Jean-Athanase Sicard

Jean-Athanase Sicard (1872-1929) was a French physician
Sicard trained in the Paris hospitals and became a leading clinician-teacher at Hôpital Necker and later at the Paris Faculty. His career bridged neurology, pain therapy, and early neuroradiology, and he maintained a reputation for practical bedside neurology and an unusually wide technical repertoire for the era.
Sicard’s influence is felt most strongly in procedures that sit at the junction of needle, nerve and diagnosis. In 1901 he was one of the two Paris pioneers (with Fernand Cathelin) to develop the sacral route to the epidural space. This work that helped launch caudal epidural injection as both an anaesthetic and therapeutic technique. In parallel, he contributed to the early clinical science of neurology through CSF studies, reflecting the turn-of-the-century shift toward laboratory-supported diagnosis.
In the 1920s Sicard’s collaborations became foundational for spinal imaging. With Jacques Forestier (1890–1978) he introduced Lipiodol as a radiopaque agent for epidural exploration and helped drive the rapid evolution toward contrast myelography, transforming the localisation of compressive spinal lesions. Alongside this procedural legacy, Sicard’s name persists in classic skull-base localisation in Collet–Sicard syndrome and injection therapy in France, including his later work on sclerosing injections for varicose veins with Louis C. Gaugier.
Biographical Timeline
- Born June 23, 1872 in Marseille, France.
- 1890s – Medical studies begun in Marseille, completed in Paris; influenced in neurology by Édouard Brissaud (1852–1909). Research with Georges-Fernand Widal (1862–1929).
- 1894 – Externe des hôpitaux (Paris).
- 1895 – Interne des hôpitaux (Paris).
- 1899 – MD (Paris); doctoral work and early studies on cerebrospinal fluid.
- 1901 – Chef de clinique; reported cytological CSF changes in chronic neurosyphilis. Independently of Fernand Cathelin (1873–1960), Sicard pioneers caudal (sacral) epidural injection via puncture of the sacral canal (“Sicard’s method”).
- 1903 – Médecin des hôpitaux (Paris).
- 1906 – Appointed agrégé (Faculty of Medicine, Paris).
- 1910 – Appointed chef de service, Hôpital Necker, Paris.
- 1914–1918 – World War I service: mobilised Aug 2, 1914; served in the Sanitary Corps (initially Toulon), later led the Neurological Centre of the XVth military region in Marseille.
- 1921 – With Jacques Forestier (1890–1978) advanced radiographic exploration using iodised oil (Lipiodol). Noted prior use of air for “epidural pneumo” and promoted Lipiodol epidurography for detecting compressive lesions.
- 1923 – Appointed Professor of (Internal) Pathology / Medical Pathology, Paris Faculty; continued leadership/teaching at Necker.
- Died January 28, 1929 in Paris (aged 57).
Medical Eponyms
Sicard’s method (1901)
An epidural injection technique in which medication is introduced into the epidural space via the sacral canal (through the sacro-coccygeal region/sacral hiatus), i.e. “dans le canal sacré, en dehors des méninges.”
1901 – Experimental caudal epidural injections (including cocaine) were explored in parallel by Fernand Cathelin (1873–1960) and Sicard. Cathelin explicitly stated that “priority is set aside” and that “M. Sicard and I experimented simultaneously and independently, describing sacral canal injections producing profound analgesia/anaesthesia in animals (Jan–Feb 1901).
Cathelin (1901) reported complete analgesia after “injections de cocaïne dans l’espace épidural par la voie du canal sacré” and noted the independent parallel work with Sicard.
c.1920–1923 – Sicard’s “injection” work broadened into radiological exploration using iodised oil (Lipiodol), initially observed tracking through tissue planes, then adapted to epidural injection for sciatica and ultimately to intrathecal use, catalysing modern spinal contrast studies.
Modern usage: Caudal epidural injection remains a standard route for epidural therapy (analgesia and steroid/local anaesthetic delivery). Sicard’s later Lipiodol work sits historically at the junction between therapeutic epidural injection and diagnostic neuroradiology (epidurography → myelography).
Collet–Sicard syndrome (1915; Sicard expanded 1917)
Unilateral palsy of the lower cranial nerves IX, X, XI and XII, usually localising to a skull-base lesion involving the jugular foramen (IX–XI) with extension to the hypoglossal canal (XII).
