Guido Fanconi
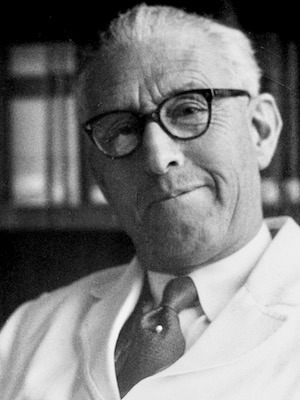
Guido Fanconi (1892–1979) was a Swiss paediatrician
Fanconi served for over three decades as director of the Kinderspital Zürich, transforming it into one of the world’s foremost centres for paediatric care and research. His holistic approach to medicine blended bedside observation with pathophysiological reasoning, laying the groundwork for modern paediatric nephrology, haematology, and medical genetics.
Fanconi is best remembered for first describing Fanconi anaemia (1927), an inherited bone marrow failure syndrome and Fanconi syndrome, a proximal tubular disorder leading to rickets and solute wasting. He is also eponymously linked with Fanconi–Bickel syndrome (a hepatic-renal glycogenosis), Fanconi–Zellweger syndrome, and several inherited thrombocytopathies later reclassified under MYH9-related disease.
Biographical Timeline
- Born January 1, 1892 in Poschiavo, Canton Grisons (Graubünden), Switzerland.
- 1905 – Moved to Schiers (German-speaking region) for better education.
- 1911 – Completed school-leaving certificate (Matura); began medical studies in Lausanne, then studied in Munich, Zurich, and Bern.
- 1918 – Graduated MD from the University of Bern.
- 1920-1926 – Training in paediatrics at Kinderspital Zürich under Emil Feer-Sulzer (1864-1955). Completed doctoral thesis: Fünf Fälle von angeborenem Darmverschluss.
- 1922 – Spent a year in biochemistry at Prof. Emil Abderhalden’s lab in Halle.
- 1926 – Completed Habilitationsschrift on scarlet fever.
- 1927 – Described hereditary panmyelopathy now known as Fanconi anaemia.
- 1929 – Appointed Director of the Kinderspital Zürich and Professor of Paediatrics, University of Zurich.
- 1930 – Advocated raw fruit (pectin) therapy for diarrhoea at 2nd International Pediatric Congress in Stockholm.
- 1934 – First documented cases of cystic fibrosis of the pancreas in a student’s thesis under his supervision.
- 1936 – Published description of what became Fanconi syndrome (De Toni–Debré–Fanconi syndrome).
- 1941 – Identified gastrointestinal, not droplet, transmission of poliomyelitis during Swiss epidemic.
- 1945 – Founded the journal Helvetica Paediatrica Acta (absorbed by the European journal of pediatrics in 1988).
- 1947–1950 – Served as President of the International Pediatric Association.
- 1951–1967 – Served as Secretary-General of the International Pediatric Association.
- 1963 – Retired as Director of Kinderspital after 34 years in the role.
- 1965 – Official retirement from University of Zurich professorship.
- Died October 10, 1979 in Poschiavo, aged 87, after a prolonged illness.
Medical Eponyms
Fanconi Anaemia (1927)
Fanconi anaemia (FA) is a rare inherited disorder characterised by progressive bone marrow failure, congenital malformations, and increased cancer susceptibility, especially to acute myeloid leukaemia (AML) and squamous cell carcinomas. FA is caused by mutations in genes of the FA/BRCA DNA repair pathway, resulting in defective repair of DNA interstrand crosslinks. The diagnostic hallmark is chromosomal breakage in response to crosslinking agents such as diepoxybutane or mitomycin C.
1927 – Fanconi first described the condition in three brothers who exhibited pancytopenia, short stature, microcephaly, and skin pigmentation abnormalities. He referred to it as “Familiäre, infantile perniciosähnliche Anämie“ (familial infantile pernicious-like anaemia).
