FFS: Aspiration
Aspiration is the inhalation of oropharyngeal or gastric contents into the lungs. Less commonly, foreign substances (e.g. water, hydrocarbons) may be aspirated, but these are considered distinct clinical entities.
Aspiration is often occult — especially in:
- Elderly nursing home residents
- Patients with decreased consciousness (e.g. overdose, seizures)
A witnessed aspiration event is rarely observed. Clinicians must maintain a high index of suspicion.
Consequences of Aspiration
| Condition | Definition | Key Features |
|---|---|---|
| Aspiration pneumonitis | Acute chemical injury from gastric acid | Symptoms within hours; typically no infection |
| Aspiration pneumonia | Secondary bacterial infection following aspiration event | Symptoms usually ≥48 hrs post-event; may not be witnessed |
In practice, the distinction is often unclear. Management decisions are based on clinical judgement.
Pathophysiology
Mechanisms of Aspiration
- Vomiting (active process)
- Regurgitation (passive process)
- External sources: near-drowning, hydrocarbons
Severity Determinants
- Nature of aspirate:
- pH < 2.5 increases risk of severe pneumonitis
- Particulate or infected material worsens injury
- Volume: ≥0.3 mL/kg (≈20–25 mL in adults)
- Patient comorbidities
Risk Factors
| Category | Examples |
|---|---|
| Airway reflex impairment | ↓ Consciousness (e.g. drugs, seizures), neuromuscular disease, dementia |
| ↑ Gastric volume/pressure | Recent meals, delayed gastric emptying, obstruction |
| Dysphagia pathology | Tracheo-oesophageal fistula, achalasia, strictures, oesophageal tumours |
| Iatrogenic | NGTs, tracheostomy, bag-valve masking in unfasted patients |
Clinical Features
Aspiration is frequently occult. Suspect aspiration in any patient with:
- Predisposing risk factor
- History of vomiting/choking
- Acute respiratory symptoms
Presentations
- Abrupt respiratory distress: cough, wheeze, crepitations, cyanosis
- Occult collapse in elderly, particularly with stroke or dementia
- Status epilepticus, OD, intoxication → silent aspiration
Investigations
Bloods
- FBC, U&Es, glucose, CRP
- ABG/VBG and lactate as indicated
ECG
- Routine for unwell patients, though not specific
CXR
- May be normal in early/low-volume aspiration
- Changes: patchy opacities, usually gravity-dependent
- Most affected lobes:
- Right lower lobe (most common)
- If supine: posterior upper/lower lobes
- If upright: basal lower lobes, right middle lobe, lingula
CT Chest
- More sensitive than CXR
- Common findings:
- Tree-in-bud nodules (airway impaction)
- Ground-glass opacities
- Consolidation ± atelectasis
- Airway plugging
Management
Aspiration Pneumonitis
| Action | Details |
|---|---|
| Airway | Clear oropharynx; suction |
| Oxygenation | NP/mask/rebreather; intubation if hypoxic or unable to protect |
| Antibiotics | Not routinely required unless severe/unwell/aspirated food |
If uncertain, err on the side of treating with antibiotics due to high risk of secondary infection (~25%).
Aspiration Pneumonia
| Action | Details |
|---|---|
| Oxygenation | As above |
| Antibiotics | Required |
Empirical regime:
- Ceftriaxone + Metronidazole
- Particularly if periodontal disease, putrid sputum, necrotising pneumonia, or abscess
Steroids
- No proven benefit in either pneumonitis or pneumonia
Appendix 1
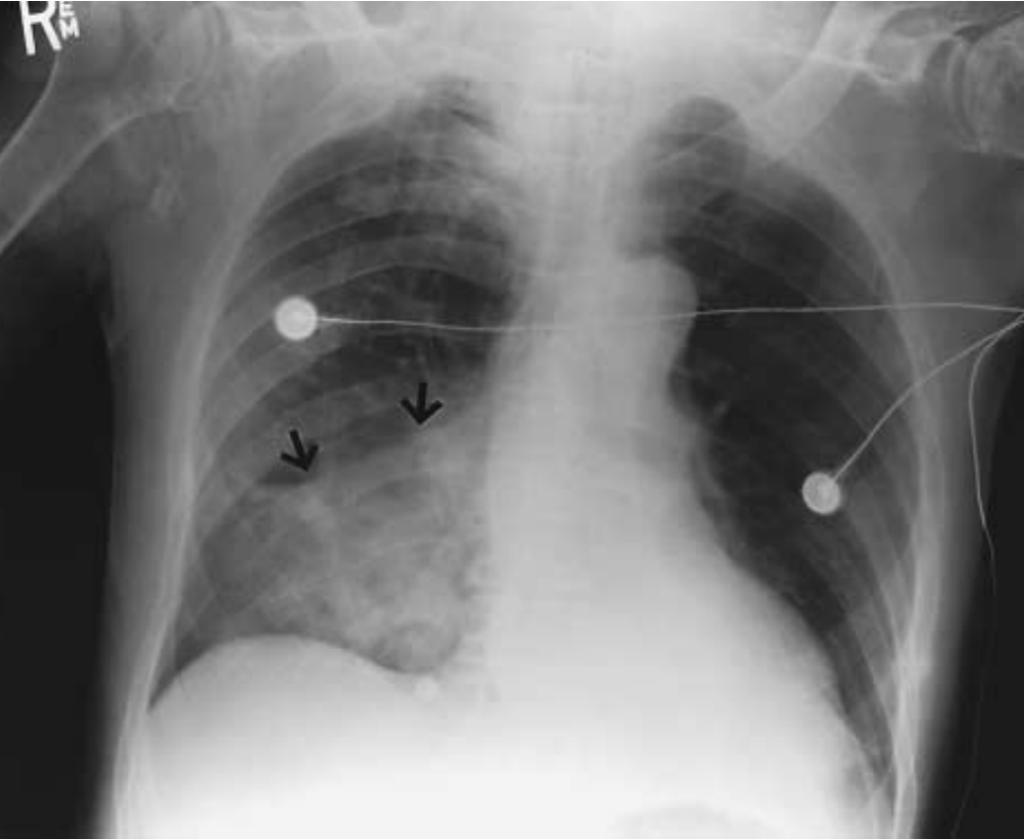
Air-Space Consolidation (Arrows) in the Right Lower Lobe in a
Patient Who Had Recently Had a Thrombotic Stroke. NEJM
References
FOAMed
- Brims F. CXR Case 125. LITFL
- Nickson C. Aspiration Pneumonia. CCC
- Nickson C. Aspiration Pneumonitis. CCC
- Brims F. CXR Case 098. LIYTFL
Resources
- Silverstone L. Aspiration pneumonia. Radiopaedia
- Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med. 2001 Mar 1;344(9):665-71
- O’Connor S. Aspiration pneumonia and pneumonitis. Australian prescriber
Fellowship Notes
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |

