CT Case 103
A 35 year old male presents with recurrent episodes of spontaneous bleeding from his right ear. He has no significant medical background and takes no regular medications. He denies tinnitus, hearing loss, trauma, or infective symptoms.
On exam he is found to have a small pulsatile cystic lesion on his right antitragus, and his external auditory canal is filled with dried blood. Following examination he developed persistent haemorrhage from this auditory canal
A CT angiogram of his head and neck is arranged
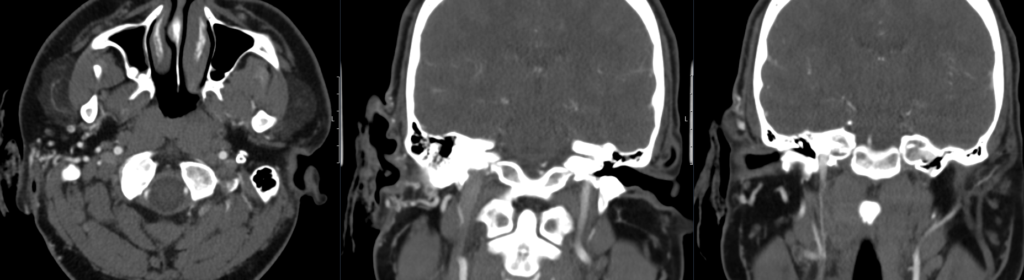
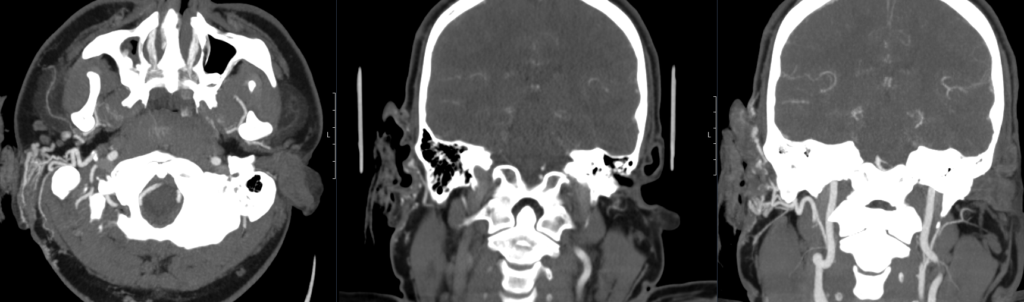
Describe and interpret the CT scan
There appears to be a right ear arteriovenous malformation (AVM) arising from branches of the right external carotid artery. There is probably active bleeding occurring posterior to the antitragus at the time of the scan on axial image 340. Specialist ENT review without undue delay is suggested.
The internal and external carotid arteries and vertebral arteries are seen to fill. No significant stenosis is seen at the origins of the internal carotid arteries.
The M1 and M2 branches of the middle cerebral arteries, A1 and A2 branches of the anterior cerebral arteries, posterior cerebral arteries, internal carotid arteries and basilar artery are seen to fill.
There is no intraparenchymal arteriovenous malformation seen.
No intracranial arterial aneurysm is identified.
Clinical Pearls
Arteriovenous malformations (AVMs) are rare tangles of blood vessels that allow arteries and veins to communicate directly, bypassing the usual capillary bed. They may involve any organ but are most common in the head and neck region. AVMs can arise from any part of an organ including subcutaneous tissue, muscle, and bone.
