Developing Visual Expertise in ECG Interpretation
Evaluating the Differences in Approach to the ECG Between Experts and Novices
We know that emergency medicine attendings are generally faster and more accurate at ECG interpretation than residents and medical students. But how are they able to process this information so much quicker while maintaining accuracy? And can we use these strategies to help learners progress to their own ‘expert-like’ level?
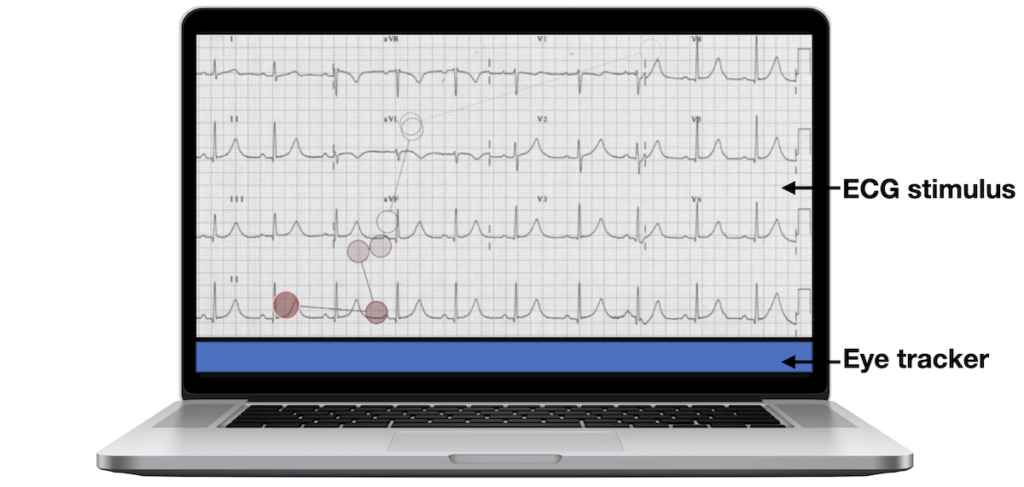
Our study combined eye-tracking and interview data to come up with a few ways in which EM attendings look and think about ECGs differently than more novice learners.1
Dual-process reasoning
Based on Daniel Kahneman’s work Thinking Fast and Slow2, there are two types of thinking: System 1 thinking (unconscious and automatic pattern recognition) vs System 2 thinking (methodical, conscious and analytical search). The vast majority of EM attendings approached ECGs with System 1 thinking, often immediately recognizing an ECG diagnosis within the first few seconds of viewing. It was only when they weren’t able to quickly recognize a pattern on initial impression, or they wanted to double check a specific feature, that the attendings switched to the slower System 2 model of thinking.
I don’t follow an axis, rhythm sort of thing – maybe that’s how I went so fast. You’d think there’s method there, but I’m just sampling but I’m trying to give you my thought process, the conscious part of it. But I’m sure a lot of it was subconscious.
EM Attending
On the other hand, medical students and residents relied almost entirely on System 2 thinking. Many of them stated that they preferred their systematic approach to not miss anything and approached each ECG the same way regardless of their initial impression.
Some of the cardiologists (or in medical school) – they’ll talk about how most computers are better than humans because the computer is trained to do the same thing every time. So, convincing yourself to do the same thing every time is hard, but every ECG should be rate, rhythm – well I think my thing has been just overall gestalt, then rate, rhythm, axis, signs of ischemia, signs of right heart strain, look for blocks, then looking for finer details.
EM Resident
Ability to prioritize
Attendings tended to make very rapid decisions on which features of an ECG were relevant or irrelevant, with the irrelevant findings then quickly deprioritized. Often, this was due to having a preformed differential based on the clinical stem provided beforehand – in essence they knew what to look for before even seeing the ECG.
So initially when I looked at it, the first thing that stood out to me was this baseline that’s kind of rough here, but it was isolated to V1 so I just quickly ignored because that didn’t mean much to me
EM Attending 5
I was thinking about the differential, like I’m going to look for ischemia, I’m going to look for pericarditis, primarily only those two things [based on the stem]
EM Attending 6
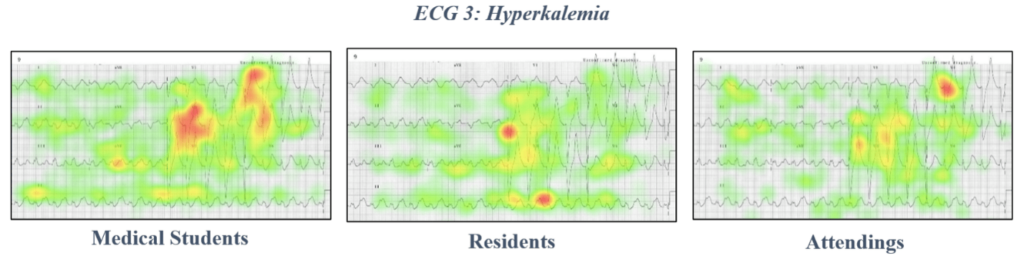
However, medical students spent significant time and effort analyzing numerous notable features of the ECG. This often lead to feelings of being overwhelmed and increased cognitive load.