The eponym Fanconi anaemia entered widespread clinical use by the 1950s, distinguishing it from other causes of aplastic anaemia and dysmorphic syndromes.
Subsequent research throughout the 20th century revealed the genetic heterogeneity of FA. More than 23 complementation groups (FANC genes) have been identified, with FANCA, FANCC, and FANCG being the most common. The FA/BRCA pathway has become a key model in DNA repair research.
Modern management:
- Supportive care: blood transfusions, infection prophylaxis
- Hematopoietic stem cell transplantation (HSCT): curative for marrow failure
- Cancer surveillance: essential due to high risk of AML and solid tumours
- Genetic counselling: for family risk assessment
- Molecular diagnosis: FA diagnosis confirmed via chromosomal breakage tests and sequencing of FANC genes; fibroblast testing helps identify somatic mosaicism
De Toni–Debré–Fanconi Syndrome [Fanconi syndrome] (1936)
De Toni–Debré–Fanconi syndrome (Fanconi syndrome) is a rare disorder of the proximal renal tubule characterised by impaired reabsorption of glucose, phosphate, bicarbonate, amino acids, and other solutes, leading to polyuria, growth failure, hypophosphataemic rickets, metabolic acidosis (type II RTA), and electrolyte disturbances.
1933 – Giovanni De Toni (1895–1973) First reported the association between renal dwarfism and glycosuria in a case of renal rickets.
1934 – Robert Debré (1882–1978) and colleagues published a French case “Rachitisme tardif coexistant avec une néphrite chronique et une glycosurie” with chronic nephritis, glycosuria, and rickets, further characterising the clinical picture.
1936 – Fanconi reported a more detailed and widely cited description of three children with growth retardation, glycosuria, phosphaturia, aminoaciduria, and hypophosphatemic rickets with “Der frühinfantile nephrotisch-glycosurische Zwergwuchs mit hypophosphatämischer Rachitis” (early infantile nephrotic-glycosuric dwarfism with hypophosphataemic rickets).
1940s – The term “Fanconi syndrome” had gained generalised use to describe any form of proximal renal tubular dysfunction, regardless of its underlying cause. The broader application of the term increasingly supplanted the full eponym “De Toni–Debré–Fanconi syndrome” in routine clinical practice.
Modern understanding of Fanconi syndrome:
Aetiology: Fanconi syndrome can be inherited or acquired:
- Inherited causes include: Cystinosis, Lowe syndrome, Wilson disease, galactosaemia, tyrosinaemia, and mitochondrial cytopathies
- Acquired causes include: Drug-induced toxicity (e.g., ifosfamide, tenofovir); heavy metal exposure (e.g., lead, cadmium); and post-transplant and light-chain associated proximal tubulopathies
Diagnosis: Typically presents in early childhood with polyuria, growth failure, rickets, and developmental delay. Diagnosis is based on the following findings:
- Genetic testing: increasingly used to identify inherited forms, particularly in cystinosis and Lowe syndrome
- Urinalysis: glycosuria (with normal blood glucose), aminoaciduria, phosphaturia, bicarbonaturia
- Serum studies: hypophosphataemia, metabolic acidosis, hypokalaemia
- Imaging: signs of rickets (e.g. metaphyseal cupping/fraying)
- Functional testing: bicarbonate loading test confirms type II (proximal) renal tubular acidosis
Management:
- Electrolyte and fluid replacement: phosphate, bicarbonate, potassium
- Vitamin D analogues: to support bone mineralisation
- Disease-specific therapy: e.g., cysteamine in cystinosis
- Surveillance: renal function, bone health, growth
- Avoidance of nephrotoxins in acquired cases
Fanconi–Bickel Syndrome (1949)
Fanconi–Bickel syndrome (FBS) is a rare autosomal recessive disorder classified as glycogen storage disease type XI (GSD XI). It combines features of hepatic glycogen accumulation with renal tubular dysfunction, most notably Fanconi syndrome. The condition is caused by mutations in the GLUT2 (SLC2A2) gene, which encodes the facilitative glucose transporter primarily expressed in the liver, kidney, pancreas, and intestine.