- IX / X: dysphagia, palatal droop, impaired gag; dysphonia/hoarseness (vocal cord palsy)
- XI: sternomastoid/trapezius weakness → shoulder droop, impaired head turn
- XII: tongue weakness/wasting with deviation toward the lesion
1915 – Frédéric Justin Collet (1870–1964) described a new war-injury pharyngo-laryngeal paralytic syndrome in a soldier with a bullet wound to the skull base. Injury caused unilateral glosso–laryngo–scapulo–pharyngeal paralysis of cranial nerves IX–X–XI–XII which Collet described as “hémiplégie glosso-laryngo-scapulo-pharyngée”
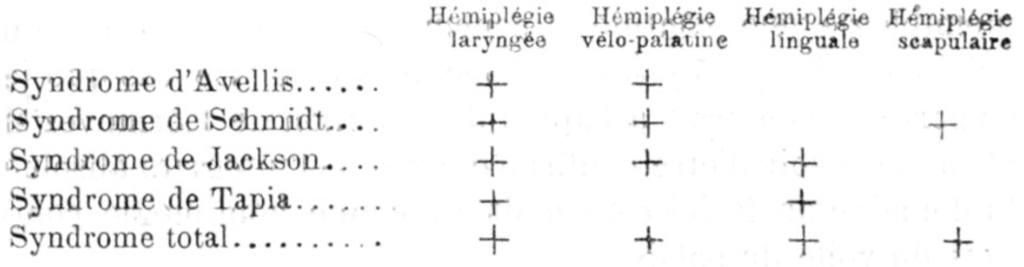
1917 – Sicard reported a comparable (and more anatomically localised) entity as a “pure type” paralysis of the last four cranial nerves, naming the skull-base crossroads the “carrefour condylo-déchiré postérieur” (posterior condylar–lacerum region), again rooted in trauma.
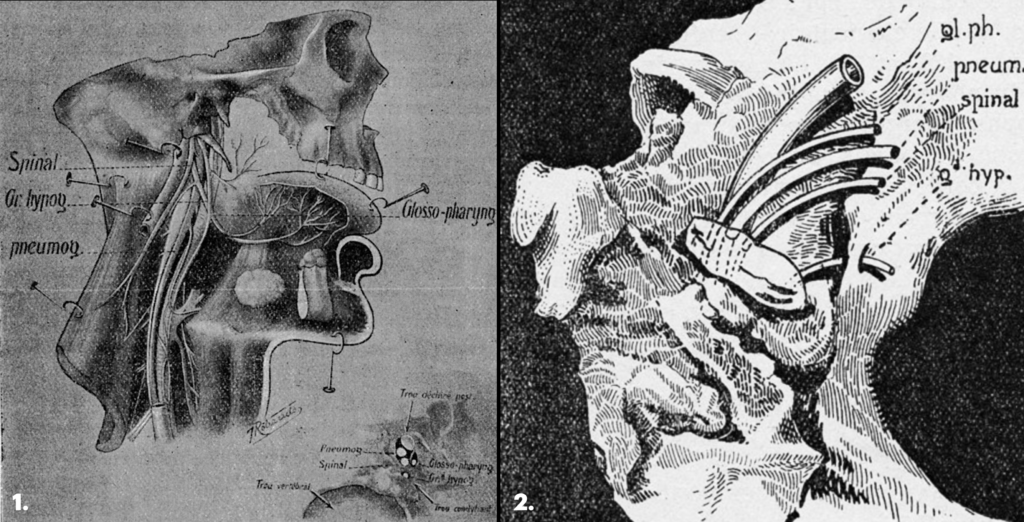
Figure 2. Sicard’s wartime skull-base illustration showing a retained projectile in the posterior condylar region and the adjacent lower cranial nerve pathways—anatomical justification for combined IX–X–XI–XII palsy following penetrating trauma.
Modern interpretation: Originally a war-trauma skull-base localisation syndrome, Collet–Sicard syndrome is now used for IX–X–XI–XII palsy from any pathology at the jugular foramen/hypoglossal canal region. Most commonly associated with skull-base tumours/metastases, basilar skull fractures/occipital condyle injuries, vascular lesions (e.g. carotid dissection), inflammatory/infective and iatrogenic causes.
Brissaud–Sicard syndrome (1908)
A crossed pontine syndrome characterised by ipsilateral facial spasm (hemifacial spasm/cramps) with contralateral hemiparesis, due to a lesion involving the pons (classically the basilar/anterolateral pons affecting corticospinal pathways with irritation of facial nerve fibres/nucleus).
Clinical features
- Ipsilateral tonic/clonic facial contractions (hemifacial spasm)
- Contralateral pyramidal weakness (hemiparesis) ± other long-tract signs
- Localises to the pons
1856 – Adolphe-Marie Gubler (1821–1879) described the crossed pontine pattern (often cited as the earliest description).
1908 – Édouard Brissaud (1852–1909) and Sicard published a detailed clinical series (three cases), attributing the syndrome to pontine pyramidal tract involvement with facial nerve irritation (reported in the context of syphilis-related cerebrovascular disease).
NOTE: Not to be confused with Millard–Gubler syndrome:
- Brissaud–Sicard describes ipsilateral hemifacial spasm with contralateral hemiparesis, implying irritation of facial pathways plus corticospinal involvement in the pons.
