Cognitive Aids in Healthcare
“Have you a plan of action so developed that the right thing is always done in the emergency and time is not frittered away with useless or non-essential details?”
W.Babcock (1924)1
What is a cognitive aid?
In its simplest form, a cognitive aid can be defined as any external representation that supports cognitive processes demanded by a task.2
They present in many different formats to support a multitude of actions in both domestic and industrial sectors.
In healthcare they include checklists, emergency manuals, alarms, reminders like hand hygiene wall posters and mnemonics such as iSoBAR. For the purpose of this review, our focus will be on two areas that have received significant attention over the last decade concerning patient safety – checklists and emergency or crisis manuals.
Is there a difference between a checklist and a cognitive aid?
The scope of cognitive aids is vast, and terminology can be confusing. Cognitive aid is an all-encompassing term for tools that help reduce cognitive load when performing tasks (usually complex, tightly coupled or time pressured), helping reduce errors of both action and omission. Checklists and emergency manuals are both cognitive aids.
History of Cognitive Aids in High Reliability Organisations (HROs)
“When are we going to quit with the aviation stuff?! We are not pilots and patients aren’t planes!” 3. The aviation safety analogy has been thoroughly dissected by the healthcare community. However, there is a reason why we continue to look at HROs like commercial aviation and nuclear energy for safety inspiration.
Checklists in aviation emerged in the 1930s following the B299 Flying Fortress crash on take-off during a test flight. The very experienced military test pilot, Major Ployer Peter Hill, had forgotten to disengage the lock on the control surfaces. The routine use of pre-take-off checklists were subsequently implemented.4 (Fig.1)
As more lessons in aviation were learned, checklist development expanded and the QRH (Quick Reference Handbook) emerged – a cognitive aid to assist flight crew in managing in flight emergencies.
From these experiences came the well-known adage, aviation regulations are written in blood. This sentiment applies equally to health care. It is frequently from someone else’s tragedy protocols and checklists emerge. The Elaine Bromiley story5 and the patient safety initiatives that followed is a prima facie example.
History of Cognitive Aids in Patient Safety
Atul Gawande’s The Checklist Manifesto, published in 2011 and generating the global introduction of the Surgical Safety Checklist6 is perhaps the highest profile cognitive aid in healthcare. However, also published in 2011 was The Anaesthetic Crisis Manual7, soon followed by the Stanford Emergency Manual8 and the Harvard Operating Room Emergency Checklists.
The emergence of this manual format of cognitive aid was predicated on the pioneering work started decades ago by Stanford’s David Gaba10 and University of South Australia’s William Runciman11 – both giants in their field of anaesthesia and patient safety.
They recognised the organisational similarities between aviation and anaesthesia and adapted aviation safety initiatives. In particular, the introduction of simulation, crew (crisis) resource management and the use of cognitive aids became embedded in specialist training programs12.
When should cognitive aids be used?
Since the 1991 landmark Harvard Medical Practice study13 and the follow up Quality in Australian Healthcare Study14 suggested 3.7 to 16.6% of hospitalisations experience adverse events, there have been global initiatives to reduce patient harm. Examples include the 2011 Helsinki Declaration15 as well as the emergence of patient safety networks and foundations.
One of the key components of a multifaceted approach to reduce patient harm has been the promotion of Cognitive Aids.