1949 – Fanconi and Horst Bickel (1918–2000) described a child with hepatomegaly, severe growth retardation, fasting hypoglycaemia, postprandial hyperglycaemia and glucosuria, rickets, and aminoaciduria. [Die chronische Aminoacidurie (Aminosäurediabetes oder nephrotisch-glukosurischer Zwergwuchs) bei der Glykogenose und der Cystinkrankheit (Chronic aminoaciduria (amino acid diabetes or nephrotic-glucosuric dwarfism)]
Pathophysiology: GLUT2 deficiency impairs glucose transport in hepatocytes and renal tubular cells. This results in:
- Hepatic glycogen storage → hepatomegaly, fasting hypoglycaemia, postprandial hyperglycaemia
- Renal tubular dysfunction → glucosuria, phosphaturia, aminoaciduria, bicarbonaturia
- Growth retardation, rickets, and hypophosphataemia
Diagnosis:
- Biochemical profile: fasting hypoglycaemia with elevated postprandial glucose, glucosuria with normoglycaemia, electrolyte losses
- Liver biopsy (historically): glycogen accumulation without enzyme deficiency
- Genetic testing: pathogenic mutations in SLC2A2 gene (chromosome 3q26.1–q26.3)
Modern management:
- Nutritional support: frequent feeds with slow-release carbohydrates or uncooked cornstarch to prevent hypoglycaemia
- Electrolyte and bicarbonate replacement for proximal tubulopathy
- Vitamin D and phosphate supplementation for rickets
- Liver monitoring: hepatomegaly often improves with age
- Genetic counselling
Fanconi–Zellweger Syndrome (Obsolete)
Fanconi–Zellweger syndrome is an archaic eponym once used to describe a constellation of findings now understood to belong to the Zellweger spectrum disorders (ZSDs), a group of peroxisomal biogenesis disorders caused by mutations in the PEX gene family. These syndromes are autosomal recessive and typically present in the neonatal period with severe hypotonia, craniofacial dysmorphism, hepatomegaly, seizures, and early death.
1948 – Fanconi–Zellweger syndrome or Fanconi–Albertini–Zellweger syndrome, refers to early attempts to classify severe neurodegenerative infantile syndromes. Hans-Ulrich Zellweger (1909-1990), a student of Fanconi, helped clarify the phenotype with detailed neuropathological and biochemical analysis.
The eponym fell out of favour as the biochemical basis of peroxisomal disorders was elucidated, particularly with advances in peroxisomal enzyme assays and PEX gene identification in the 1980s–1990s. These conditions are now grouped under the Zellweger spectrum, which includes:
- Zellweger syndrome (most severe)
- Neonatal adrenoleukodystrophy
- Infantile Refsum disease
Fanconi–Hegglin / Fanconi–Patrassi Syndrome (Obsolete)
Fanconi–Hegglin and Fanconi–Patrassi syndromes were historical eponyms describing inherited macrothrombocytopenias with abnormal platelet morphology and function. Patients presented with mild bleeding tendencies, giant platelets, and sometimes leukocyte inclusion bodies. These syndromes are now recognised as part of the MYH9-related disease spectrum, a group of autosomal dominant disorders caused by mutations in the MYH9 gene encoding non-muscle myosin heavy chain IIA.se.