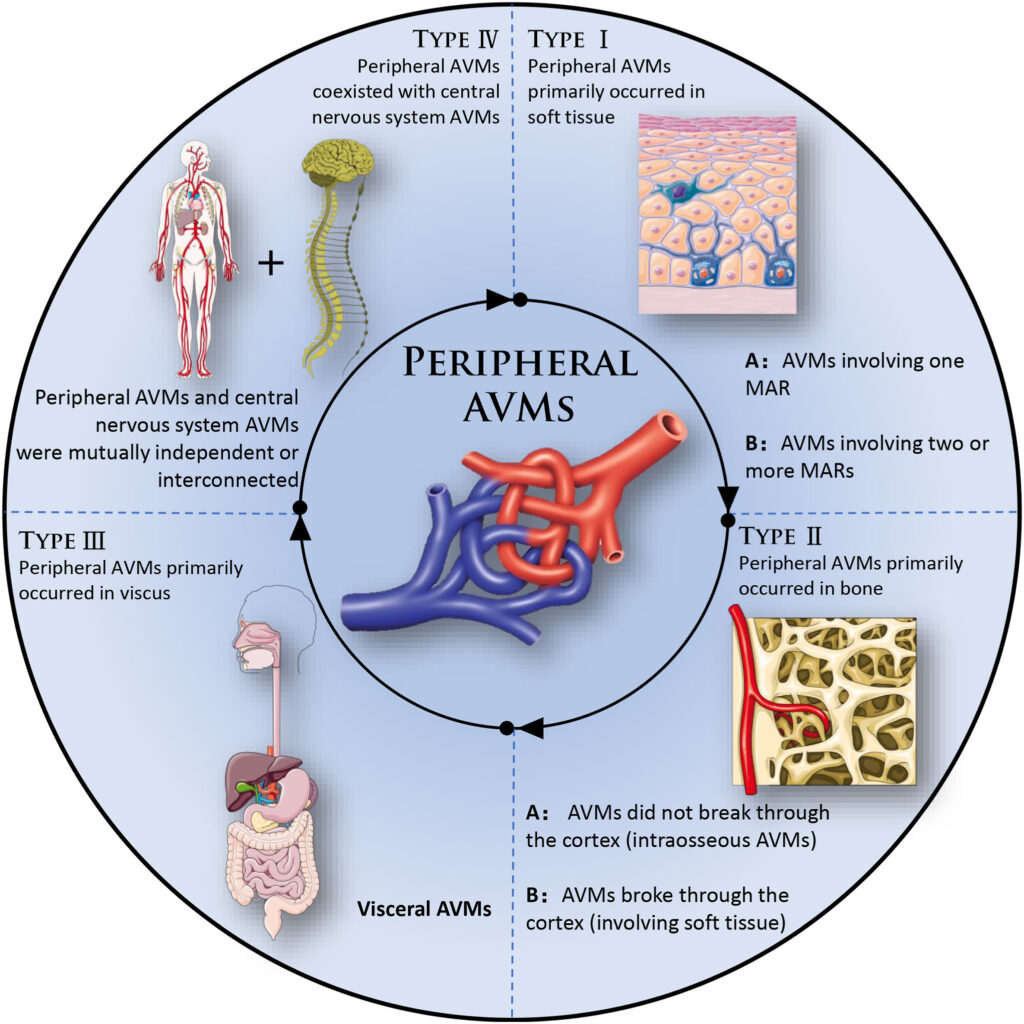
Depending on their location they can present with various signs and symptoms. When the lesion is located near skin or mucosa, a warmish pulsatile blush and swelling may occur, and bruits may be heard. More severe symptoms develop as the lesion progresses such as pain, ulceration, bleeding, and functional impairment. Death is a rare but serious possibility, particularly nasopharyngeal and intracranial AVMs that result in difficult to control haemorrhage.
Treatment often requires a multidisciplinary approach and may involve surgical resection, angioembolisation, laser coagulation, and medical therapy.
This patient was initially managed with tranexamic acid (TXA) soaked gauze to pack the auditory canal and given regular IV TXA. The AVM was considered too large for surgical resection and so he underwent IR guided angioembolisation of the right ear AVM. He continues to have occasional spontaneous bleeds from the right ear due to a large persisting shunt near the AVM, and further embolisation may be required to selectively shut down the bigger shunts.
References
- Shen Y, Su L, Wang D, Fan X. Overview of peripheral arteriovenous malformations: From diagnosis to treatment methods. J Interv Med. 2023 Oct 29;6(4):170-175
TOP 100 CT SERIES
Sydney-based Emergency Physician (MBBS, FACEM) working at Liverpool Hospital. Passionate about education, trainees and travel. Special interests include radiology, orthopaedics and trauma. Creator of the Sydney Emergency XRay interpretation day (SEXI).
Dr Leon Lam FRANZCR MBBS BSci(Med). Clinical Radiologist and Senior Staff Specialist at Liverpool Hospital, Sydney
FACEM, MBBS (Hon), B. Pharm. Emergency Medicine Education Fellow at Liverpool Hospital, Australia. Special interests in clinical education, ECG interpretation and diagnostic ultrasound. Proud father and husband, sadly a golf tragic