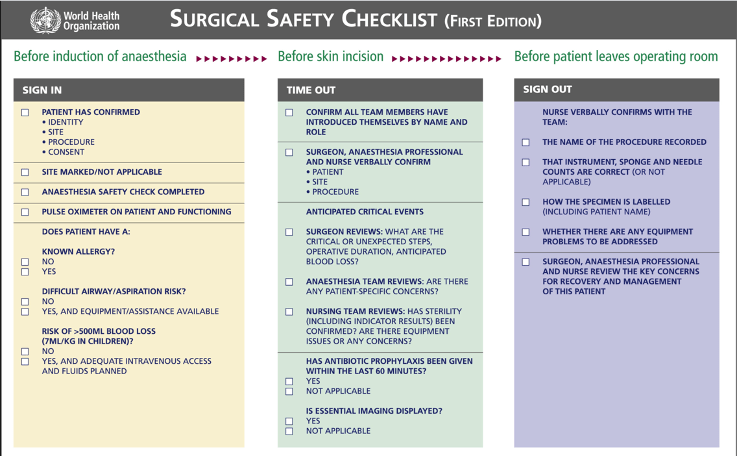
The Surgical Safety Checklist has been the most successful example of cognitive aid implementation in reference to both user acceptance and evidence to support its impact on patient outcomes.16
Many more checklists have since been introduced for handovers (iSoBAR), intubation, CVC insertion and other similar procedures, with varying degrees of acceptance by clinicians. Interestingly, checklist fatigue in healthcare professionals is a very real issue, exacerbated by poor design, poor accessibility and questionable indications17.
Overwhelming healthcare professionals with multiple checklists risks undermining compliance and effectiveness.
Although there are many potential areas in healthcare for cognitive aids, complex, time sensitive tasks with potential catastrophic outcomes have been the focus during the last decade. In anaesthesia and critical care, the main targets have been management of emergencies, patient handover and airway control.
Content
Deciding on checklist and manual content is both context and task specific. Checklists are specifically tailored to prevent errors of omission (e.g., failing to give intraoperative antibiotics) or missteps (giving penicillin to a patient with allergy) during task completion.
Emergency or Crisis Manuals (not infrequently labelled ‘checklists’ or ‘tick box medicine’ by those with a negative perception!), contain guideline based prescriptive emergency protocols. It is well recognised cognitive load can rapidly escalate with time-pressure, anxiety, unfamiliar environments or equipment, and ‘high-stakes’ procedures18. They are designed to improve performance through prompting, reduction of cognitive load (assisting executive function) and enhanced memory recall.
Appropriate international, national, local and hospital guidelines should be used wherever appropriate. If not available, expert consensus can be used.
Design Principles
Much has been written on the importance of cognitive aid design using knowledge and experience from HROs like aviation19 as well as that in healthcare20,21,22. There is even a ‘checklist’ for checklists23. Regardless, most healthcare professionals greet cognitive aid creation with more enthusiasm than design awareness, often leading to disappointing results despite considerable effort.
Design should be based on minimalist principles providing only essential information for the stated purpose – vital to minimize user’s cognitive load and decision-making time, so quality and quantity of information is crucial.
Perhaps the biggest transgression when creating CAs, is including too much information. Doctors have acquired a vast amount of knowledge involving significant detail from medical school onwards so the tendency to include too much is often irresistible and not surprising. However, the more information and the more complex the instruction, the greater cognition required – increasing rather than decreasing cognitive load.
Good prescriptive protocols are logical and appear deceptively simple but achieving this requires merciless word culling. Culling should be taken to the extreme without losing the directive’s meaning while also avoiding ambiguity. Iterative testing by multiple frontline users helps to sharpen the focus and justify the presence (or exclusion) of each word.