Many such cases are now recognised as part of the MYH9-related disorders, which include:
- May–Hegglin anomaly
- Sebastian syndrome
- Fechtner syndrome
- Epstein syndrome
These disorders involve mutations in the MYH9 gene encoding non-muscle myosin heavy chain IIA, and are characterised by:
- Macrothrombocytopenia
- Döhle-like inclusion bodies in neutrophils
- Variably associated with hearing loss, renal disease, and cataracts
Wissler–Fanconi Syndrome (1944–1946) (Obsolete)
Wissler–Fanconi syndrome (Also known as: Subsepsis hyperergica, Subsepsis allergica Wissler) was a historical eponym used to describe a systemic inflammatory syndrome seen in children and adolescents, featuring intermittent fever, exanthema, leukocytosis, arthralgia, and carditis. Though initially proposed as a distinct clinical entity, it is now understood to overlap significantly with systemic juvenile idiopathic arthritis (sJIA) and acute rheumatic fever, and is no longer recognised as a separate diagnosis.
Landsteiner–Fanconi–Andersen Syndrome
A rarely used and now obsolete eponym that combined the names of Karl Landsteiner (1868–1943), Fanconi, and Dorothy Hansine Andersen (1901–1963). The term was used historically to describe infantile nephropathies thought to involve immune dysfunction, prior to the delineation of specific glomerulopathies. No longer in clinical use, and likely encompassed what are now better classified as congenital nephrotic syndromes or immune-mediated renal diseases.
Fanconi–Tüerler Syndrome
A historical and extremely rare term, with limited description in the literature. Sometimes associated with gastrointestinal symptoms, failure to thrive, or mucosal pathology in infancy. There is speculation it may have overlapped with or been a misclassification within the cystic fibrosis spectrum or chronic enteropathies. The term has disappeared from modern nosology and lacks a defined clinical entity.
Major Publications
- Fanconi G. Familiäre, infantile perniciosähnliche Anämie (perniziöses Blutbild und Konstitution). Jahrbuch für Kinderheilkunde und physische Erziehung. 1927; 117: 257-280. [Fanconi anaemia]
- Fanconi G. Der frühinfantile nephrotisch-glycosurische Zwergwuchs mit hypophosphatämischer Rachitis. Jahrbuch für Kinderheilkunde. 1936; 147: 299-318. [Abderhalden-Kaufmann-Lignac syndrome] [de Toni-Debré-Fanconi syndrome]
- Fanconi G, Uehlinger E, Knauer C. Das Coeliakiesyndrom bei angeborener zystischer Pankreasfibromatose und bronchiektasien. Wiener medizinische Wochenschrift, 1936; 86: 753-756. [Landsteiner-Fanconi-Andersen syndrome][Clarke-Hadfield syndrome]
- Fanconi G. Die pseudoluetische, subakute hilifugale Bronchopneumonie des heruntergekommenen Kindes. Schweizerische medizinische Wochenschrift, Basel, 1936; 66: 821-826. [Fanconi-Hegglin syndrome]
- Fanconi G. Ueber einen Fall von Subsepsis allergica Wissler [About a case of subsepsis allergica Wissler]. Helv Paediatr Acta. 1946 Oct;1(6):532-7. [Wissler disease]
- Fanconi G, von Albertini A, Zellweger H. Osteopathia acidotica pseudorachitica [Osteopathic acidotica pseudorachitica]. Helv Paediatr Acta. 1948 May;3(2):95-112 [Fanconi-Albertini-Zellweger syndrome]
- Fanconi G, Bickel H. Die chronische Aminoacidurie (Aminosäurediabetes oder nephrotisch-glukosurischer Zwergwuchs) bei der Glykogenose und der Cystinkrankheit [Chronic aminoaciduria (amino acid diabetes or nephrotic-glucosuric dwarfism) in glycogen storage and cystine disease]. Helv Paediatr Acta. 1949 Nov;4(5):359-96. [Fanconi-Bickel syndrome]
- Fanconi G, Hanhart E, von Albertini A, Uhlinger E, Dolivo G, Prader A. Die familiäre juvenile Nephronophthise (die idiopathische parenchymatöse Schrumpfniere) [Familial, juvenile nephronophthisis (idiopathic parenchymal contracted kidney)]. Helv Paediatr Acta. 1951 Feb;6(1):1-49. [Fanconi syndrome I]
- Fanconi G, Turler U. Kongenitale Kleinhirnatrophie mit supranucleären Störungen der Motilität der Augenmuskeln [Congenital cerebellar atrophy with supranuclear disturbance of ocular motility]. Helv Paediatr Acta. 1951 Dec;6(6):475-83. [Fanconi-Turler syndrome]
- Fanconi G. Prader A, Isler W, Lüthy F, Siebenmann R. Morbus Addison mit Hirnsklerosse im Kindesalter. Ein hereditäres Syndrom mit X-chromosomaler Vererbung? Helvetica paediatrica acta. 1963; 18: 480-501. [Addison-Schilder syndrome]
- Fanconi G. Die familiaere panmyelopathie [Familial panmyelopathy]. Schweizerische medizinische Wochenschrift. 1964; 94: 1309-1318. [Fanconi anaemia]
- Fanconi G. Familial constitutional panmyelocytopathy, Fanconi’s anemia (F.A.). I. Clinical aspects. Semin Hematol. 1967 Jul;4(3):233-40.
