Bundgaard syndrome
Description
Bundgaard et al introduced us in 2018 to “Familial ST-segment depression syndrome”, a new cardiac arrhythmia syndrome predisposing to atrial fibrillation, VT, and sudden cardiac death.
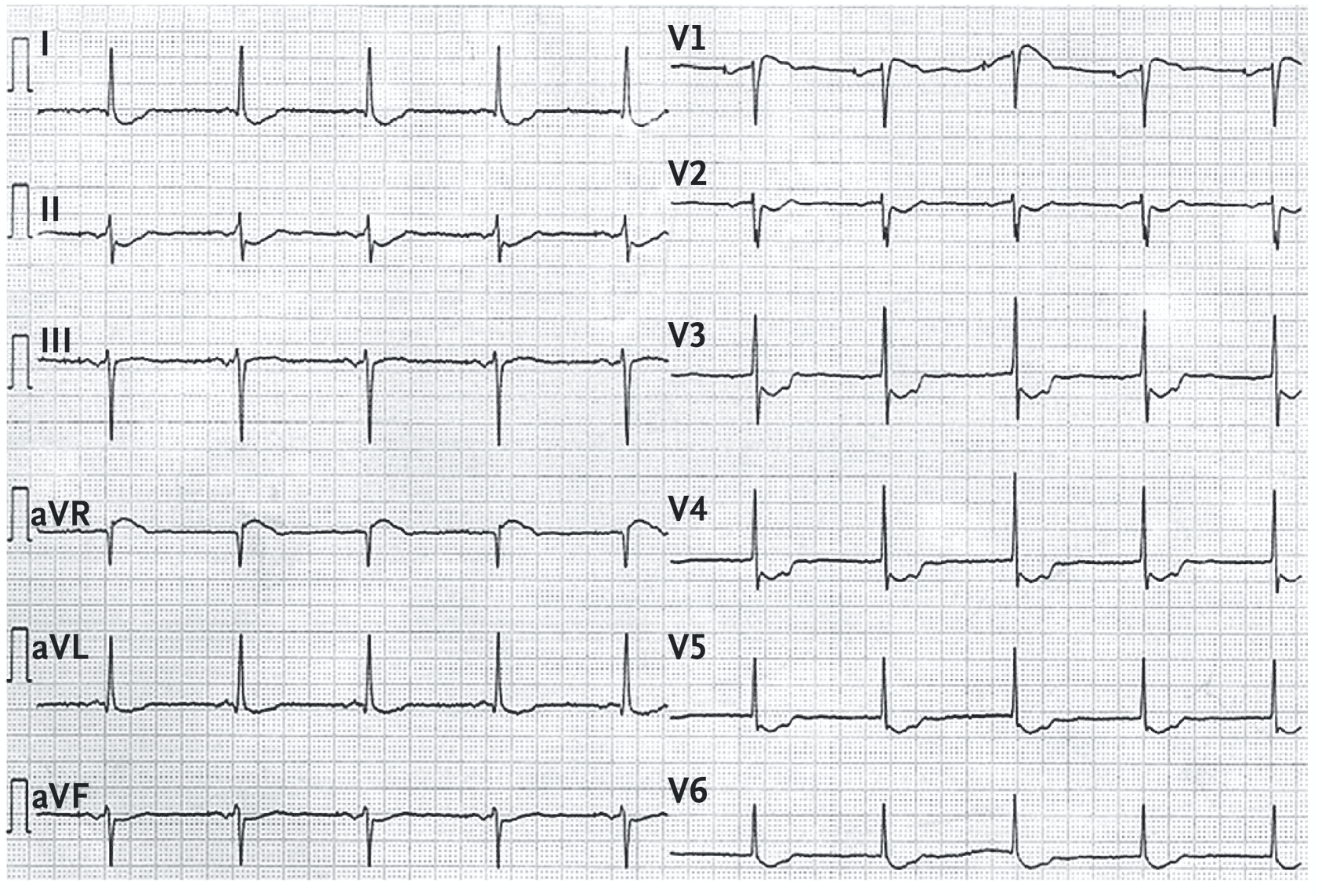
- ECGs reviewed from five unrelated families demonstrated a consistent pattern of widespread, concave-upward ST depression, in the absence of coronary artery disease or ischaemia. In contrast to other genetic disorders such as Brugada syndrome and LQTS, these changes remain stable over time, only accentuated by exercise.
