Hans Kehr

Johannes Otto Kehr (1862-1916) was a German surgeon.
Hans Keh was a transformative figure in the evolution of biliary surgery. At a time when gallbladder disease was often managed conservatively or with limited operative techniques like cholecystostomy, Kehr championed the routine use of cholecystectomy. Through thousands of meticulously documented operations, he advanced a structured surgical approach to gallstone disease that emphasised early diagnosis, thorough ductal exploration, and definitive treatment. His seminal text, Die Praxis der Gallenwege-Chirurgie in Wort und Bild (1913), consolidated his operative philosophy and provided richly illustrated case studies that educated a generation of surgeons across Europe and beyond.
In clinical circles, his name also became associated with Kehr’s sign, left shoulder pain due to diaphragmatic irritation from splenic pathology, although this was a posthumous eponym rooted in a tangential observation from his writings on splenic pathology.
Kehr developed the T-tube for biliary drainage, now widely known as the Kehr tube. First described in 1912, this simple yet elegant device allowed safe postoperative drainage of the common bile duct following choledochotomy, preventing bile leakage and enabling cholangiographic evaluation. His modifications, including shortening the transverse limb and partial wall excision, reflected a deep understanding of intraoperative anatomy and long-term patient outcomes. Kehr also emphasized the importance of intraoperative inspection and palpation of the bile ducts.
Biographical Timeline
- Born April 27, 1862 in Waltershausen, Thuringia, Germany, as the third eldest son of Karl Kehr, a respected educator.
- 1880s – Attended multiple medical schools: Freiburg, Jena, Halle, and Berlin.
- 1885 – Earned his medical degree in 1885 from the University of Jena.
- 1885–1888 – Completed a two-year assistantship in Gotha with Meusel, followed by opening a private surgical clinic in Halberstadt.
- 1890 – Performed his first cholecystectomy in Halberstadt, reportedly never having seen one performed before.
- 1895 – Received the title of Professor for his innovative work in gallstone disease surgery.
- 1899 – Published “Anleitung zur Erlernung der Diagnostik der einzelnen Formen der Gallensteinkrankheit”, based on 433 gallstone laparotomies.
- 1903 – Lectured and demonstrated biliary surgery techniques in the United States, expanding his international reputation.
- 1904 – Invited to Paris to consult on the case of the French Prime Minister, Pierre Waldeck-Rousseau.
- 1905 – Awarded the title Geheimer Sanitätsrat (Privy Medical Councillor).
- 1907 – Operated on the daughter of Professor Ernst von Bergmann in Halberstadt in a high-profile procedure witnessed by several professors from Berlin.
- 1910 – Moved to Berlin, opened a new private clinic and dedicated himself to publishing and specializing in biliary tract surgery.
- 1913 – Published his monumental work “Die Praxis der Gallenwege-Chirurgie in Wort und Bild”
- Died May 20, 1916 of septicaemia in Berlin after contracting an infection from a surgical wound
Medical Eponyms
Kehr’s Sign
Kehr’s sign is classically described as the occurrence of left shoulder (referred) pain stemming from irritation of the diaphragmatic peritoneum, most often due to a sub‑diaphragmatic process such as splenic rupture, splenic infarct, or abscess on the left side.
Clinically it is used as a clue in trauma and surgical settings: the presence of left radiating shoulder pain (via the phrenic nerve, C3–C5) in the setting of blunt abdominal injury may prompt consideration of splenic injury even when the abdomen appears relatively unremarkable otherwise.
From the surgical and radiological perspective, the sign remains of limited sensitivity but high specificity in appropriate context: i.e., left shoulder pain + left upper quadrant trauma + unstable haemodynamics. Its value lies in prompting further imaging or exploration rather than serving as definitive evidence. While modern trauma protocols rely heavily on FAST ultrasound, CT scan, and full diagnostics, the historical sign still appears in textbooks as an eponymous “warning sign”.
1907 – The attribution of this phenomenon to Hans Kehr stems from his prominence in German biliary and abdominal surgery in the early 20th century and his description of “Schulterschmerz” (shoulder pain) in the context of splenic pathology.