- Millard–Gubler is the “loss” syndrome, facial palsy rather than spasm, paired with contralateral hemiplegia.
Sicard’s method II (1921)
Radiographic exploration of the epidural space (“cavité épidurale”) using Lipiodol (iodised poppy-seed oil) injected extra-durally to outline epidural spread and help localise compressive spinal pathology.
1920 – While treating sciatica with iodised oil preparations, Sicard observed Lipiodol’s radiopacity and gravity-dependent tracking along tissue planes, then refined a deliberate epidural injection technique for analgesia and for mapping spread.
1921 – Sicard and Jacques Forestier (1890-1978) published “Méthode radiographique d’exploration de la cavité épidurale par la lipiodol”, noting they had long used air in “epidural pneumo,” and proposing Lipiodol epidurography to detect compressive lesions.
After 1921 – The work rapidly bridged into intrathecal Lipiodol myelography (often described as arising after inadvertent subarachnoid injection), formalised with later publications (e.g. suboccipital/cervical approaches in 1923 with Paraf and Laplane).
Modern relevance: “Sicard’s method II” sits at the hinge between therapeutic epidural injection and diagnostic neuroradiology. Lipiodol techniques transformed localisation of spinal compressive lesions and dominated practice for decades before being replaced by newer contrast media and, later, MRI.
Note: The 1921 method is explicitly epidural cavity exploration. Intrathecal Lipiodol myelography developed soon after and was consolidated in subsequent publications.
Major Publications
- Sicard J-A. Les Injections sous-arachnoïdiennes et le liquide céphalo-rachidien, recherches expérimentales et cliniques 1900
- Enriquez E, Sicard J-A. Les oxydations de l’organisme. 1902
- Sicard J-A. Exposé des travaux scientifiques. 1903 [1906, 1925]
- Brissaud E, Sicard J-A. L’hémispasme facial alterné. Presse médicale (Paris), 1908; 16: 234-236
- Sicard J-A. Syndrome du carrefour condylo-déchiré postérieur (type pur de paralysie des quatre derniers nerfs craniens). Marseille médical. 1917; 53: 385-397
- Sicard J-A, Forestier J. Méthode radiographique d’exploration de la cavité épidurale par la lipiodol. Revue neurologique, Paris, 1921, 28(12): 1264-1266
- Sicard J-A, Forestier J. Méthode générale d’exploration radiologique par l’huile iodée (lipiodol). Bulletins et Mémoires de la Société médicale des hôpitaux de Paris 1922; 46(1): 463-469
- Sicard J-A, Paraf J, Lermoyez J. Traitement des varices par les injections phlébo-sclérosantes du salicylate de soude. Gazette des hôpitaux, Paris, 1922, 95: 1573-1575.
- Sicard J-A, Forestier J. Diagnostic et thérapeutique par le lipiodol; clinique et radiologie. 1928 [English translation: 1932]
- Sicard J-A, Gaugier L. Le traitement des varices par les injections locales sclérosantes. 2e 1929
References
Biography
- Roger H. J-A. Sicard (1872-1929). La Presse médicale 1929; 38: 153–154
- Steimle RH. Jean A. Sicard (1872-1929). His pioneer work in nervous diseases. Neuroradiology. 1990;32(1):1-3.
Eponymous terms
Collet-Sicard syndrome
- Collet FJ. Sur un nouveau syndrome paralytique pharyngo-laryngé par blessure de guerre (hémiplégie glosso-laryngo-scapulo-pharyngée) Lyon médical, 1915; 124: 121-129
- Gutiérrez Ríos R et al. Collet-Sicard syndrome. Neurologia. 2015 Mar;30(2):130-2.
- Mnari W et al. An unusual etiology of posttraumatic Collet-Sicard Syndrome: a case report. Pan Afr Med J. 2016 Mar 30;23:143
- Aguilera-Pena MP et al. Collet-Sicard syndrome: a scoping review. Neurosurg Rev. 2023 Sep 14;46(1):244
- Tekiner H, Yale ES, Draves J, Yale SH. Trauma eponyms (1837-1950): a comprehensive historical review. J Trauma Inj. 2025 Sep;38(3):168-180.
Brissaud-Sicard syndrome
- Gubler A-M. De l’hémiplégie alterne envisagée comme signe de lésion de la protubérance annulaire et comme preuve de la décussation des nerfs faciaux. Gazette hebdomadaire de médecine et de chirurgie. 1856; 3: 749-754, 789-792, 811-816.
- Tacik P, Krasnianski M, Alfieri A, Dressler D. Brissaud-Sicard syndrome caused by a diffuse brainstem glioma. A rare differential diagnosis of hemifacial spasm. Acta Neurochir (Wien). 2014 Feb;156(2):429-30.
Eponym
the person behind the name
BSc MD University of Western Australia. Interested in all things critical care and completing side quests along the way
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | On Call: Principles and Protocol 4e| Eponyms | Books |

