Charles Foix
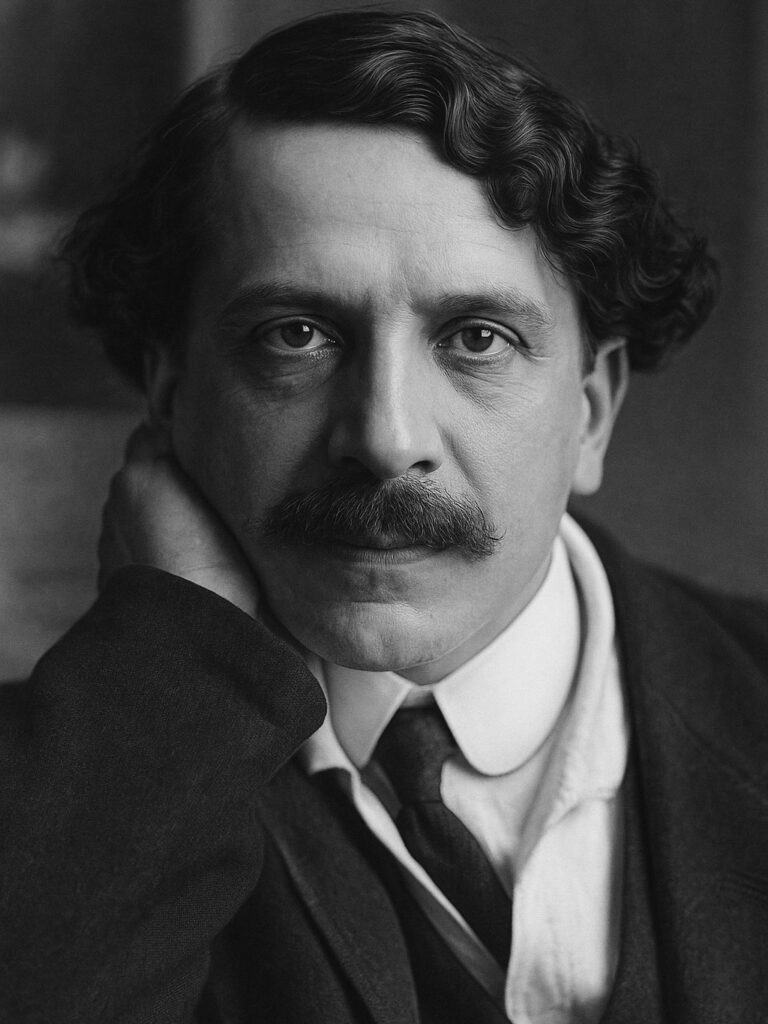
Charles Foix (1882-1927) was a French neurologist.
Foix was one of the most gifted clinical observers and neuropathologists of early 20th-century French neurology. A protégé of Pierre Marie (1853-1940) and later mentor to Théophile Alajouanine (1890-1980), Foix helped usher in a new era of anatomoclinical correlation through detailed studies of vascular anatomy, brainstem syndromes, and spinal cord pathology. His legacy includes multiple enduring eponyms such as Foix-Alajouanine syndrome, Foix-Chavany-Marie syndrome, and Marie-Foix syndrome.
Born in Salies-de-Béarn in 1882, Foix moved to Paris to study medicine and began his career under Georges Marinesco and Pierre Marie at the Salpêtrière. He quickly distinguished himself through exceptional autopsy-based research and original anatomical illustrations. By the 1920s, Foix had become a leading voice in French neurology, co-authoring seminal papers on cerebrovascular territories and pathologies with colleagues such as N. Hillemand and Théophile Alajouanine.
Foix was especially committed to understanding the vascular supply of the brainstem and spinal cord. His 1926 and 1927 publications helped establish vascular topography as a clinical tool, influencing generations of neurologists. He also demonstrated how chronic spinal arteriovenous malformations led to progressive myelopathy, work that would later be eponymised as Foix-Alajouanine syndrome.
A reserved and disciplined man, Foix rarely sought the spotlight but was deeply respected by his peers. His career was cut tragically short by leukemia at the age of 44, yet his legacy endures in both nomenclature and neurological practice.
Biographical timeline
- 1882 – Born February 1, in Salies-de-Béarn, France
- 1900 – Began medical studies in Paris.