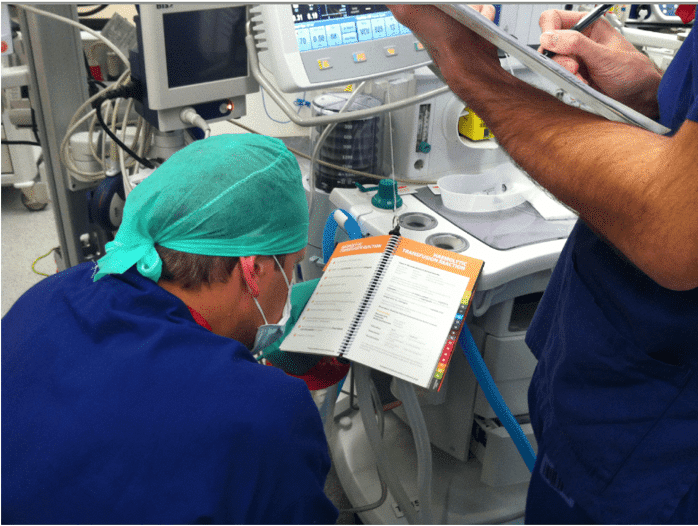
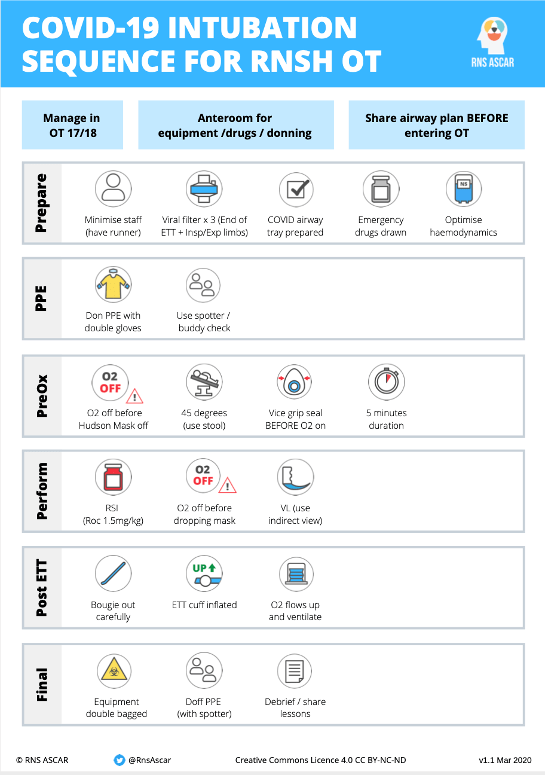
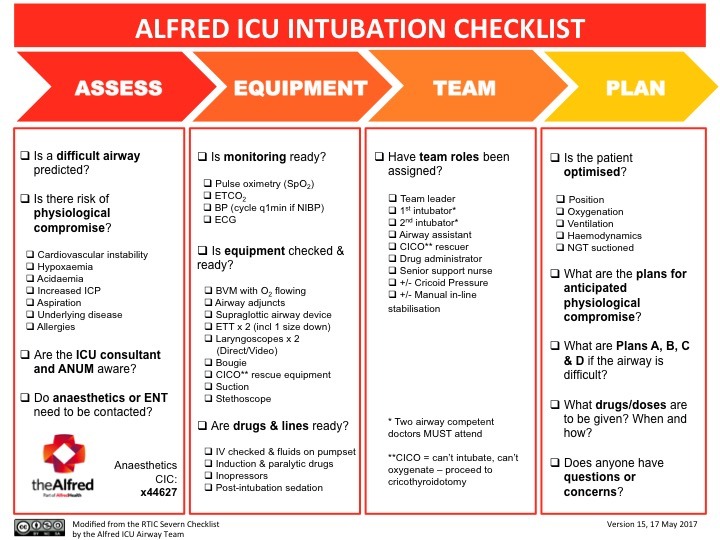
Checklists can be accomplished with a tick box structure (Fig. 2) as often the order of items is not a priority. Emergency protocols more frequently are written in a prioritised, linear sequence and numbered accordingly – usually from the top to bottom or left to right across a page (fig 3.). Well-designed Covid intubation protocols such as that from Royal North Shore Hospital (Fig. 4) show features of both prescriptive and checklist type cognitive aids and include a pictorial component.
