Funtabulously Frivolous Friday Five 338
Just when you thought your brain could unwind on a Friday, you realise that it would rather be challenged with some good old fashioned medical trivia FFFF, introducing the Funtabulously Frivolous Friday Five 338
Question 1
You decide to spend several months at the Siroka University Medical Center of Ben-Gurion University in Israel to experience first-hand the types of medical emergencies in that part of the world. It is summer. You are surprised when you see three children admitted from the emergency room with painful faecal impactions over a month or so.
The only history elicited is that each of these children, who are Bedouin and are 5 to 9 years of age, had been eating the ripe fruit from a particular plant found in the region.
What is your diagnosis as to the cause of the painful faecal impaction?
Reveal the funtabulous answer
Ingestion of Opuntia Ficus Indica
A well-defined clinical entity in the Middle East is faecal impaction because of eating cactus seeds from the ingestion of prickly pears (Opuntia Ficus Indica).
At the above-mentioned medical centre, an average of 2 to 3 children are admitted with painful faecal impactions each summer after the ingestion of prickly pears. This cactus is common in Israel; in the summertime, the fruits of the cactus are ripe. As a rule, the problem affects children of Bedouin origin, and symptoms begin 1 to 2 days after eating large amounts of cactus fruit. The consequence is painful faecal impaction, low abdominal pain, difficulty walking, and occasional rectal bleeding. A foul odour usually emanates from the child. Abdominal examination frequently shows left lower quadrant tenderness, and the outline of a tender left colonic loop.
Rectal examination is excruciating and will demonstrate dense granular masses. Treatment consists of the evacuation of these masses under general anaesthesia. The procedure itself often causes rectal bleeding. Some children require a second procedure because of the large amounts of seeds continuing to reach the rectum.
Cactuses found in the Middle East originated in the Western hemisphere and the West Indies.
After the discovery of the Americas, cactuses were introduced to many countries around the world. There are more than 1500 species in the cactus family. Opuntia Ficus Indica is a widely-cultivated species and grows well around the Mediterranean basin, in Mexico, Australia, and South Africa, flowering in the spring. The 80 to 90 days after flowering are a period of fruit growth and ripening. The cactus pear is a medium-sized (100 to 200 g), oblong, greenish fruit consisting of a firm peel and a soft pulp. The peel is covered with small spines (glochids). The pulp contains 50 to 300 seeds, 1 to 2 mm in size.
The pulp is variously green, yellow, and red and is usually eaten with the tiny seeds. Fruit juices, concentrates, jams, jellies, alcoholic drinks, and sweet cheese are made from this fruit, mainly in Mexico. It has medicinal benefits, including; control of diabetes mellitus, reduction of triglyceride and cholesterol levels, and improving prostatic function. The pears of Opuntia Ficus Indica are delicious and are served cold as a dessert (after removing the prickly peel).
The rub with the cactus pear is that since it is so good to eat, children in certain parts of the world will ingest large amounts of the pear without any other food. The soft pulp is readily digested in the gastrointestinal tract, but the seeds reach the colon. After water absorption, the faecal mass consists of a dense matrix of innumerable seeds mixed with small amounts of faeces. Spontaneous defecation is impossible because of severe rectal pain. If there is a lesson to be learned about eating cactus pears, it is to eat no more than five fruits at any one time and then preferably only as a dessert after the main meal.
Reference:
- Kleiner O, Cohen Z, Mares AJ. Low colonic obstruction due to Opuntia ficus indica seeds: the aftermath of enjoying delicious cactus fruits. Acta Paediatr. 2002;91(5):606-7
Question 2
The commonly used phrase “to blow smoke” up a certain part of the anatomy. The question is, is there such a medical procedure, or has there ever been one?
Reveal the funtabulous answer
Yes. Tobacco smoke enemas have been used therapeutically.
The notion of reviving victims of drowning accidents with tobacco smoke enemas may seem a bit odd, but to 18th-century physicians, this approach was entirely rational. The mainstay of treating the “apparently dead” was warmth and stimulation. Rubbing the skin was one method of stimulation, but injecting tobacco smoke into the rectum was generally thought to be more powerful. Since its introduction from the New World by Sir Walter Raleigh, tobacco has had a place in pharmacopeia for its warming and stimulating properties. This was nothing new, Indigenous Americans had been using tobacco for medicinal purposes long before Europeans showed up their shores.