- 1906 – Became interne des hôpitaux; trained at Salpêtrière under Pierre Marie and Georges Marinesco.
- 1910 – Earned medical doctorate with a thesis on cerebral vasculature.
- 1914–1918 Served in World War I as a military neurologist.
- 1918 – Appointed chef de clinique at Salpêtrière.
- 1922 – Published work on vascular anatomy of the brainstem and pons.
- 1924 – Co-authored studies with Hillemand on medullary and pontine infarction.
- 1926 – Described necrotising myelopathy from spinal vascular malformation (Foix-Alajouanine syndrome).
- 1926 – Published foundational work on cerebrovascular territories and occlusions.
- 1927 – Died of leukaemia on March 24 in Paris, aged 44.
- Died March 22, 1927 aged 43
Medical Eponyms
Foix-Alajouanine syndrome (Syndrome de Foix-Alajouanine) 1926
Rare subacute necrotizing myelopathy, historically associated with thrombosis of spinal medullary veins, now understood to stem from congestive myelopathy due to spinal dural arteriovenous fistulas (AVFs). This progressive myelopathy leads to paraplegia, sensory disturbances, sphincter dysfunction, and eventual death if untreated. The condition affects primarily middle-aged adults, with a strong male predominance.
First described by Charles Foix and Alajouanine in 1926, it was termed “myélite nécrotique subaiguë” and believed to represent spinal cord ischaemia due to vascular occlusion. Modern neuroimaging and angiography have since clarified the underlying pathophysiology as venous hypertension resulting from dural AVFs, causing spinal cord edema and infarction—especially in the thoracolumbar region.
In contemporary neurology, the term “Foix–Alajouanine syndrome” is generally reserved for non-haemorrhagic spinal AVMs or dural AVFs that present with progressive myelopathy, often mimicking other cord pathologies such as cauda equina or MS.
1926 – Foix and Alajouanine publish La myélite nécrotique subaiguë describing two fatal cases of progressive paraplegia with spinal cord necrosis and vascular congestion.
1989 – Criscuolo et al. redefine the syndrome’s pathogenesis as reversible congestive myelopathy secondary to dural AVFs rather than irreversible spinal artery thrombosis.
2000s–2020s – MRI and DSA become standard for diagnosis; successful treatments via embolization or surgical ligation improve prognosis significantly when diagnosed early.
2024 – Atallah et al. publish a pooled analysis of 26 confirmed FAS cases, clarifying diagnostic criteria, typical imaging findings, and best outcomes with early surgical ligation.
Marie–Foix Syndrome (1913)
Marie–Foix syndrome describes a classical brainstem stroke syndrome involving the lateral pons, presenting with ipsilateral cerebellar ataxia and contralateral hemiparesis. It reflects a crossed hemiplegic syndrome due to interruption of cerebellar and pyramidal tracts, typically attributed today to infarction in the territory of the anterior inferior cerebellar artery (AICA).
This syndrome was originally described by Pierre Marie and Charles Foix in 1913 through cases of syphilitic brainstem involvement, and further summarised in 1914. While modern terminology prefers anatomical descriptors (e.g. AICA infarct), this eponym remains of historical significance in cerebrovascular neurology.
1913 – Marie and Foix publish two case reports in La Semaine Médicale:
- One patient with pure hemicerebellar syndrome due to syphilitic mid-pontine lesion.
- Four patients with ipsilateral cerebellar and pyramidal signs. “La lésion, macroscopiquement minuscule, sectionnait tout le pédoncule cérébelleux moyen...”
1914 – Revue Neurologique publishes a detailed review summarising these findings (vol 28(14): 93-94). It classifies the syndromes into three clinical types:
- Ipsilateral cerebellar and pyramidal signs with contralateral oculomotor palsy
- Ipsilateral cerebellar and pyramidal signs with dysarthria
- Ipsilateral cerebellar and pyramidal signs with thalamic symptoms
1922 – Marie, Foix, and Alajouanine publish a separate work on cortical cerebellar atrophy, leading to long-standing eponymous confusion with Marie–Foix–Alajouanine syndrome.
