Jerome W. Conn

Jerome W. Conn (1907-1994) was an American endocrinologist
Conn’s name is synonymous with primary hyperaldosteronism, or Conn syndrome. He trained and spent his entire career at the University of Michigan, where he led the Division of Endocrinology and Metabolism and became one of the most influential figures in 20th-century endocrine medicine.
In 1955 he presented the case of a young woman with hypertension and hypokalaemia caused by an aldosterone-producing adrenal adenoma. Drawing on earlier wartime research into heat acclimatisation and sodium metabolism, Conn postulated that excess aldosterone could cause autonomous sodium retention. This led to the identification of a curable form of endocrine hypertension and a lasting shift in clinical approach.
Beyond the initial syndrome, Conn developed diagnostic frameworks involving plasma renin activity (1961), classified types of aldosteronism (1964), and described licorice-induced pseudoaldosteronism (1968). He remained a central figure in academic medicine for decades, known for both his clinical insight and pioneering role in adrenal pathophysiology.
Biographical Timeline
- Born September 24, 1907 in New York City
- 1924–1927 – Attended Rutgers University
- 1928-1932 – University of Michigan Medical School. Graduated MD with honours; inducted into Alpha Omega Alpha
- 1932 – Internship in surgery, later transitioned to internal medicine
- 1935 – Appointed clinical fellow at the University of Michigan
- 1938 – Became Assistant Professor
- 1943 – Appointed Director of the Division of Endocrinology and Metabolism
- 1940s (WWII) – Researched heat acclimatisation in military personnel; discovered sodium retention mechanisms involving adrenal hormones
- 1954 – Admitted a patient with episodic muscle weakness and hypokalaemia; postulated hyperaldosteronism due to an adrenal adenoma
- 1955 – First described primary hyperaldosteronism, later termed Conn syndrome, caused by aldosterone-secreting adrenal adenomas
- 1965 – Awarded the Gairdner Foundation International Award for his work on endocrine hypertension
- 1968 – Named L. H. Newburgh Distinguished University Professor at the University of Michigan
- 1974 – Retired from the University of Michigan after a 40+ year academic career
- Died June 11, 1994 in Naples, Florida, aged 86
Medical Eponyms
Conn Syndrome (Primary Hyperaldosteronism) 1955
Primary hyperaldosteronism, or Conn syndrome, is characterised by the autonomous secretion of aldosterone, leading to hypertension, hypokalaemia, and metabolic alkalosis and suppressed plasma renin activity. The condition is potentially curable and revolutionised the understanding of endocrine causes of hypertension.
1940s – Precursor Research. During World War II, Conn studied the physiology of heat exposure and salt conservation in soldiers stationed in hot, humid climates. His work on heat acclimatisation revealed that sodium conservation was regulated by the adrenal cortex and led him to hypothesise the existence of distinct “salt-active” adrenal steroids well before aldosterone was identified by Simpson et al in 1952
1954 – The Index Case. In April 1954, a 34-year-old woman was admitted to the University of Michigan with paralysis, tetany, severe hypokalaemia, and hypertension. Conn immediately suspected adrenal overproduction of a salt-retaining steroid, noting the absence of cortisol or androgen excess. Over 227 days, she underwent exhaustive testing in the metabolic unit, including:
- Electrolyte analysis of sweat and saliva
- Bioassays in adrenalectomised rats showing 4–30× normal levels of mineralocorticoid
- Metabolic balance studies confirming resistance to potassium repletion
These findings paralleled Conn’s wartime heat acclimatisation work, pointing to mineralocorticoid excess, likely aldosterone.
1955 – Conn presented his findings on June 11, 1955, at the Central Society for Clinical Research in Chicago, outlining a new syndrome with episodic paralysis, hypokalaemia, and hypertension caused by an aldosterone-producing adrenal adenoma. His patient underwent successful surgical removal of a 13 g adrenal tumour, with resolution of hypertension and hypokalaemia. Conn also proposed a screening test using sodium loading to evaluate aldosterone autonomy.