Symptomatologie und Verlauf. Ein pathognostisches Symptom für die Verletzungen der Milz gibt es nicht, bei den Kontusionen sind Schmerz und Vergrößerung der Milz die gewöhnlichen Erscheinungen, bei den Rupturen drängen die Zeichen der inneren Blutung alle anderen Symptome in den Hintergrund. Der Betroffene wird bei der subkutanen Verletzung meistenteils von einem anfangs in der linken Seite, schnell sich über das ganze Abdomen verbreitenden Schmerz befallen. Die Zeichen des Kollapses (ausgesprochene Blässe, kleiner Puls, Kälte- und Ohnmachtsgefühl) stellen sich ein: in sehr seltenen Fällen fühlt der Verletzte gar nichts von der Milzzerreißung und der Kollaps kann ausbleiben. Der linksseitige Schulterschmerz ist nicht häufig; sonstige Erscheinungen von Seiten der Lunge, des Herzens und des Kehlkopfes (heisere Stimme bis zur völligen Stimmlosigkeit) deuten auf eine Alteration des Vagus, der mit dem Plexus lienalis durch das Ganglion semilunare in Beziehung steht, hin. Der Bluterguß nimmt entweder die ganze Bauchhöhle ein oder beschränkt sich nur auf gewisse Teile des Abdomens, wenn vor dem Unfall in der Umgebung der krankhaft veränderten Milz Verwachsungen bestanden, welche die allgemeine Ausbreitung der Blutung in der Bauchhöhle verhindern. Betraf die Ruptur eine krankhaft vergrößert/C Milz, so kann bei Zerreißung der Milzkapsel der Milztumor kleiner werden, während bei einer Blutung in das Milzgewebe ohne gleichzeitige Verletzung der Milzkapsel sich ein palpabler Milztumor entwickeln kann – Kehr 1907
There is no pathognomonic symptom for injuries to the spleen. In contusions, pain and enlargement of the spleen are typical symptoms; in ruptures, all the other signs and symptoms of internal bleeding are less important …The signs of collapse (pronounced pallor, small pulse, cold and feeling of fainting) appear. In very rare cases, the injured person feels nothing at all of the rupture of the spleen and the collapse may not occur. Left-sided shoulder pain is not common. Other symptoms from the lungs, heart and larynx (hoarse voice to complete voicelessness) indicate an alteration of the vagus, which is connected to the splenic plexus through the semilunar ganglion. Kehr 1907
Kehr never claimed left shoulder pain was either pathognomonic or frequent, but that it was observed occasionally in the context of splenic pathology.
1910 – Wiesbaden surgeon, Lorenz Levy published Zur Diagnose der Milzverletzungen. He referenced Kehr’s publication on splenic injuries and left shoulder pain symptoms when presenting the case of a 29-year old man with internal haemorrhage secondary to splenic injury and severe left shoulder pain, emphasising its diagnostic significance.
Ich habe mich bemüht, in der mir zugängigen Literatur Angaben über die Diagnose der subkutanen Ruptur zu finden und habe dabei ein Symptom vermißt, das mir in einem Falle sehr bemerkenswert erschien. Eine diesbezügliche Angabe fand ich nur in dem von Kehr im Handbuch der Chirurgie von Bergmann, Mikulicz und Bruns bearbeiteten Kapitel über die Milz… In meinem Falle klagte der Kranke außer über die Bauchschmerzen über heftigste Schmerzen in der linken Schulter. Ich erinnere nur an die als pathognomonisch geltenden Schmerzen in der rechten Schulter beim Leberabszeẞ. Wie bei der Leber , so dürften die Schulterschmerzen bei Verletzungen der Milz auf eine Alteration des Nervus phrenicus zurückzuführen sein, der seinerseits wieder mit dem vierten Cervikalnerven in Verbindung steht und so die Schmerzen hervorruft – Levy 1910
I tried to find information about the diagnosis of subcutaneous rupture in the literature available to me and I missed a symptom that in one case seemed very remarkable. I only found information in the chapter on the spleen by Kehr in the Handbook of Surgery by Bergmann, Mikulicz and Bruns…
In my case, in addition to the abdominal pain, the patient complained of severe pain in the left shoulder. I remember that pain in the right shoulder that is considered pathognomonic in liver abscess. Left shoulder pain caused by injuries to the spleen is likely to be due to an alteration of the phrenic nerve, which in turn is connected to the fourth cervical nerve and thus causes the pain – Levy 1910
Levy explicitly cited Kehr’s 1907 treatise and emphasized that while often overlooked, the presence of left shoulder pain could offer significant diagnostic value in ambiguous abdominal trauma.