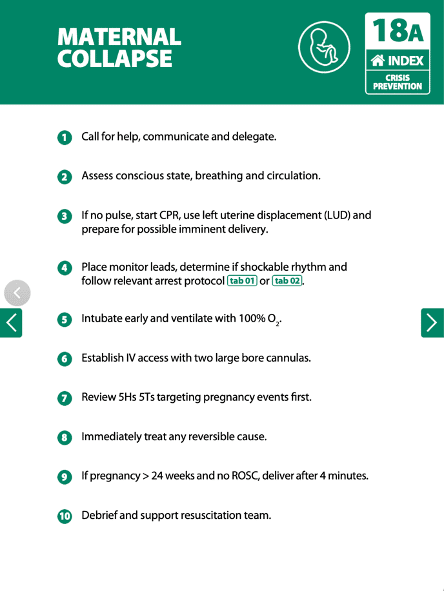
Summary of design principles
- Be specific about the procedure to be addressed and keep that focus.
- Be clear about the goal, e.g. preventing contamination, following recommended guidelines.
- Use short, concise, unambiguous sentences and avoid detail.
- 7-10 steps or directives on page clearly numbered or boxed.
- Make flow logical, intuitive, and hierarchical (most crucial tasks first).
- Minimise questions. Directives reduces choice and the associated cognitive load.
- Format with maximal white space, symmetry, balance, proportion, alignment and consistency to ease the visual burden24.
- Use minimal colour wisely – to emphasise, highlight, guide, categorise and engage25.
How should cognitive aids be used?
In “real time”
The use of checklist cognitive aids is relatively uncomplicated. For example, the surgical safety checklist is systematically read through before surgery starts by a designated leader of the ‘Team Time Out’ process, with call and response closed loop communication principles applied. For example, “have antibiotics been given?” “Yes, 2gm Cephazolin given”.
Similarly the intubation checklist in the Emergency Department or ICU can be systematically worked through with the airway doctor and assistant cross-checking all items are present and confirming a shared mental model (Plan A,B,C, D) with the entire team (Fig. 5). Sub-teams can perform different components of the checklist, for instance the airway sub-team may perform the equipment checks and report to the team leader, rather than the entire resuscitation team checking every component.
Using emergency manuals is more complicated and related to team dynamics, the high intensity and often changing environment of a crisis scenario, institutional safety culture and individual clinician acceptance26.
There was perhaps both an expectation (and concern) in the early days of crisis manual implementation that a delegated reader would read to the team leader the prioritised individual steps and perform the designated steps in a didactic SOP format similar to a captain – first officer interaction using the QRH.
This misconception and the perceived threat to intellect, acquired skill and professional autonomy may have contributed to a disappointingly slow integration of emergency manual into crisis management. Clinician responses deriding manuals as ‘cheat sheets’, ‘cookbook medicine’, ‘tick-box exercises’ and ‘medicine for dummies’ indicated a lack of cultural support for widespread adoption, highlighted by one response from an experienced resuscitationist suggesting, “If you need a manual to resuscitate a patient, get out of the way and let somebody in who knows what they’re doing!”
However, through a greater understanding of human factors and how teams work, simulation studies and the concerted effort of specialist societies, training colleges, FOAM and local champions, the strategic use of cognitive aids to support decision making and treatment is more commonly being perceived as good medical practice rather than weakness.
Resuscitation team leaders can delegate a ‘reader’ of the protocol to follow team actions without interrupting flow but prompting an action should any steps be missed. In essence, this cognitively ‘off-loads’ the leader and helps maintain situational awareness.27 Simulation studies continue to support improved team performance and reduced anxiety during resuscitations using cognitive aids28.
In “down time”
Participating in an unexpected cardiac arrest during an elective procedure was this author’s inspiration for creating a crisis manual cognitive aid. Reflecting on the chaos, difficulty in recalling cycle times and drug doses under pressure, role confusion and general lack of structure when managing a rare event, provided the impetus.
Understanding human factors in its design has been a priority. Overinclusive, complicated and ill-conceived laminated guidelines scattered across walls or tied to airway trolleys provides false reassurance that information or instructions can be easily retrieved in the heat of the moment.
Many factors influence how manuals are used (or not used) including design, content, availability, accessibility, exposure, familiarity, and training. Being easily visible in all resuscitation locations and immediately within reach of the clinician can promote memory ‘refresh’, familiarization, drill rehearsal, teaching and heightened awareness during downtime (Fig. 6). Keeping practitioners ‘on their toes’ – to expect the unexpected and be ready should such an event unfold – may all lead to better performance before the manual is actually opened during a real event.
