Charles Macklin

Charles Clifford Macklin (1883-1959) was a Canadian pulmonologist.
He showed great interest in pulmonary histology, physiology. The majority of his 130 publications investigated the structure and function of the lung and its pathology
Eponymously remembered for his description of the Macklin Effect (1937).
Biography
- Born in 1883
- 1903-1908 Moved to Toronto, Canada to work at the Medical Department of the Canada Assurance Company. Here, one of his superiors, Dr. Scadding, recognized his ability and suggested he go to medical school.
- 1908 – Accepted into the University of Toronto Medical School.
- 1912 – Won the James Richardson Fellowship in Anatomy
- 1914 – MB, University of Toronto
- 1918 – MD, University of Toronto
- 1918 – Married Madge Thurlow Macklin (1893 – 1962)
- 1921 – 1953 – Professor of anatomy, Professor of History and Embryology, University of Western Ontario
- 1923 – MA, PhD, University of Toronto
- 1924 – Fellow of Royal Society of Canada
- 1953 – Retired. Degree of Doctor of Science, University of Western Ontario
- Died on November 23, 1959 in London, Ontario at the age of 76
Medical Eponyms
Macklin Effect (1939)
The Macklin effect describes one of the pathophysiological processes of pneumomediastinum in blunt chest trauma. The Macklin effect relates to a three-step pathophysiologic process:
- blunt traumatic alveolar ruptures,
- air dissection along bronchovascular sheaths, and
- spreading of this blunt pulmonary interstitial emphysema into the mediastinum.
Spontaneous pneumomediastinum (SPM) is defined as the presence of mediastinal free air in the absence of an obvious precipitating cause. The first case series of spontaneous pneumomediastinum was published in 1939 by Louis Hamman (1877-1946). Macklin proposed the term Hamman sign in the same year.
Although pneumomediastinum has been recognized clinically for a long time, there has been a recent revival of interest in it, and some important points have been emphasized. One of these is the curious crunching sound heard over the region of the heart in some cases, and which, on account of the prominence given to it by Hamman, may be known as Hamman’s sign.
Macklin 1939
First proposed by Macklin in 1937 and elaborated in 1939. The pathophysiological process was experimentally demonstrated by Macklin and Madge Macklin in 1944. Barotrauma causes alveolar rupture which then allows air to flow down a pressure gradient from the alveolus to the mediastinum via the pulmonary interstitium and pulmonary hilum (the Macklin effect).
The Macklin effect is involved in secondary pneumomediastinum such as in blunt trauma, but also in pneumomediastinum arising in conditions, such as respiratory distress syndromes; barotrauma; asthma; mechanical ventilation; and valsalva manoeuvres (e.g. parturition, intense vomiting and epileptic seizures)
2001 – Wintermark and Schnyder evaluated 51 patients with severe blunt trauma between 1995 and 2000 with severe trauma or high-speed deceleration justifying chest CT. The Macklin effect was diagnosed when an air collection adjacent to a bronchus and a pulmonary vessel could be clearly identified on the chest CT. Clinical relevance of the Macklin effect was statistically evaluated regarding its repercussions on the pulmonary gas exchange function, the respective durations of intensive care and total hospital stay, and the associated injuries.
The Macklin effect was present in 39% of severe blunt traumatic pneumomediastinum detected by CT. Its identification does not rule out a tracheobronchial injury. The Macklin effect reflects severe trauma, and is associated with significantly prolonged intensive care stay.