Key Medical Contributions
Renin–Aldosterone Axis and the Diagnosis of Primary Aldosteronism
Following his 1955 description of primary hyperaldosteronism, Conn recognised the importance of plasma renin activity (PRA) in distinguishing between primary and secondary forms. He helped establish the foundational principle that suppressed renin in the context of elevated aldosterone indicates an autonomous adrenal source.
Low plasma renin activity in the presence of mineralocorticoid excess distinguishes primary aldosteronism and provides a critical diagnostic tool.
Conn, JAMA 1964
This concept evolved into the modern aldosterone-renin ratio (ARR), which remains the screening cornerstone for primary aldosteronism.
Classifying Aldosteronism
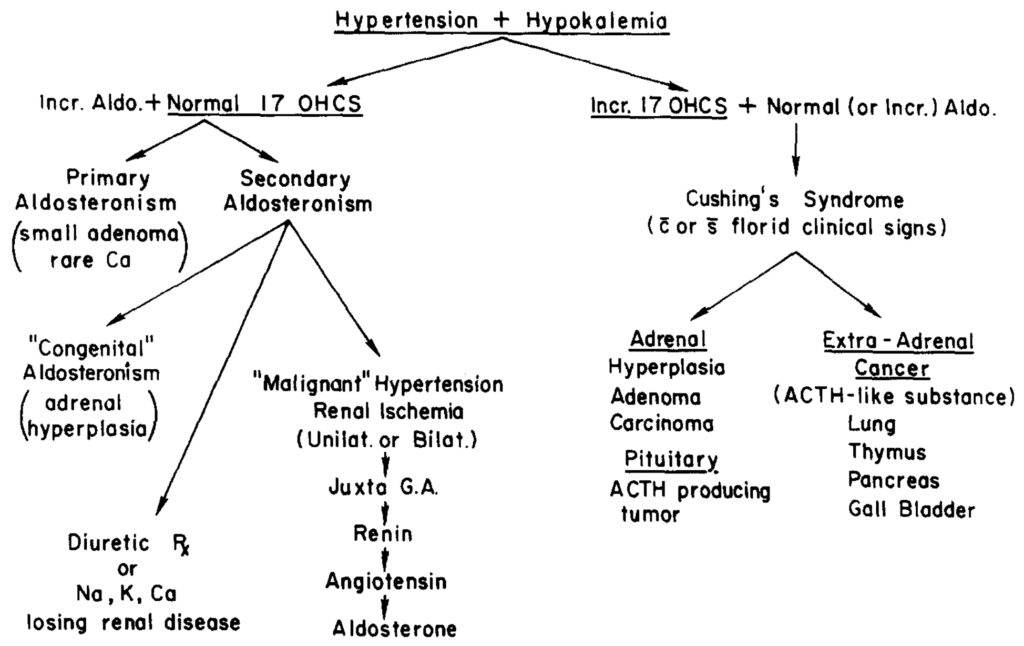
In a pivotal 1964 American Journal of Surgery publication, Conn and colleagues reviewed 145 cases of primary aldosteronism, refining the clinical understanding of the syndrome. This work defined the clinical spectrum, expanded awareness of normokalaemic variants, and proposed a diagnostic flowchart that became a foundational model for endocrine hypertension.
Primary aldosteronism is not rare. Its recognition depends on clinical vigilance, especially in patients with resistant hypertension and spontaneous hypokalaemia.
Conn, Am J Surg 1964
Figure 2 from this paper proposed a pathophysiological classification separating:
- Primary aldosteronism (e.g., adenoma, hyperplasia)
- Secondary aldosteronism (e.g., renin-driven)
- Pseudohyperaldosteronism (e.g., licorice ingestion, Liddle syndrome)
1968 – Conn published a groundbreaking case of licorice-induced pseudoaldosteronism, in which a patient developed hypertension, hypokalaemia, and suppressed renin and aldosterone from chronic ingestion of glycyrrhizinic acid, the active component of licorice. This case mimicked primary aldosteronism but with a key difference: aldosterone levels were low. The condition was experimentally reproduced and reversed with cessation of licorice intake, illustrating the power of the renin-aldosterone axis as a diagnostic discriminator.