Do cognitive aids work?
Few would argue that checklist cognitive aids when operating machinery in HROs such as nuclear power plants and commercial aviation are beneficial in promoting safety. However, it could be said components of such industries are designed and manufactured from the ‘ground up’ by human operators. Obviously, patients are not programmed ‘robots’ but complex, sophisticated physiological systems not always predictable. In addition, healthcare is often a fluid, dynamic environment and doesn’t always lend itself to rigid protocols – our monitors may indicate physiological derangement but don’t necessarily pinpoint aetiology.
Combined with the infrequency of intraoperative crises, this makes outcome studies difficult and may contribute to emergency manual ‘hesitancy’ among established practitioners.
The WHO surgical safety checklist (SSC) is an example of a checklist cognitive aid proven effective in changing team behaviour and improving patient outcomes30. Endorsement by Health Ministers and incorporating it into National Safety and Quality Healthcare Standards (NSQHS)31 helped implementation from the ‘top down’.
Given the SSC is used before every procedure in a controlled pre-procedural pause (usually without time pressure), studies soon emerged supporting its use. In contrast, opportunities for assessing crisis manual utility are (thankfully) few and far between. It has been estimated that to achieve significant statistical power based on event rate and effect size, it would require 1.6 million patients over three years and therefore not considered feasible.32
Regardless of the paucity of quality outcome studies, from as early as 2006 simulation studies have repeatedly demonstrated less errors of omission, missteps, improved team performance and decrease clinician anxiety when managing simulated crises.
It seems a small leap of faith to suggest demonstrable benefits in the simulated emergency would be transferrable to real life events.33,35
The future of Cognitive aids and the COVID effect
The last decade has seen the gradual acceptance of checklist cognitive aids into healthcare culture. In contrast, integration of manuals is lagging. In addition to a paucity of outcome study data, perhaps the greatest obstacles to widespread adoption of the crisis or emergency manual have been practitioner cultural bias and the lack of a centralised implementation process using standardised protocols – albeit with scope for local input.32,34
Practitioner bias
Undermining training, autonomy, intellect and skillset have all been arguments used against cognitive aids. This ego driven belief, combined with concern diagnoses may not immediately align with a manual protocol, suggests a misunderstanding of purpose. Manuals are not ‘problem solvers’ but designed to support and complement the knowledge and expertise of those managing the emergency.36
Earlier concerns such as potential interference and delay in time sensitive treatment, impact on communication and protocol fixation error have diminished as simulation studies, familiarisation and training, and national implementation programs have promoted manual use as a ‘positive intellectual skill for every level of anaesthesia providers’ (and an important contributor to patient safety.36
Interestingly, a significant shift in cognitive aid acceptance appeared during the recent SARS-CoV-2 pandemic. It was often suggested by those involved in simulation and emergency manuals, that ‘going down with the plane’ was a strong incentive for pilots to accept regular emergency simulation training and consult the QRH – to use all resources at hand to remain the best one can be.
Although patient safety should be a priority for all healthcare workers, there has not been the same threat to personal wellbeing when managing medical emergencies. It has been suggested that if there was, institutions and individuals would be incentivised to embrace all resources at hand, including cognitive aids, simulation and drill rehearsal.37
During the pandemic, the proliferation in cognitive aids (of varying design quality) for PPE, intubation, extubation, patient transfer and other associated procedures may support this theory. COVID-19 has sharpened clinician priorities and possibly contributed to attitude recalibration. When healthcare worker safety is directly affected and there are daily body counts, media images reminiscent of wartime, and perhaps knowledge of frontline colleagues falling ill, there is strong incentive to make our workplace as safe as possible. Cognitive aids have proven an integral component of protecting HCWs and may be indicative of cultural change.