- Affected individuals had varying time courses of disease, but usually remained asymptomatic until the onset of tachyarrhythmias, often initially atrial fibrillation with subsequent episodes of VT/VF leading to sudden cardiac death.
Diagnosing “Familial ST-segment depression syndrome”
- Unexplained concave-upward ST depression in at least 7 leads, 90ms after J point
- ST elevation in lead aVR > 0.1mV
- ECG findings are persistent with time
- Autosomal dominant pattern of inheritance
The authors proposed the above diagnostic criteria, with “unexplained” highlighting the importance that ischaemia, structural heart disease and metabolic abnormalities have been excluded prior to labelling the condition.
Other secondary diagnostic features were accentuation seen with exercise in some, and the presence of a notch in the ascending part of the ST segment. Note that onset of complications do not appear to correlate with age based on limited observations of affected individuals.

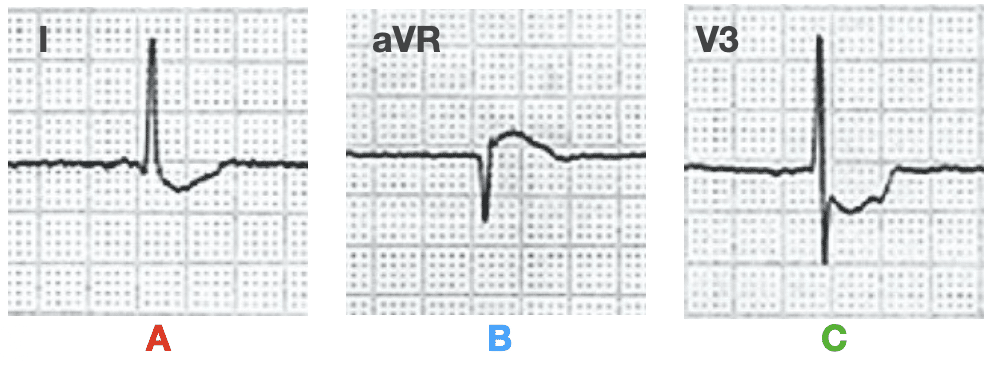
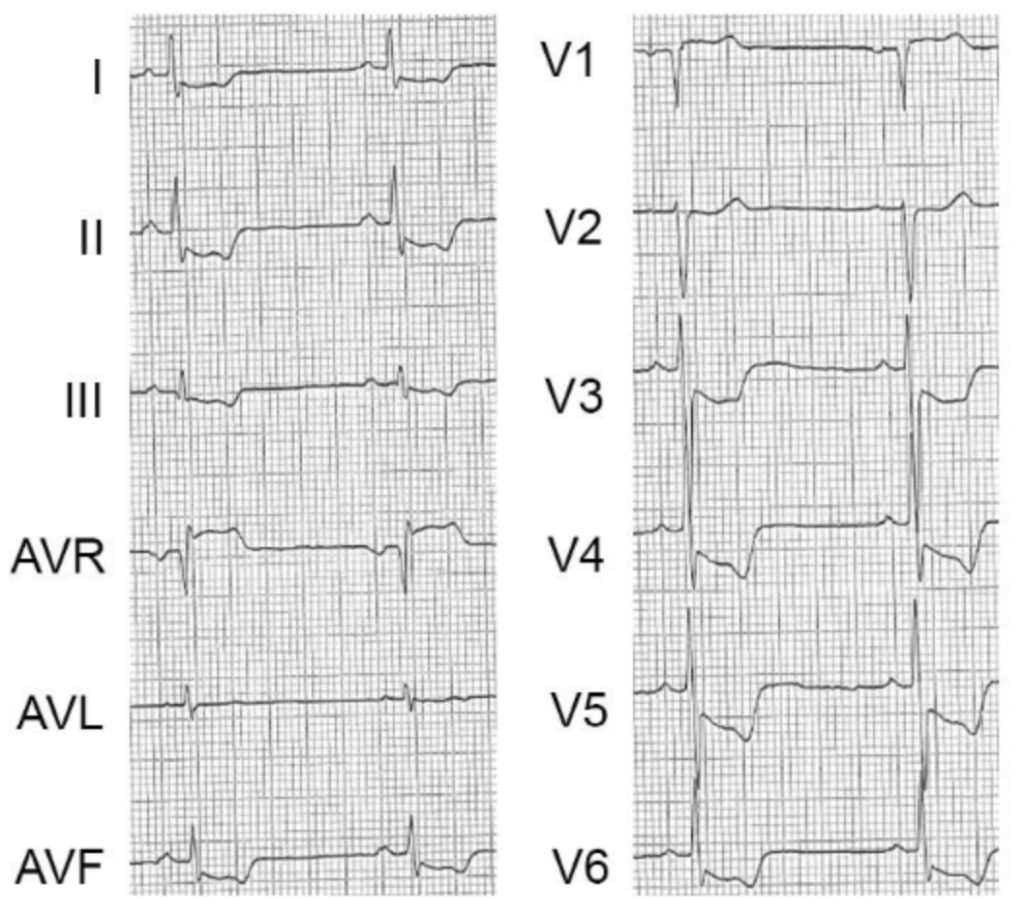
- (A) concave-upward ST-segment depression in leads I, II, aVL, aVF, V2-V6,
- (B) ST-segment elevation in lead aVR.
