasia of the juxtaglomerular complex with hyperaldosteronism and hypokalemic alkalosis. A new syndrome. Am J Med. 1962 Dec;33:811-28
Eponymous term review
- Unwin RJ, Capasso G. Bartter’s and Gitelman’s syndromes: their relationship to the actions of loop and thiazide diuretics. Curr Opin Pharmacol. 2006 Apr;6(2):208-13.
- Konrad M et al. Diagnosis and management of Bartter syndrome: executive summary of the consensus and recommendations from the European Rare Kidney Disease Reference Network Working Group for Tubular Disorders. Kidney Int. 2021 Feb;99(2):324-335.
eponymictionary
the names behind the name
BMedSci (Pharm) MB ChB, Edinburgh University. Emergency and Internal Medicine training. Interested in neuropharmacology and electrophysiology
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | On Call: Principles and Protocol 4e| Eponyms | Books |