Implementation
Despite a decade of simulation studies, implementation strategies, collaborations and patient safety declarations, use of perioperative crisis manuals is still not routine. It is well recognised even with a perfectly designed manual placed appropriately; it is often left untouched in crisis management.29,38
There are many components to successful implementation including institutional support and safety culture, local champions, education and training, anecdotal sharing, publicising successful outcomes, as well as practitioner and interprofessional buy-in.
Perhaps the most significant hurdle to routine use is unlike the surgical safety checklist, there has been no centralised and standardised implementation strategy.
To complicate the process, there is variation in content, design, and institutional endorsement, reflecting the piecemeal and often parallel development of cognitive aids across different countries.
As Gaba states, it is surprising that despite several decades, ‘….no international body, has attempted to create a more comprehensive set of perioperative cognitive aids through formal consensus…’ 34
Marshall has expressed a similar sentiment by suggesting ‘….the process currently used for the management of cardiac arrest by the International Liaison Committee on Resuscitation would seem to be the ideal template.’39 Gaba concluded the task must be too daunting ‘logistically, politically, and financially’ and he is probably right. Consensus when attainable is desirable but sometimes ‘benevolent dictatorship’ gets things done.
Instead, institutions and medical societies through different countries have risen to the challenge, supporting local design, education, and collaboration.41.42 The European Society of Anaesthesiology and Intensive Care, The Association of Anaesthetists Great Britain and Ireland, The Stanford Anesthesia Cognitive Aid Group and Ariadne Labs have all produced operating room emergency protocols and checklists.8,9,40 More recently collaboration between these groups and the Emergency Manual Implementation Collaborative (EMIC) have produced online toolkits to help implement cognitive aids.43
Although there is global acceptance of the manual concept, a standard emergency manual acceptable to all is unlikely. In Australia, The Anaesthetic Crisis Manual has gained widespread acceptance as a commercially available ‘ready to go’ product, avoiding the potential hold ups of downloading, printing, laminating and binding freely available internet resources. In addition, it received early institutional support from The Australian Society of Anaesthetists, with all advanced anaesthesia trainees receiving complimentary copies. Along with inclusion in college accredited EMAC simulation courses, institutional support of this kind plays a significant role in cultural change.
Finally, formal inclusion in the surgical safety checklist could enhance visibility and lead to greater use – for example, asking during time out “Is there an emergency manual present? Who will be the designated reader should it be needed?” may prevent the “I didn’t think of it” response.
Integrated cognitive aids and decision support.
It is only logical in the digital age to expect the use of cognitive aids to be transferrable to interactive electronic format. Although electronic formats have been demonstrated44, recognised drawbacks include lack of visibility, accessibility and mobility when navigating workflow dynamics in crisis scenarios.
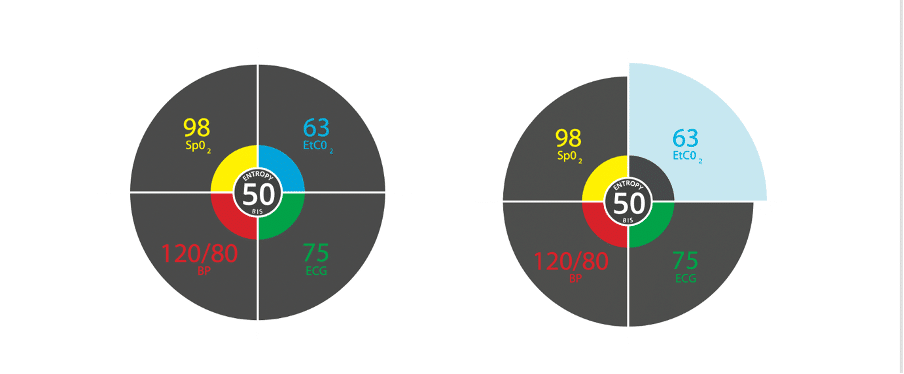
It is likely that just as monitoring, feedback systems and checklists have converged into a prioritised central display unit in modern aircraft (Fig. 7), we are at the beginning of a revolution in healthcare monitoring. As previously alluded to 22, the prospect of integrated decision support systems, guidelines and protocols all in prioritised display units seems inevitable (Fig. 8).