- (C) A notch is visible in the ascending part of the ST segment of the precordial leads, most prominent in leads V3-V4
Clinical significance: Doesn’t that look familiar?
- The pattern of “diffuse ST depression with coexistent ST elevation in lead aVR” would be familiar to many of us. In the acute chest pain presentation it raises concern for LMCA insufficiency causing severe ischaemia. Although this pattern is no longer thought to be an indicator of acute occlusion, these NOMI patients should undergo urgent catherisation following medical therapy
- Patients with Familial ST-segment Depression Syndrome presenting with chest pain may be mistakenly identified as suffering from an acute ischaemic event. Subsequent unremarkable laboratory and angiography findings, in combination with the “static” nature of this pattern, should raise concern for FSDS and prompt further investigation and screening of family members
- Genetic testing for cardiovascular disorders in affected individuals was negative and to date a causative genetic sequence is yet to be identified
Further examples
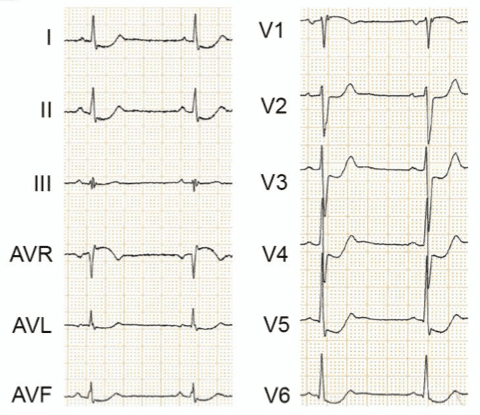
Example 1
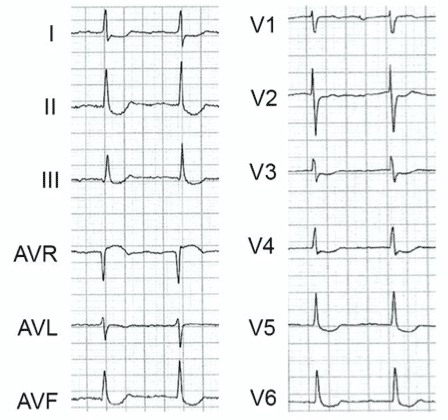
Example 2
Example 3
Associated Persons
- Henning Bundgaard. Department of Cardiology, Rigshospitalet, University Hospital Copenhagen, Denmark
References
Historical references
- Bundgaard H, Jøns C, Lodder EM et al. A Novel Familial Cardiac Arrhythmia Syndrome with Widespread ST-Segment Depression. N Engl J Med. 2018 Nov 1;379(18):1780-1781.
Eponymous term review
- Rawshani A. A Novel Familial Cardiac Arrhythmia Syndrome Identified Using ECG. ECGWaves 2018
- Marstrand P, Theilade J, Andersson C, et al. Long QT syndrome is associated with an increased burden of diabetes, psychiatric and neurological comorbidities: a nationwide cohort study. Open Heart 2019; 6: e001161
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
eponymictionary
the names behind the name
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner


Translated to catalan here https://emermedpirineus.eu/sindrome-de-bundgaard/
Thanks very much for your work