1938 – The concept was further refined by Max Saegesser (1902-1975), who described a phrenic nerve pressure point sign. This was a clinical method of physically eliciting referred pain to aid diagnosis:
The examination is performed by applying pressure with the thumb of the right hand from behind on the left side of the neck between the sternocleidomastoid and anterior scalene muscles and in the direction of the larynx and spine. If tenderness is clearly more marked on the left. Combined with local findings this can strongly suggest splenic injury.
1966 – The term “Kehr’s sign” as related to splenic rupture and left shoulder tip pain appears to have gained traction later. Lowenfels published Kehr’s sign – a neglected aid in rupture of the spleen re-enforcing the eponymous term and proposing the clinical value of the sign in diagnosing splenic injury. Subsequent literature, including Sutton (2002) and Söyüncü (2012), reiterated the sign’s utility.
2004 – A critical commentary by V. Klimpel questioned the legitimacy of Kehr’s attribution, concluding that Kehr never documented the symptom in splenic trauma, suggesting the eponym might be a case of historical misattribution based on his prominence in hepatobiliary surgery
Kehr T-tube (Kehrsche T-Drain) (1912)
The T-tube or “Kehr tube,” is a flexible rubber device, shaped like the letter “T”, which allows controlled external drainage of bile following exploration or surgery on the biliary tract, particularly after choledochotomy (incision of the common bile duct). Its design prevents bile leakage into the peritoneal cavity and facilitates postoperative cholangiography to assess duct patency.
1912 – Kehr outlined his innovative design for a modified biliary drainage system. Kehr developed a T-shaped rubber drain that allowed the external drainage of bile, with a shortened intraductal limb and controlled closure strategy to prevent bile leakage and reduce post-operative complications.
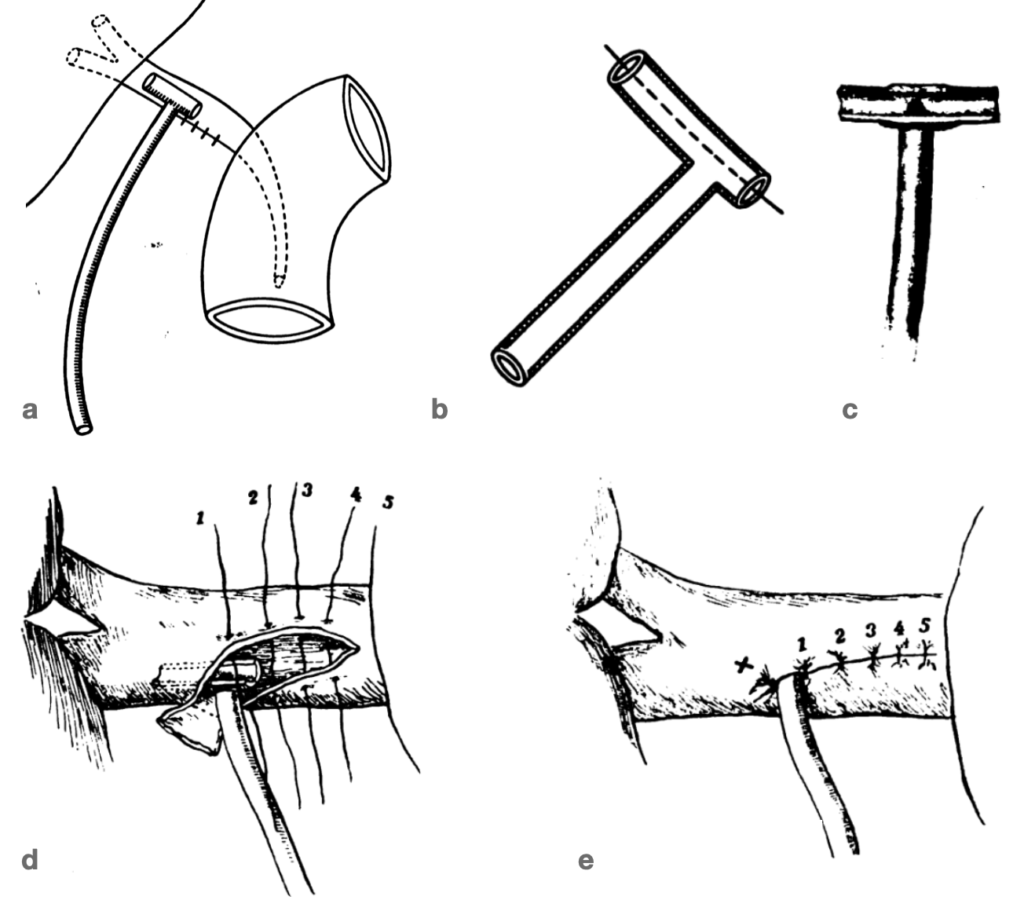
Fig b, c: Illustrate the modified Rinnenrohr (groove tube), with the dorsal wall removed to prevent obstruction and simplify removal.
Fig d, e: Demonstrate full placement technique, including hepatic duct incision, T-tube positioning, suture strategy, and gallbladder stump closure. Kehr H. Zur Verbesserung der Hepatikusdrainage 1912
The best battle against infectious cholelithiasis is the surgeon’s knife.
Aphorism attributed to Hans Kehr
Key Medical Contributions