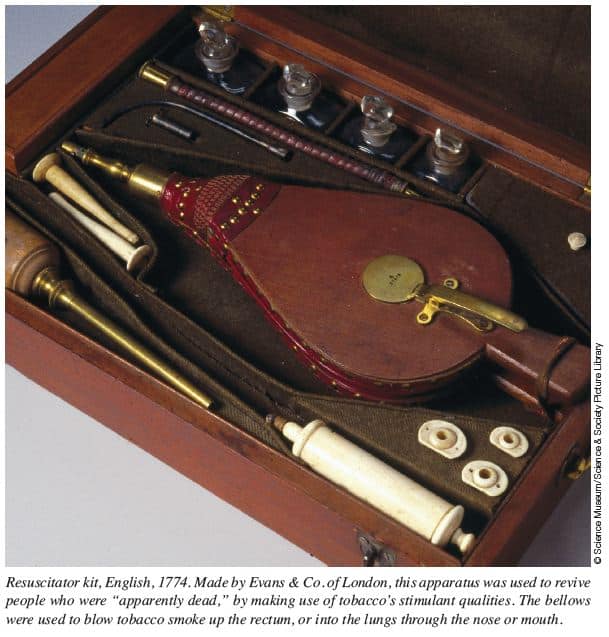
The standard resuscitation kit of the 18th century was designed to allow tobacco smoke enemas to be performed. Such kits consisted of bellows, tubing, nasal or tracheal airways, rectal pipes, and various medications. One of the earliest and most graphic accounts of resuscitation by tobacco enema dates from 1746. A woman was pulled from a pond, apparently dead. Amid much conflicting advice, a passing sailor proffered his pipe and instructed the husband of the woman to insert the stem into his wife’s rectum, cover the bowl with a piece of perforated paper, and “blow hard’. Miraculously, the woman survived.
Before bellows were included in the resuscitation kit the risks to the provider were considerable. At the time cholera was on the therapeutic guidelines for tobacco enemas and if the medic inadvertently inhaled during a coughing spell, rice water stool of cholera flagellates could be aspirated causing the demise of the provider some days later.
Drs William Hawes and Thomas Cogan who practiced medicine in London, England, founded the Institution for Affording Immediate Relief to Persons Apparently Dead from Drowning in 1774. Sounds like something from Monty Python. In the 18th century, the society paid 4 guineas (about $160 today) to anyone who brought a drowning victim back to life. It eventually became the Royal Humane Society and is still sponsored by Her Majesty the Queen of England. The Royal Humane Society still grants awards for acts of bravery in the saving of human life and also for the restoration of life by resuscitation.
Of course, tobacco enemas fell into disfavor, probably around 1800. Resuscitation subsequently involved gymnastics of external body compression systems, not to be replaced until the onset of mouth-to-mouth techniques around 1959.
To read the history of tobacco smoke enemas and other primitive resuscitation techniques, see the excellent review by Lawrence
Reference:
- Lawrence G. Tobacco smoke enemas, tools of the trade. Lancet 2002; 359: 1442
- Haynes S. Special Feature: Tobacco smoke enemas. BCMJ 2012;54(10):496-497
- Nickson C. Ever tried smoking? LITFL
Question 3
You are seeing a 7-year-old boy with complaints of a chronic cough. The history indicates that 4 years previously, he underwent a right-sided tympanoplasty for cholesteatoma. He had no postoperative complications or recurrences.
About 1 year later, however, he began to complain of a persistent dry cough that was present both day and night. By the time you see him, he has had several studies of the upper and lower respiratory tracts, including repeated chest radiographs, CT scans of the sinuses, bronchoscopy, nasobroscopy, and allergic screening. Additionally, a CT scan of the head has been performed as well as a psychological evaluation to exclude a psychogenic origin for his cough. None of these tests have been remarkable.
When you see the youngster, he continues to have recurring complaints of a dry cough of several years’ duration. There are no other symptoms. The cough is dry. On physical examination, the only finding of note is an accumulation of earwax surrounding a small skin ulceration in a narrowed external auditory canal, the same side he was operated on years before.