Modern usage – “Marie–Foix syndrome” now generally refers to the lateral pontine stroke syndrome, often replaced in clinical settings by “AICA infarct syndrome” or “lateral pontine syndrome.”
Marie–Foix–Alajouanine syndrome (1922)
A progressive cortical cerebellar atrophy typically seen in older adults, with a strong association to chronic alcohol use. Clinically, it manifests with gait ataxia, dysarthria, intention tremor, and truncal instability — classic features of cerebellar dysfunction. Histologically, the condition involves degeneration of Purkinje cells, particularly in the anterior lobe of the cerebellum.
Originally described in 1922 by Pierre Marie, Charles Foix, and Théophile Alajouanine as l’atrophie cérébelleuse tardive à prédominance corticale, the syndrome was framed as a late-onset, predominately cortical cerebellar degeneration. While most commonly seen in alcoholics, a hereditary form was later described by Richter in 1950, suggesting an autosomal dominant inheritance in select families.
In modern neurology, the term is used less frequently, with most cases now subsumed under alcoholic cerebellar degeneration or spinocerebellar ataxias (SCAs), depending on aetiology and family history.
Foix–Chavany–Marie syndrome (FCMS) (1926)
Also known as the anterior opercular syndrome, is a rare form of bilateral pseudobulbar palsy caused by lesions of the anterior operculum — the cortical area overlying the insula. Clinically, it presents with facial diplegia, anarthria, linguo-bucco-facial apraxia, and dysphagia, despite preserved limb movement and automatic emotional facial responses. This striking dissociation, termed automatic-voluntary dissociation, distinguishes it from brainstem lesions.
The condition results from bilateral infarction, trauma, or degenerative disease affecting the frontal opercular cortices, which contain the cortical representation of cranial nerve motor control.
1837 – Adolph Magnus describes a case suggestive of automatic-voluntary dissociation in Fall von Aufhebund dis willenseinflusses auf einige Hirnnerven. This early case of dissociation between voluntary and emotional cranial nerve control is retrospectively linked to opercular dysfunction.
1926 – Charles Foix, Jean Alfred Émile Chavany (1892-1959), and French paediatrician Julien Marie (1899–1987) published Diplégie facio-linguo-masticatrice d’origine sous-corticale sans paralysie des membres (contribution à l’étude de la localisation des centres de la face du membre supérieur). They describe patients with bilateral opercular lesions causing profound dysarthria and bulbar symptoms with preserved emotional expression.
Mid-20th century – Syndrome becomes a classic model of cortical pseudobulbar palsy, particularly in differentiating from brainstem strokes.
Late 20th century–present – It remains a recognised clinical entity in stroke neurology, neurorehabilitation, and the assessment of higher-level bulbar motor control. Used in the context of bilateral MCA infarcts, ALS variants, and neurodegenerative cortical syndromes.
Major Publications
- Marie P, Foix C. Sur la retrait réflexe du membre inférieure provoqué par la flexion forcée des orteils. Revue neurologique, 1910; 26(14): 121-123. [Marie-Foix manoeuvre and reflex]
- Foix C. Activité leucocytaire et pouvoir leuco-activant des humeurs. Thèses du 19e siècle. 1911
- Marie P, Foix C. Les réflexes d’automatisme medullaire. Revue neurologique, 1912; 23(10): 657-676 [Marie-Foix manoeuvre and reflex]
- Marie P, Foix C. Hémisyndrome cérébelleux d’origine syphilitique: hémiplégie cérébelleuse syphilitique. La Semaine Médicale. 1913; 33(2): 13–15. [Marie-Foix syndrome]
- Marie P, Foix C. Formes cliniques et diagnostic de l’hémiplégie cérébelleuse syphilitique. La Semaine Médicale. 1913; 33(13): 145–152. [Marie-Foix syndrome]
- Marie P, Foix C. Atrophie isolée de l’éminence thénar d’origine névritique. Rôle du ligament annulaire dans la localisation de la lésion. Revue Neurologique 1913; 26: 647-649
- Feindel E. Review of: Formes cliniques et diagnostic de l’’Hémiplégie Cérébelleuse syphilitique et Hémisyndrome Cérébelleux d’Origine Syphilitique : Hémiplégie Cérébelleuse Syphilitique. Revue Neurologique 1914; 28(14): 93-94
- Foix C. Les lésions anatomiques de la maladie de Parkinson. Revue Neurologique 1921; 28: 593–600
- Foix C. Syndrome de la paroi externe du sinus caverneux (ophtalmoplégie unilatérale à marche rapidement progressive. Algie du territoire de l’ophtalmique). Amélioration considérable par le traitement radiothérapique. Revue neurologique, 1922; 38(6): 827-832. [Foix syndrome II]
- Marie P, Foix C, Alajouanine T. De l’atrophie cérébelleuse tardive à prédominance corticale.