References
- Babcock WW. Resuscitation during anesthesia. Anesthesia and Analgesia. 1924; 3(6): 208-213
- http://www.apa.org/
- Twitter; @edexam 5.7.21
- Boeing 299 Flying Fortress; ASN Wikibase Occurrence # 83555. Aviation Safety Network
- The case of Elaine Bromiley. CHFG
- Gawande A. The Checklist Manifesto: How to Get Things Right. New York, NY Metropolitan Books 2009
- Borshoff D.C. The Anaesthetic Crisis Manual. 2011 Perth, Australia. Leeuwin Press. www.leeuwinpress.com.au
- Stanford Anesthesia Cognitive Aid Group. Emergency Manual: Cognitive Aids for perioperative clinical events. Stanford Medicine
- Ariadne Labs launches online toolkit to help surgical teams implement OR Crisis Checklists. Ariadne Labs 2017
- Gaba DM, Fish KJ, Howard SK. Crisis Management in Anesthesiology. New York, NY Churchill Livingstone, 1994
- Runciman WB, Sellen A, Webb RK. Errors, incidents and accidents in anaesthetic practice. Anaesth Intens Care 1993; 21: 506–519.
- Emergency Management of Anaesthetic Crises (EMAC)
- Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. N Engl J Med 1991; 324:370 – 376.
- Wilson RM, Runciman WB, Gibberd RW, Harrison BT, Newby L, Hamilton JD. The Quality in Australian Health Care Study. Med J Aust. 1995 Nov 6;163(9):458-71
- Mellin-Olsen J, Staender S, Whitaker DK, Smith AF. The Helsinki Declaration on Patient Safety in Anaesthesiology. Eur J Anaesthesiol. 2010 Jul;27(7):592-7.
- McLachlan G. WHO’s surgical safety checklist: it ain’t what you do… BMJ. 2019 May 20;365:l2237.
- Grigg E. Smarter Clinical Checklists: How to Minimize Checklist Fatigue and Maximize Clinician Performance Anaes Analg 2015; 121(2): 570-573
- Vital K, Cornwell B, Arkin N, Grillon C, Describing the interplay between anxiety and cognition: From impaired performance under low cognitive load to reduced anxiety under high load. Psychophysiology 2012 Jun; 49(6): 842–852.
- Degani A. Cockpit Checklists: Concepts, Design and Use. Human Factors 1993; 35(2), pp.28-32
- Ziewacz JE, Arriaga AF, et al. Crisis checklists for the operating room: development and pilot testing. J Am Coll Surg. 2011 Aug;213(2):212-217.e10.
- Arriaga AF, Bader AM, Wong JM, Lipsitz SR, Berry WR, Ziewacz JE, Hepner DL, Boorman DJ, Pozner CN, Smink DS, Gawande AA. Simulation-based trial of surgical-crisis checklists. N Engl J Med. 2013 Jan 17;368(3):246-53.
- Marshall SD. Helping experts and expert teams perform under duress: an agenda for cognitive aid research. Anaesthesia 2017; 72: 283-295
- A Checklist for Checklists. Ariadne Labs; accessed 14.8.21
- Gordon K. Using Color to Enhance Your Design. Nielsen Norman Group, 2021
- Fessenden T. Aesthetic and Minimalist Design (Usability Heuristic #8). Nielsen Norman Group, 2021
- Alidina, S., Goldhaber-Fiebert, S.N., Hannenberg, A.A. et al. Factors associated with the use of cognitive aids in operating room crises: a cross-sectional study of US hospitals and ambulatory surgical centers. Implementation Sci 2018; 13: 50
- Calder LA, Bhandari A, Mastoras G, Day K, Momtahan K, Falconer M, Weitzman B, Sohmer B, Cwinn AA, Hamstra SJ, Parush A. Healthcare providers’ perceptions of a situational awareness display for emergency department resuscitation: a simulation qualitative study. Int J Qual Health Care. 2018 Feb 1;30(1):16-22
- Hall, C., Robertson, D., Rolfe, M. et al. Do cognitive aids reduce error rates in resuscitation team performance? Trial of emergency medicine protocols in simulation training (TEMPIST) in Australia. Hum Resour Health 2020; 18: 1
- Goldhaber-Fiebert SN, Bereknyei Merrell S, Agarwala AV, De La Cruz MM, Cooper JB, Howard SK, Asch SM, Gaba DM. Clinical Uses and Impacts of Emergency Manuals During Perioperative Crises. Anesth Analg. 2020 Dec;131(6):1815-1826.
