Kawasaki disease
Description
Kawasaki disease (KD) is an acute self-limited febrile multisystem vasculitis of childhood of unknown aetiology in which coronary artery aneurysms (CAA) may develop in 15% – 25% of untreated cases.
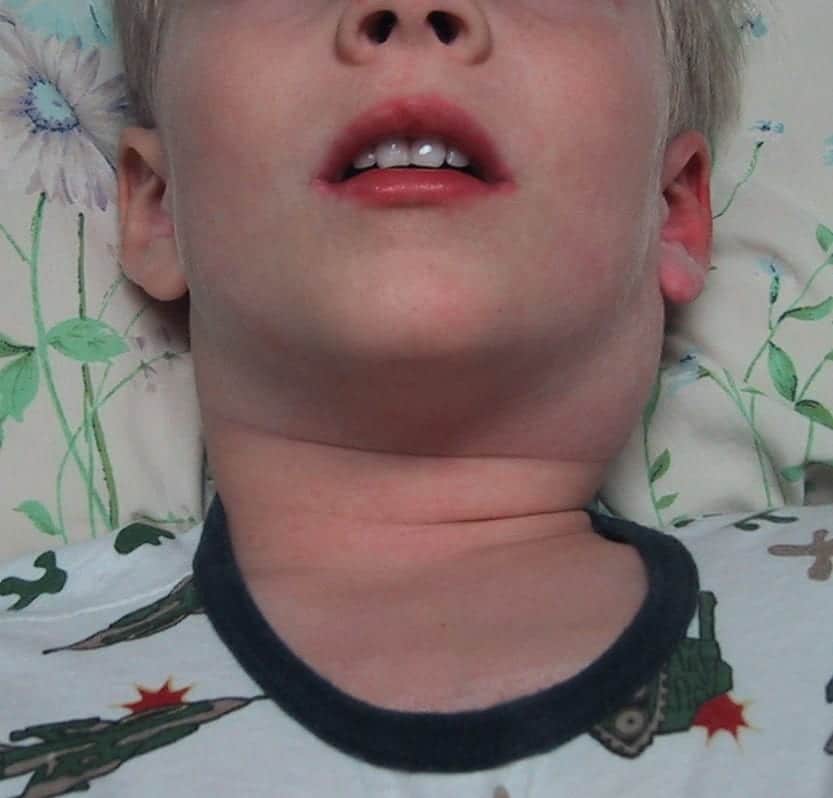
Diagnosis is based on the presence of persistent fever in conjunction with clinical features including polymorphous exanthema; cervical lymphadenopathy; bilateral non-purulent conjunctival injection; buccal mucosae changes (erythema of mucosae, strawberry tongue, cracked lips); and changes in extremities (acute phase: swelling and redness of the palms, subacute phase: desquamation).
Incidence varies markedly between ethnic groups and countries. Epidemiological data from European studies (2016) suggest an incidence of KD of 5-10/100,000 children <5 years; but increased incidence in Asian countries such as Japan with 265/100,000 children <5 years (2012)
Aetiology remains unknown. Current consensus that it results from an infectious trigger initiating an abnormal immune response in genetically predisposed children.
Treatment consists of high dose intravenous immunoglobulin (IVIG) and is directed at preventing the development of CAA.,

Since the first survey in 1970, there have been 200,000 reported cases in Japan. Three times there have been epidemics. Kawasaki disease appears in all races and on all continents. Although more than 6,000 research papers have been written about it, the cause remains unknown.
Kawasaki 2007
History
1961 – January 5, Tomisaku Kawasaki examined a 4 year-3 month old boy, with curious clinical symptom-complex.
The patient showed high fever of about two weeks duration, bilateral conjunctival hyperemia without discharge, reddening dry fissured lips, diffuse redness of the mucous membrane of oral cavity, strawberry-like tongue, left nonpurulent cervical adenopathy, polymorphous erythema on the body and marked redness of palms and soles with indurative edema of hands and feet following desquamation from the fingertips.
When I presented this case at a clinical conference, it was suggested as atypical scarlet fever or mild-type Stevens-Johnson syndrome. But I did not agree with any of the opinions suggested. Finally the case was declared “Diagnosis Unknown.” I always wondered what the diagnosis might be.
Kawasaki 2006
1962 – Kawasaki presented 7 cases to the Chiba Regional Pediatric Meeting under the title, “Non scarlatiniform Syndrome with Desquamation from the Fingertips”. However there was no further discussion.