Revue neurologique 1922; 38(7): 849-885 and 1922; 38(8): 1082-1111. [Marie-Foix-Alajouanine syndrome] and [Marie-Foix syndrome] - Foix C, Masson A. Le syndrome de l’artère cérébrale postérieure. La Presse Médicale 1923; 31: 361-365.
- Foix C, Nicolesco J. Anatomie cérébrale. Les moyens gris centraux et la région mesencephalo-sous-optique; suivi d’une appendice sur l’anatomie pathologique de la maladie de Parkinson. Paris: Masson, 1925
- Foix C. Les syndromes de la region thalamique. La presse médical, 1925; 33: 113-117. [Foix syndrome I]
- Foix C, Chavany JA, Marie J. Diplégie facio-linguo-masticatrice d’origine sous-corticale sans paralysie des membres (contribution à l’étude de la localisation des centres de la face du membre supérieur). Revue Neurologique. 1926; 1: 214–219. [Foix–Chavany–Marie syndrome]
- Foix C, Alajouanine T. La myélite nécrotique subaiguë (Myélite centrale angiohypertrophique à évolution progressive). Paraplégie amyotrophique lentement ascendante d’abord spasmodique, puis flasque. Revue neurologique 1926; 2: 1-42. [Foix-Alajouanine disease]
References
Biography
- Caplan LR. Charles Foix–the first modern stroke neurologist. Stroke. 1990;21(2):348-356.
- Caplan LR. Charles Foix (1882-1927). J Neurol. 2010;257(11):1941-1942.
- Tessaro CL, Doubek JGC, Pedro MKF. Beyond the Neurologist: Charles Foix as a Poet and a Playwright. Eur Neurol. 2024;87(3):140-146.
Eponyms
- Magnus A. Fall von Aufhebund dis willenseinflusses auf einige Hirnnerven. Archiv für Anatomie, Physiologie und wissenschaftliche Medicin. 1837: 258–266
- Hillemand P. Charles Foix et son Oeuvre, 1882–1927 Clio Medica, 1976; 11(4): 269-287
- Criscuolo GR, Oldfield EH, Doppman JL. Reversible acute and subacute myelopathy in patients with dural arteriovenous fistulas. Foix-Alajouanine syndrome reconsidered. J Neurosurg. 1989 Mar;70(3):354-9.
- Bhatt N, Bhatt N. Foix-Alajouanine syndrome: a case report. Eur J Neurol. 2007 Aug;14(8):e4-5
- Ferrell AS, Tubbs RS, Acakpo-Satchivi L, Deveikis JP, Harrigan MR. Legacy and current understanding of the often-misunderstood Foix-Alajouanine syndrome. Historical vignette. J Neurosurg. 2009;111(5):902-906.
- Delgado-García G, Rodríguez-Návarez C, Coron T, Estañol B. Marie-Foix Syndrome: A Classical Crossed Pontine Syndrome? AAN Abstract P4.9-046. Neurology 2019; 92(15 supplement)
- Turgut, A.Ç., Tubbs, R.S. & Turgut, M. French neurologists Charles Foix and Jean Alfred Émile Chavany and French pediatrician Julien Marie and the Foix-Chavany-Marie syndrome. Childs Nerv Syst 2020; 36: 2597–2598
- Atallah O, Almealawy YF, Arian R, Dwebi A, Badary A, Abdul Hussein AF, Sanker V, Zafarshamspour S, Chaurasia B, Agrawal A, Pastrana Brandes S, Azab MA. Foix-Alajouanine syndrome: a comprehensive overview of rare but relevant diagnosis. Ann Med Surg (Lond). 2024 Sep 30;86(11):6636-6644.
Eponym
the person behind the name