I definitely saw the peaked T waves, and they’re discordant. I was just trying to remember what that meant though, because I can’t. And then I thought okay I remember this was like that Wellens syndrome had inverted T waves and I was like okay wait no, that’s not it… And then I looked at the other leads and noticed there’s no p waves there and the QRS complexes are very wide, might be ventricular pacing and at one point I considered pericarditis because of the elevations across the board, or what I thought were ST elevations across the board. I think this is one of the ones I had the most trouble with
Medical Student 3
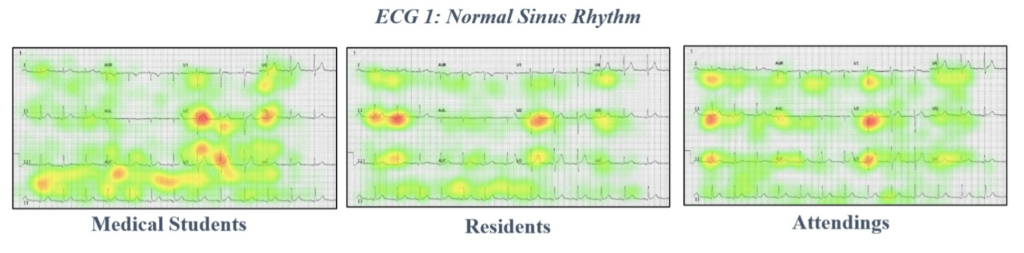
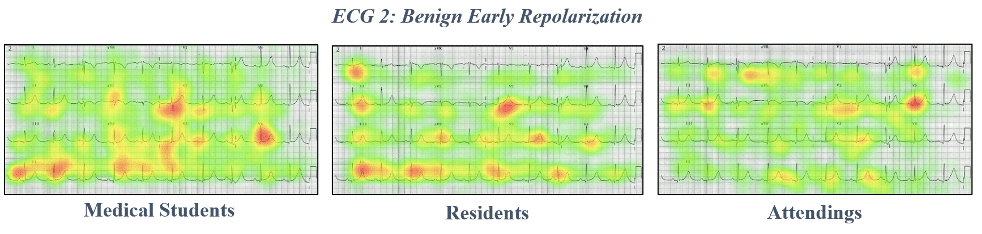
These differences in approach were supported by eye-tracking data showing heat mapping of gaze fixations between EM attendings, EM residents, and medical students. Notice the highly specific focus on narrow areas of interest in the attending heat maps, compared to the widespread focus of more novice learners.
Clinical considerations
Attendings and residents commonly employed practical, real-life strategies to their ECG interpretation. They often focused on ruling out life-threatening pathologies first and emphasized treatment implications when the diagnosis was not clear. They also thought outside of the ECG, asking for things like previous ECGs, bloodwork, and other clinical correlates. Medical students did not mention these considerations.
[T]here’s not enough here, that from a clinical point of view, in the first five minutes of the emergency room, that’s going to make a difference. As I’m writing the admission note, or I’m dealing with the EP fellow, then we can have more of a discussion. But I’ve learned over time, that it’s not going to change my response to that
Attending 8
So what can we learn from this? On one hand, while teaching novices to think more like experts may be the eventual goal of medical education, learners may not have the knowledge base early on in their training to reliably depend on expert-level strategies like pattern recognition. They need to develop the medical expert competence first before the strategies employed by experts offer much value. Of note, a study by Ark et al3 pitted System 1 versus System 2 thinking head-to-head between learners with no prior ECG experience. Interestingly, although there was no significant difference between System 1 versus System 2 learners, the groups that were designed to perform both System 1 and 2 thinking had significantly better results.
Summary
In summary, having knowledge of expert versus novice approaches to the ECG may help learners progress in their individual development of expertise; it may also better inform teachers who are mentoring and evaluating those students. Focus on the expert-like approach may be particularly helpful in times of learning stagnation or in the later stages of medical residency.
References
- Wu W, Hall AK, Braund H, Bell CR, Szulewski A. The Development of Visual Expertise in ECG Interpretation: An Eye-Tracking Augmented Re Situ Interview Approach. Teach Learn Med. 2020 Dec 10:1-20
- Kahneman D, Egan P. Thinking, fast and slow. Farrar, Straus and Giroux; 1st edition (March 1, 2013)
- Ark TK, Brooks LR, Eva KW. Giving learners the best of both worlds: do clinical teachers need to guard against teaching pattern recognition to novices? Acad Med. 2006 Apr;81(4):405-9.
Online ECG Resources
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbook ECG Resources
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
ECG LIBRARY
4th year Canadian medical student from Queen's University. Passionate about FOAMed, rural medicine, and adventuring in the outdoors


Davies et al. first described a dual process to ECG interpretation in 2019 also using interviews and eye-tracking: https://www.magonlinelibrary.com/doi/abs/10.12968/bjca.2019.0073