Courvoisier’s Law (1890)
Courvoisier’s law/sign refers to the clinical observation that a painless, palpable, enlarged gallbladder in the presence of jaundice is more likely caused by malignant obstruction (e.g., carcinoma of the head of pancreas or bile duct) than by gallstones.
1899 – Kehr in Anleitung zur Erlernung der Diagnostik der einzelnen Formen der Gallensteinkrankheit confirms the same clinical pattern:
To the results of palpation. In obstruction of the choledochus by a stone the gall-bladder is usually small and not to be felt ; in obstruction by tumor, usually to be felt as a large and elastic distended tumor under the right ribs.
Kehr 1899
Major Publications
- Kehr H. Die chirurgische Behandlung der Gallensteinkrankheit; ein Rückblick auf 206 Gallenstein-Laparotomieen unter besonderem Hinweis auf die Nothwendigkeit frühzeitiger Operationen. Für praktische Aerzte und Chirurgen. 1896
- Kehr H. Anleitung zur Erlernung der Diagnostik der einzelnen Formen der Gallensteinkrankheit. 1899
- Kehr H. Anleitung zur Erlernung der Diagnostik der einzelnen Formen der Gallensteinkrankheit; auf Grund eigener, bei 433 Gallensteinlaparotomien gewonnener Erfahrungen. 1899 [Translation: Kehr H. Diagnosis of gallstone disease. 1901]
- Kehr H. Introduction to the differential diagnosis of the separate forms of gallstone disease, based upon his own experience gained in 433 laparotomies for gallstones, by Professor Hans Kehr: Authorized translation by William Wotkyns Seymour 1901
- Kehr H. Beiträge zur Bauchchirurgie. 1902
- Kehr H. Die in meiner Klinik geübte Technik der Gallensteinoperationen mit einem Hinweis auf die Indikationen und die Dauererfolge. 1905
- Kehr H. Die interne und chirurgische Behandlung der Gallensteinkrankheit. 1906
- Kehr H. Verletzungen und Chirurgische Erkrankungen der Leber, der Gallenwege und der Milz. In: Handbuch der praktischen Chirurgie 1907; 685-701
- Kehr H. Drei Jahre Gallensteinchirurgie; Bericht über 312 Laparotomien am Gallensystem aus Jahren 1904-1906. 1908
- Kehr H. Zur Verbesserung der Hepatikusdrainage. Zentralblatt für Chirurgie 1912; 39: 1017–1020
- Kehr H. Die Praxis der Gallenwege-Chirurgie in Wort und Bild. 1913
References
Biography
- Erwin P. Hans Kehr. Münchener medizinische Wochenschrift 1916; 63(29): 1046-1047
- Abe HR. Hans Kehr. Beiträge zur Geschichte der Universität Erfurt. 1979: 233-240
- Klimpel V. Der Chirurg Hans Kehr (1862-1916). Medizinhist J. 1991;26(3-4):363-5.