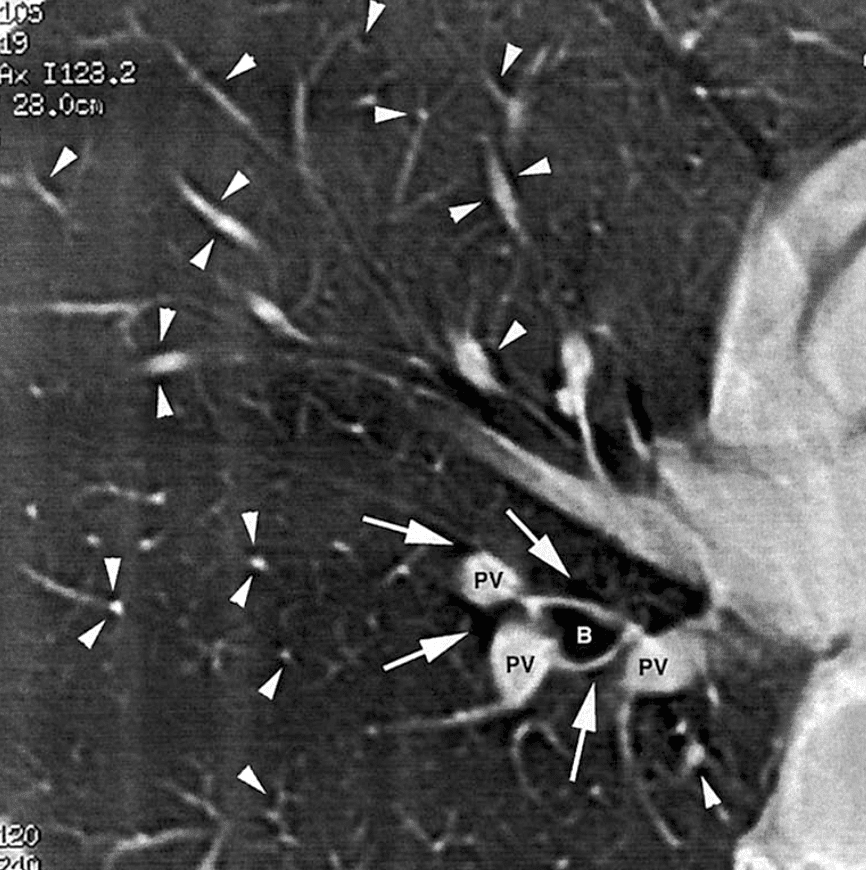
Fig 1: The Macklin effect: pulmonary interstitial emphysema, with multiple air lucencies (arrowheads) contiguous to small pulmonary vessels on both lung fields. The Macklin effect is definitely diagnosed only when a triad bronchus (B); pulmonary vessel (PV); adjacent air collection (arrows) is clearly identified on the chest CT
Major Publications
- Macklin CC. Pneumothorax with Massive Collapse from Experimental Local Over-inflation of the Lung Substance. Can Med Assoc J. 1937 Apr; 36(4): 414–420.
- Macklin CC. Spontaneous Mediastinal Emphysema: A Review and Comment, Medical Record. 1939; 150: 5.
- Macklin CC. Transport of air along sheaths of pulmonic blood vessels from alveoli to mediastinum: clinical implications. Arch Intern Med (Chic). 1939; 64(5): 913-926
- Macklin CC, Macklin MT. Air block in lung blast? Lancet 1942; 239(6194): 602
- Macklin MT, Macklin C. Malignant interstitial emphysema of the lungs and mediastinum as an important occult complication in many respiratory diseases and other conditions: an interpretation of the clinical literature in the light of laboratory experiment. Medicine 1944; 23: 281-358
References
Biography
- Barr ML, Buck RC, Jarvis CE. Dr. Charles Clifford Macklin: an appreciation. Can Med Assoc J. 1960;82(6):335.
- Staub NC, Clements JA, Permutt S, Proctor DF. Charles Clifford Macklin, 1883-1959: an appreciation. Am Rev Respir Dis. 1976;114(5):823-830.
- Staub NC. Charles Clifford Macklin (1883-1959): Pioneer Canadian Pulmonologist. Canadian Respiratory Journal 1994; 1(3): 199-207
Eponymous terms
- Hamman L. Spontaneous mediastinal emphysema. Bulletin of the Johns Hopkins Hospital 1939; 64: 1-21
- Zylak CM, Standen JR, Barnes GR, Zylak CJ. Pneumomediastinum revisited. Radiographics. 2000; 20: 1043–1057
- Wintermark M, Schnyder P. The Macklin effect: a frequent etiology for pneumomediastinum in severe blunt chest trauma. Chest. 2001 Aug;120(2):543-7.
- Kelly S, Hughes S, Nixon S, Paterson-Brown S. Spontaneous pneumomediastinum (Hamman’s syndrome). Surgeon. 2010;8(2):63-66.
- Murayama S, Gibo S. Spontaneous pneumomediastinum and Macklin effect: Overview and appearance on computed tomography. World J Radiol. 2014; 6 (11): 850-4
Graduated Medicine in 2020 from Queens University Belfast. Interested in Internal Medicine.