When both renin and aldosterone yield low values it is likely that a potent sodium-retaining substance, other than aldosterone… is at work.
Conn, 1968
Major Publications
- Conn JW, Newburgh LH. The glycemic response to isoglucogenic quantities of protein and carbohydrate. J Clin Invest. 1936 Nov;15(6):665-71.
- Conn JW. The advantage of a high protein diet in the treatment of spontaneous hypoglycemia: Preliminary Report. J Clin Invest. 1936 Nov;15(6):673-8.
- Conn JW, Newburgh LH, Johnson MW, Conn ES. A new interpretation of diabetes mellitus in obese, middle-aged persons: Recovery through reduction in weight. Transactions of the Association of American Physicians. 1938, 53: 245-257.
- Conn JW. Man’s endocrine and metabolic responses to stressing circumstances: clinical implications. Hawaii Med J. 1954 Sep-Oct;14(1):19-26.
- Conn JW. Presidential address Part I: Painting background. The Journal of Laboratory and Clinical Medicine 1955; 45(1): 3-17.
- Conn JW. Presidential address Part II: Primary aldosteronism. The Journal of Laboratory and Clinical Medicine 1955; 45(4): 661-664 [Conn Syndrome]
- Conn JW, Louis LH. Primary aldosteronism: a new clinical entity. Transactions of the Association of American Physicians. 1955; 68: 215-31; discussion, 231-3.
- Conn JW, et al. Intermittent aldosteronism in periodic paralysis; dependence of attacks on retention of sodium, and failure to induce attacks by restriction of dietary sodium. Lancet. 1957 Apr 20;272(6973):802-5.
- Conn JW, Conn ES. Primary aldosteronism versus hypertensive disease with secondary aldosteronism. Recent Prog Horm Res. 1961;17:389-414
- Conn JW. Plasma renin activity in primary aldosteronism. importance in differential diagnosis and in research of essential hypertension. JAMA. 1964 Oct 19;190:222-5.
- Conn JW, Knopf RF, Nesbit RM. Clinical characteristics of primary aldosteronism from an analysis of 145 cases. Am J Surg. 1964 Jan;107:159-72.
- Fajans SS, Floyd JC Jr, Knopf RF, Conn FW. Effect of amino acids and proteins on insulin secretion in man. Recent Prog Horm Res. 1967;23:617-62
- Conn JW, Rovner DR, Cohen EL. Licorice-induced pseudoaldosteronism. Hypertension, hypokalemia, aldosteronopenia, and suppressed plasma renin activity. JAMA. 1968 Aug 12;205(7):492-6.
- Conn JW, Cohen EL, Lucas CP, McDonald WJ, Mayor GH, Blough WM Jr, Eveland WC, Bookstein JJ, Lapides J. Primary reninism. Hypertension, hyperreninemia, and secondary aldosteronism due to renin-producing juxtaglomerular cell tumors. Arch Intern Med. 1972 Nov;130(5):682-96.
References
Biography
- Jerome W. Conn. Biographical Memoirs. National Academies of Sciences, Engineering, and Medicine 1997; 71
- Beazley RM. An evening with Dr. Jerome W. Conn. Endocr Pract. 2010 Sep-Oct;16(5):919-20.
Eponymous terms
- Simpson SA, Tait JF, Bush IE. Secretion of a salt-retaining hormone by the mammalian adrenal cortex. Lancet. 1952 Aug 2;2(6727):226-8.
- Gittler RD, Fajans SS. Primary aldosteronism (Conn’s syndrome). J Clin Endocrinol Metab. 1995 Dec;80(12):3438-41.
- Young WF. Primary aldosteronism: renaissance of a syndrome. Clin Endocrinol (Oxf). 2007 May;66(5):607-18.
- Parmar MS, Singh S. Conn Syndrome. 2022 Sep 12. In: StatPearls [Internet].
Eponym
the person behind the name
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | On Call: Principles and Protocol 4e| Eponyms | Books |