When you try to remove the wax, you trigger an episode of coughing. With removal of the wax, lo and behold, the cough disappears, but only for a few weeks. Shortly after recurrence of cough, you note again the fact that you can reproduce the cough with attempts to remove earwax.
Your diagnosis?
Reveal the funtabulous answer
Ear-cough reflex.
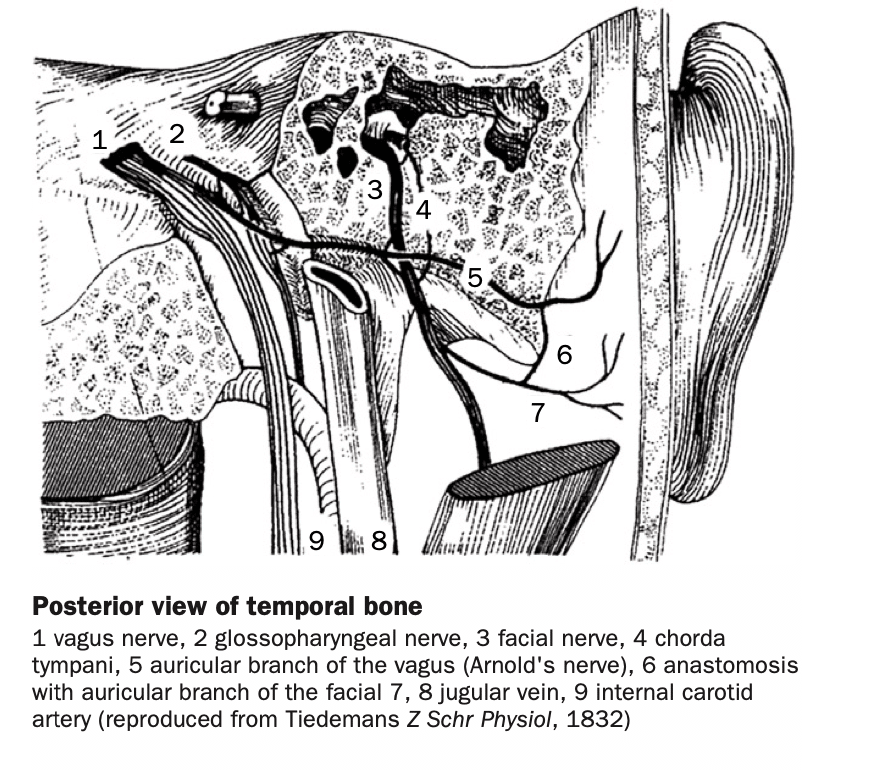
The ear-cough reflex was first described in 1832 by Friedrich Arnold (1803-1890) and was reported by Itard again in 1842. Its incidence ranges from 1.7% to 4.2% of the population at one time or another our lifetime.
If you recall your neuroanatomy, Arnold’s nerve arises from the jugular ganglion of the vagus nerve, emerges through the tympanomastoid fissure, and usually supplies the posterior and inferior meatal skin of the ear. In many normal individuals, an ear-cough reflex can be elicited by stimulation of this nerve. A third of ear-cough reflex cases are elicited by touching the anterior wall of the external auditory meatus and two-third of cases are bilateral.
Some people will vomit or pass out with such maneuvers. Either a foreign body or heavily impacted earwax is the most common pathological cause of the ear-cough reflex.
Remember the ear-cough reflex for those with a chronic cough. The diagnosis may save a patient a bunch of laboratory studies and the otoscope exam is easy and safe.
In the child described above, it was necessary to widen the stenotic ear canal to totally relieve recurrence of symptoms
References
- Feldman JI, Woodworth WF. Cause for intractable chronic cough: Arnold’s nerve. Arch Otolaryngol Head Neck Surg 1993;119:1042
- Jegoux F, Legent F, Beauvillain de Montreuil C. Chronic cough and earwax. Lancet 2002: 360: 618
- Ryan NM, Gibson PG, Birring SS. Arnold’s nerve cough reflex: evidence for chronic cough as a sensory vagal neuropathy. J Thorac Dis. 2014 Oct;6(Suppl 7):S748-52
- Friedrich Arnold (1803 – 1890)
Question 4
When was pulsus paradoxus first described?
