Henri Huchard
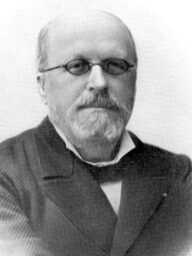
Henri Huchard (1844-1910) was a French cardiologist and neurologist.
Huchard was a leading French physician whose clinical teaching and writing helped define concepts of cardio-arterial disease linking arteriosclerosis, arterial “tension,” and the heart. He systematised bedside signs and advocated rational drug use (digitalis, caffeine/theobromine, nitroglycerin) when the concept of “essential” was established.
Elected to the Académie nationale de médecine, Huchard became an authoritative voice through reference texts (Traité clinique des maladies du cœur) and as founder-director of the Journal des praticiens (1887), popularising practical therapeutics and clinical method. His famed Sunday “Clinique du cœur” at the Hôpital Necker drew physicians from across Europe.
Eponymously remembered by Huchard’s disease (essential hypertension); Huchard’s sign (abnormal heart-rate response in the supine hypertensive) and Syndrôme de Huchard (precordial catch syndrome).
Biographical Timeline
- Born on April 4, 1844 in Auxon, (Aube), France.
- 1871 – Studies of variola (smallpox) myocarditis during the 1870–71 war; thesis on myocardite varioleuse earns faculty prize.
- 1872 – MD, University of Paris
- 1876 – Médecin des hôpitaux, Paris.
- 1883 – Co-authors Traité des névroses with Alexandre Axenfeld (1825–1876)
- 1884 – Elected Académie nationale de médecine and awarded the Godard Prize for work on angina pectoris
- 1886–1888 – Publications on cardio-arterial disease, arteriosclerosis, arterial tension, and therapeutics (digitalis, caffeine, theobromine, nitroglycerin).
- 1887-1910 Director of publication of the journal Revue générale de clinique et de therapeutique: journal des praticiens; becomes a leading voice in French clinical and therapeutic teaching.
- 1889 – Publishes first edition of Maladies du coeur et des vaisseaux which quickly becomes a standard cardiology reference text.
- 1893 – Describes “précordialgie” (Syndrôme de Huchard); expands clinical semiology of chest pain.
- 1896 – Appointed physician to the Necker Hospital; renowned Sunday “Clinique du cœur” teaching sessions.
- 1901 – Publishes Consultations médicales clinique et thérapeutique
- 1908 – Publishes Les maladies du cœur et leur traitement, consolidating therapeutic approach to cardio-arterial disease.
- Died on December 1, 1910 in Clamart, aged 66; obituaries highlight him as a pre-eminent clinician, therapeutic innovator, and medical journalist.
Medical Eponyms
Syndrôme de Huchard (1893)
The Texidor Twinge or Precordial Catch Syndrome (PCS) is a benign condition that causes brief episodes of localised musculoskeletal chest pain in children and young adults. Pain is pleuritic, non-exertional, and typically sudden onset at rest or with minimal activity. Forced inspiration or correction of posture often relieves pain completely. The exact aetiology is unknown.
1892 – Huchard first described the condition which he termed ‘précordialgie’ (from the latin “praecordia” meaning “before the heart”). The condition was later termed ‘Syndrôme de Huchard’ or ‘Huchard syndrome’.
Dans une leçon clinique qu’il faisait à l’hopital Bichat au mois de novembre 1892, M. Huchard donnait le nom de précordialgie à toute douleur, accompagnée ou non d’angoisse, survenant dans la région précordiale. Après avoir passé en revue les diverses douleurs qui peuvent affecter cette région, notre excellent maître arrivait à cette conclusion: «En général, à de rares exceptions près, chaque fois qu’un malade vient se plaindre au médecin, d’une douleur dans la région cardiaque, il n’a pas d’affection organique du cœur»
In a clinical lesson he gave at the Bichat hospital in November 1892, Mr. Huchard gave the name precordialgia to any pain, whether or not accompanied by anxiety, occurring in the precordial region. After having reviewed the various pains which can affect this region, our excellent teacher came to this conclusion: “In general, with rare exceptions, each time a patient comes to complain to the doctor, of a pain in the region of the heart, there is no organic cause“
Huchard classified the précordialgies into 4 categories
1° Douleurs précordiales, accompagnées d’angoisse douleurs de l’angine et des pseudu-angines de poitrine;
2° Précordialgies ne consistant que dans l’angoisse qui s’ observent dans les maladies infectieuses et qui ne s’ accompagnent pas de douleur. J’ai en maintes fois l’occasion de les rencontrer dans les formes malignes de la variole, de la grippe, de la scarlatine, etc;
3° Précordialgies néuralgiques, caractérisées par des douleurs augmentant par la pression sans angoisse;
4° Enfin, on peut encore établir un quatrième groupe en mentionnant les «algies centrales» que j’ai étudiées dans un travail récent (1) et que Blocq appelle «topoalgies». Ces douleurs ont pour caracteres de ne pas exister sur le trajet d’un nerf, de ne pas augmenter à la pression, et chez certains malades, elles se localisent à la région précordiale. Une telle douleur a un siège central et non périphérique; elle est comparable à ces douleurs que les amputés croieut éprouver dans le membre qu’on leur a enlevé.