References
Biography
- Wiedemann HR. Guido Fanconi (1892-1979) in memoriam. Eur J Pediatr. 1979 Nov;132(3):131-2.
- Zellweger H. Guido Fanconi, 1892-1979. J Pediatr. 1980 Apr;96(4):674-5.
- Lobitz S, Velleuer E. Guido Fanconi (1892-1979): a jack of all trades. Nat Rev Cancer. 2006 Nov;6(11):893-8
- Fresquet JL. Guido Fanconi (1892-1979). Historia de la Medicina
Eponymous Terms
- Clarke C, Hadfield G. Congenital pancreatic disease with infantilism. Quarterly Journal of Medicine, Oxford, 1924, 17: 358-364. [Clarke-Hadfield syndrome]
- de Toni G. Remarks on the relation between renal rickets (renal dwarfism) and renal diabetes.
Acta pædiatrica, Stockholm, 1933; 16: 479. [De Toni-Debré-Fanconi syndrome] - Debré R, Marie J, Cleret F, Messiny, R. Rachitisme tardif coexistant avec une néphrite chronique et une glycosurie. Bulletins de la société de pédiatrie de Paris, 1934; 32: 305-316 [De Toni-Debré-Fanconi syndrome]
- Hegglin R. Das Wassermann-positive Lungeninfiltrat. Helvetica Medica Acta 1941; 7: 497 [Fanconi-Hegglin syndrome]
- Wissler H. Über eine besondere Form sepsisähnlicher Krankheiten (Subsepsis hyperergica).
Monatsschrift Kinderheilkunde, Berlin, 1944; 94: 1-15. - Marie J. Robert Debré (1882-1978): l’homme, le médecin, le professeur [Robert Debré (1882-1978): the man, the physician, the professor]. Bull Acad Natl Med. 1982 Dec;166(9):1257-64.
- Manz F, Bickel H, Brodehl J, Feist D, Gellissen K, Geschöll-Bauer B, Gilli G, Harms E, Helwig H, Nützenadel W, et al. Fanconi-Bickel syndrome. Pediatr Nephrol. 1987 Jul;1(3):509-18.
- Soulier J. Fanconi anemia. Hematology Am Soc Hematol Educ Program. 2011;2011:492-7.
- Wu ZH. The concept and practice of Fanconi Anemia: from the clinical bedside to the laboratory bench. Transl Pediatr. 2013 Jul;2(3):112-9.
- Sergi CM, Ravelli A, Pio L. Prof. Dr. Giovanni De Toni-Editorial for the Commemoration of a Pediatric Luminary. Int J Mol Sci. 2025 Mar 30;26(7):3198.
Eponym
the person behind the name
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | On Call: Principles and Protocol 4e| Eponyms | Books |