- Morgenstern L. Hans Kehr: not first, but foremost. Surg Endosc. 1993; 7(3): 152‐154.
- Wolff H. Der Chirurg Hans Kehr [Hans Kehr, the surgeon]. Zentralbl Chir. 1998;123 Suppl 2:6-9.
- Schneider B. Prof. Hans Kehr–Sein Leben und sein Werk [Prof. Hans Kehr–his life and his work]. Zentralbl Chir. 1998;123 Suppl 2:10-12.
- Röse W. Ein anästhesiologischer Rückblick auf den Chirurgen Hans Kehr [Anesthesiologic retrospective view of the surgeon Hans Kehr]. Zentralbl Chir. 1998;123 Suppl 2:13-18.
- Berci G, Greene FL. Professor Dr. Hans Kehr (1862–1916). In: No Stones Left Unturned. Springer, Cham. 2021: 7-10
- Bibliography. Kehr, Hans 1862-1916. WorldCat Identities
Eponymous terms
- Levy L. Zur Diagnose der Milzverletzungen. Zentralblatt für Chirurgie 1910; 37(50): 1577-1579
- Saegesser M. Der linksseitige Phrenikusdruckpunkt als diagnostisches Merkmal bei Milzverletzungen [The left-sided phrenic nerve pressure point as a diagnostic feature of spleen injuries]. Zentralblatt für Chirurgie 1938; 65(39): 2179-80.
- Lowenfels AB. Kehr’s sign – a neglected aid in rupture of the spleen. N Engl J Med. 1966; 274(18): 1019.
- Klimpel V. Die Durchsetzung neuer gallenchirurgischer Operationsprinzipien durch Hans Kehr (1862-1916) in der Zeit von 1890 bis 1916. Beitr Hochsch Wissenschaftsgesch Erfurts. 1987; 21: 221‐242
- Klimpel V. Der Fortbildung verpflichtet–Hans Kehr zum 125. Geburtstag [Dedicated to continuing education–Hans Kehr on the 125th anniversary of his birth]. Z Arztl Fortbild (Jena). 1987;81(11):565-7.
- Klimpel V. Das Krankenjournal von Hans Kehr (1862-1916) aus den Jahren 1905 bis 1910 als medizinhistorisches Dokument [The medical journal of Hans Kehr (1862-1916) from 1905 to 1910 as a medical history document]. Sudhoffs Arch. 1992;76(1):117-21.
- Sutton CD, Marshall LJ, White SA, Berry DP, Dennison AR. Kehr’s sign – a rare cause: spontaneous phrenic artery rupture. ANZ J Surg. 2002;72(12):913‐914.
- Klimpel V. Stammt das “Kehrsche Zeichen” von Hans Kehr? Eine quellenkritische Anmerkung [Does Kehr’s sign derive from Hans Kehr? A critical commentary on its documentation?]. Chirurg. 2004;75(1):80‐83.
- Söyüncü S, Bektaş F, Cete Y. Traditional Kehr’s sign: Left shoulder pain related to splenic abscess. Ulus Travma Acil Cerrahi Derg. 2012;18(1):87‐88.
- Rastogi V, Singh D, Tekiner H, Ye F, Mazza JJ, Yale SH. Abdominal Physical Signs of Inspection and Medical Eponyms. Clin Med Res. 2019 Dec;17(3-4):115-126.
- Yale SH, Tekiner H, Yale ES. Origin of Kehr Sign in Traumatic Splenic Trauma. Journal of the College of Physicians and Surgeons Pakistan 2023; 33(03): 360-361
Eponym
the person behind the name
BMBS BMedSci University of Southampton. Working towards a career in Emergency Medicine with interest in Cardiology and Sports Medicine.
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | On Call: Principles and Protocol 4e| Eponyms | Books |