Huchard Les précordialgies 1893
(1) Huchard. Les Neurasthénies Locales. 1892
1° Precordial pains of angina and pseudo-angina pectoris, accompanied by anxiety
2° Precordialgias consisting only of anxiety. Observed in infectious diseases and not accompanied by pain. I have on many occasions the opportunity to meet them in the malignant forms of smallpox, influenza, scarlet fever, etc;
3° Neuralgic precordialgia, characterized by pain increased with pressure without anxiety;
4° Finally, we can establish a fourth group by mentioning the “central pain” that I studied in a recent work (Huchard. Les Neurasthénies Locales. 1892) and that Blocq calls “topoalgia”. These pains have the characteristics of not existing on the path of a nerve, of not increasing under pressure, and in some patients, they are localized in the precordial region. Such pain has a central and not a peripheral site; it is comparable to the pains that amputees believe to experience in the limb that has been removed.
Huchard Les précordialgies 1893
Huchard’s disease (essential hypertension)
Historic term applied to primary/essential hypertension in Huchard’s framework of “cardio-arterial” disease (arterial sclerosis + raised tension driving cardiac change).
Huchard emphasised clinical measurement and interpretation of arterial tension and therapeutic regimens (rest, diet, graded activity, digitalis/caffeine/theobromine, nitroglycerin).
Huchard’s sign
In hypertension, failure of the pulse/heart rate to diminish appropriately when changing from standing to supine position. Reported as a bedside clue to elevated arterial tension. The observed reduction in heart rate is less than that for normotensive patients.
Period usage varied. Rarely used today though retained historically in French compilations
Médaille de Henri Huchard (1903)

Troisième République Médaille de Henri Huchard is a commemorative bronze medal struck in 1903 to honour Huchard at the Hôpital Necker (Paris). Designed and signed by the renowned French sculptor–medallist Alfred Boucher (1850–1934).
The medal commemorates Huchard 25 years of service at Hôpital Necker. Such medals were a common civic form of honouring scientific/medical achievement
The Troisième République (1870–1940) were founded after Napoleon III’s defeat at Sedan and collapse of the Second Empire. A parliamentary republic with public celebration of doctors, teachers, and scientists
Major Publications
- Desnos L, Huchard H. Des complications cardiaques dans la variole et notamment de la myocardite varioleuse. 1871
- Axenfeld A, Huchard H. Traité des névroses. 2e 1883
- Huchard H. Quand et comment doit-on prescrire la digitale. 1888
- Huchard H. Maladies du coeur et des vaisseaux: artério-sclérose, aortites, cardiopathies artérielles, angines de poitrine. 1889 [2e 1893]
- Huchard H. La thérapeutique pathogénique. 1891
- Huchard H. Le rythme couplé du coeur et la mort par la digitale. Revue générale de clinique et de thérapeutique 1892
- Huchard H. Les Neurasthénies Locales. Archives générales de médecine 1892; ser 7(30): 641-650 [Syndrôme de Huchard
- Huchard H. Les précordialgies. Revue générale de clinique et de thérapeutique 1893; 7: 1-2 [Syndrôme de Huchard]
- Huchard H. Traité clinique des maladies du coeur et des vaisseaux. 1893
- Huchard H. Traité clinique des maladies du coeur et de l’aorte. 1899 et Tome II [evaluation of the 80 theories of angina pectoris development pp 77-80]
- Huchard H. Consultations médicales clinique et thérapeutique. 1901
- Huchard H. Clinique thérapeutique du praticien. 1908
- Huchard H. Les maladies du coeur et leur traitement. 1908
- Huchard H. Maladies du coeur: artériosclérose. 1910
- Huchard H. La thérapeutique en vingt médicaments. 1910
- Huchard H. Maladies de l’appareil. 1911
References
Biography
- Le Docteur Huchard. Chanteclair 1908; 3(2): 3
- Henri Huchard. La Presse médicale 1910; 18: 1009-1011
- Brohin A. Henri Huchard. Gazette des hôpitaux civils et militaires 1910; 83: 1946
- Dr. Henri Huchard. Br Med J. 1910; 2(2608): 2011
- Nécrologie: Henri Huchard. Paris médical : la semaine du clinicien 1911; II(XIII)
- Piatot A. Les plaquettes médicales: Henri Huchard. Paris médical : la semaine du clinicien
- Henri Huchard (1844-1910) – Data BNF
- Bibliography. Huchard, Henri. WorldCat Identities
Eponymous terms
- Chevillot P. Les précordialgies: étude séméiologique sur les douleurs de la région du coeur. 1893
- Prinzmetal M, Massumi RA. The anterior chest wall syndrome: chest pain resembling pain of cardiac origin. J Am Med Assoc. 1955; 159(3): 177-184.
- Wehrmacher WH. The painful anterior chest wall syndromes. Med Clin North Am. 1958; 42(1): 111-118
- Leibowitz JO. The History of Coronary Heart Disease. 1970: 144-145
Eponym
the person behind the name
MB BCh BAO, Queen’s Belfast. Recently moved to Australia, interested in Emergency Medicine, Medical Education and Paediatrics. Keen baker & tea drinker!
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | On Call: Principles and Protocol 4e| Eponyms | Books |