Reveal the funtabulous answer
1863
It was in a manuscript published in 1863 that Adolf Kussmaul described the phenomenon of a paradoxical pulse.
Although pulsus paradoxus is most associated with pericardial tamponade, Kussmaul initially described a patient with constrictive pericarditis (Kussmaul A, Stern M. Pericarditis and the paradox pulse. Berl Klin Wochenschr 1873:38).
In case you have forgotten, the current formal definition of pulsus paradoxus is an inspiratory fall of systolic blood pressure of greater than 10 mm Hg. To measure the inspiratory decrease in blood pressure, the blood pressure cuff is first inflated 20 mm Hg above the systolic pressure, then is deflated until the first Korotkoff sound is heard.
Initially, the Korotkoff sounds are heard only during inspiration. The cuff is deflated until the Korotkoff sounds are heard equally well during inspiration and expiration. The pressure at which all of the Korotkoff sounds are heard should be subtracted from the systolic pressure (i.e. the pressure you first heard a sound). If the difference between these two pressures is greater than 10 mm Hg, the patient has a pulsus paradoxus of a magnitude equal to that difference. A pulsus paradoxus, in addition to being seen in patients with constrictive pericarditis and pericardial tamponade, may be seen in conditions in which the pleural pressure swings are exaggerated or the right ventricle is distended, such as acute pulmonary hypertension, severe asthma, or exacerbations of chronic obstructive pulmonary disease.
By the way, Kussmaul was also the first to describe Kussmaul’s sign, the reversal of the normal pattern of decreasing jugular venous pressure during inspiration. This also is seen with the same disorders that cause a pulsus paradoxus. The mechanism, however, of Kussmaul’s sign is different from that of pulsus paradoxus. During normal inspiration, contraction of the diaphragm increases abdominal pressure, which may have variable effects on the gradient for venous return. With constrictive pericarditis, the increased abdominal pressure increases systemic venous return from the engorged splanchnic bed. Because the right ventricle is noncompliant, the right atrial pressure rises more than the fall in pleural pressure, leading to distention of the neck veins with inspiration.
Reference:
- Kussmaul A. Über schwielige Mediastino-Perikarditis und den paradoxen Puls. Berliner klinische Wochenschrift, 1873; 10: 433-435 [Kussmaul pulse]
- Kussmaul A. Zur Lehre vom Diabetes mellitus. Über eine eigenthümliche Todesart bei Diabetischen, über Acetonämie, Glycerin-Behandlung Diabetes und Einspritzungen von Diastase in Blut bei dieser Krankheit. Deutsches Archiv für klinische Medicin. 1874;14:1-46. [Kussmaul respiration]
- Major RH. A peculiar mode of death in diabetes (translation) In: Classic Descriptions Of Disease. 1945: 245-249 [Kussmaul respiration]
- Adolph Kussmaul (Adolf Kußmaul) (1822 – 1902)
Question 5
Just how far can head lice jump?
Reveal the funtabulous answer
Not very far, if at all
Head lice are surprisingly bad at jumping.
An in vitro study of 480 freshly caught head louse from school children has shown that when hair is rubbed for a second or two against a head louse sitting on another hair, the louse transfers to the second hair only about 7% of the time. When it does transfer, it grabs the hair with one leg and is more likely to do so if the hair is rubbed along the louse’s lateral surface.
This study affirms that you really need head-to-head contact to transfer lice from one recipient to another and it does not support the hypothesis that head lice are able to transfer from head-to-head by the slightest bodily contact.
Reference
- Canyon D et al. Spatial and Kinetic Factors for the Transfer of Head Lice (Pediculus capitis) Between Hairs. Journal of Investigative Dermatology. 2002;119(3):629-631
…and Finally

FFFF
Funtabulously Frivolous Friday Five
Dr Neil Long BMBS FACEM FRCEM FRCPC. Emergency Physician at Kelowna hospital, British Columbia. Loves the misery of alpine climbing and working in austere environments (namely tertiary trauma centres). Supporter of FOAMed, lifelong education and trying to find that elusive peak performance.