- Haugen AS, Wæhle HV, Almeland SK, Harthug S, Sevdalis N, Eide GE, Nortvedt MW, Smith I, Søfteland E. Causal Analysis of World Health Organization’s Surgical Safety Checklist Implementation Quality and Impact on Care Processes and Patient Outcomes: Secondary Analysis From a Large Stepped Wedge Cluster Randomized Controlled Trial in Norway. Ann Surg. 2019 Feb;269(2):283-290.
- https://www.safetyandquality.gov.au/our-work/communicating-safety/patient-identification/patient-procedure-matching-protocols/surgical-safety-checklist accessed 15.8.21
- Morrell RC, Cooper JB. APSF Sponsors Workshop on implementing Emergency Manuals. APSF Newsletter; February 2016.
- Draycott T, Sibanda T, Owen L, Akande V, Winter C, Reading S, Whitelaw A. Does training in obstetric emergencies improve neonatal outcome? BJOG. 2006 Feb;113(2):177-82.
- Gaba, David. Perioperative Cognitive Aids in Anesthesia: What, Who, How, and Why Bother?. Anesth Analg. 2013;117(5):1033-1036.
- Boet S, Bould MD, Fung L, Qosa H, Perrier L, Tavares W, Reeves S, Tricco AC. Transfer of learning and patient outcome in simulated crisis resource management: a systematic review. Can J Anaesth. 2014 Jun;61(6):571-82.
- Simmons WR, Huang J. Operating Room Emergency Manuals Improve Patient Safety: A Systemic Review. Cureus. 2019 Jun 12;11(6):e4888. doi: 10.7759/cureus.4888. PMID: 31423368; PMCID: PMC6689479.
- Borshoff DC, Sadleir P. Nonoperating room anaesthesia: safety, monitoring, cognitive aids and severe acute respiratory syndrome coronavirus 2. Curr Opin Anaesthesiol. 2020;33(4):554-560.
- Urman RD, August DA, Chung S, Jiddou AH, Buckley C, Fields KG, Morrison JB, Palaganas JC, Raemer D. The effect of emergency manuals on team performance during two different simulated perioperative crises: A prospective, randomized controlled trial. J Clin Anesth. 2021 Feb;68:110080.
- Marshall, Stuart, MB, ChB. The Use of Cognitive Aids During Emergencies in Anesthesia: A Review of the Literature. Anesth Analg. 2013; 117(5): 1162-1171.
- Quick Reference Handbook (QRH). Association of anaesthetists
- Anaesthetic Crisis Manual. European Society of Anaesthesiology and Intensive Care
- ASA Publications. Australian Society of Anaesthetists
- Emergency Manuals. Emergency Manuals Implementation Collaborative (EMIC)
- Schild S, Sedlmayr B, Schumacher AK, Sedlmayr M, Prokosch HU, St Pierre M; German Cognitive Aid Working Group. A Digital Cognitive Aid for Anesthesia to Support Intraoperative Crisis Management: Results of the User-Centered Design Process. JMIR Mhealth Uhealth. 2019 Apr 29;7(4):e13226.
This article was peer reviewed by A/Prof Chris Nickson (24 August 2021)