1967 – Kawasaki presented 50 paediatric cases he had observed over a 6 year period with characteristic differences to syndromes grouped together at that time involving skin, mucous membranes and eyes.
…I have observed 50 cases similar to so-called mucocutaneous-ocular syndrome (MCOS) but different in various points, during approximately 6 years from January 1961 to November 1966…after more precise examination of the conventional reports about MCOS, I realized that our syndrome is a unique clinical entity, which is not identical with any type of MCOS ever reported. Therefore I present the clinical analysis and laboratory data of 50 cases we experienced as well as a review of the literature, and I hope to hear your opinion.
Kawasaki 1967
1973 – Initial publications included variable use of the terms Kawasaki fever; Kawasaki’s syndrome; and Kawasaki’s disease in conjunction with Mucocutaneous Lymph Node Syndrome (MCLS).
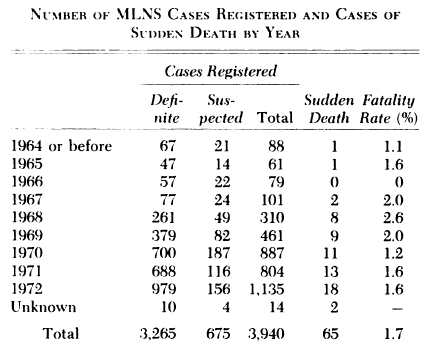
1974 – Kawasaki publishes a comprehensive review of the clinical features of the febrile mucocutaneous lymph node syndrome (MLNS). Epidemiologic review confirmed the disease was widely disseminated throughout Japan with more than 6,000 cases had been reported by the end of 1973. Kawasaki noted a low but persistent fatality rate secondary to cardiac failure.
One to two percent of the patients died suddenly of cardiac failure. All 13 autopsies showed infantile periarteritis nodosa-like arteritis accompanied by coronary thrombosis and aneurysm. Some of the surviving patients also had similar changes associated with the heart. All these facts lead us to believe that the clinical features of the disorder constitute a new clinical entity.
Kawasaki 1974
1979 – Worldwide recognition of Kawasaki disease when the 11th edition of the tome ‘Nelson: Textbook of Pediatrics’ [673-674] added the eponymous term to a new section on Mucocutaneous Lymph Node Syndrome (MLNS)
2002 – Original article translated into English by Shike, Shimizu and Burns [Pediatr Infect Dis J, 2002; 21: 1-38] and is well worth the read…
It is truly a masterpiece of descriptive clinical writing from the past century.1 In his exhaustive detailing of every observable aspect of the disease, Kawasaki was part Sherlock Holmes and part Charles Dickens with his sense of mystery and his vivid descriptions of the clinical features of these patients.
Burns 2002
2004 – Definition as per the American Heart Association
Kawasaki disease is an acute self-limited vasculitis of childhood that is characterized by fever, bilateral nonexudative conjunctivitis, erythema of the lips and oral mucosa, changes in the extremities, rash, and cervical lymphadenopathy. Coronary artery aneurysms or ectasia develop in approximately 15% to 25% of untreated children and may lead to ischemic heart disease or sudden death.
Newburger et al 2004, American Heart Association
2020 – Over the course of the SARS-CoV-2 pandemic small numbers of children across multiple countries have been noted to develop a multisystem inflammatory syndrome in response to the novel coronavirus. This rare syndrome shares common features with other paediatric inflammatory conditions including: Kawasaki disease, staphylococcal and streptococcal toxic shock syndromes, bacterial sepsis and macrophage activation syndromes. It can also present with unusual abdominal symptoms with excessive inflammatory markers.
Report from Bergamo the Italian epicentre of the SARS-CoV-2 pandemic:
…witnessed a 30-fold increased incidence of Kawasaki-like disease. Children diagnosed after the SARS-CoV-2 pandemic began showed evidence of immune response to the virus, were older, had a higher rate of cardiac involvement, and features of MAS. The SARS-CoV-2 pandemic was associated with high incidence of a severe form of Kawasaki disease
Verdoni 2020
The Royal College of Pediatrics and Child Health UK have published guidance on this Paediatric multisystem inflammatory syndrome temporally associated with COVID-19 and numerous studies have been instigated. Two COVID-19 priority studies in the UK (DIAMONDS [Central Portfolio Management System 45537] and ISARIC [UK Clinical Research Network 14152]) are collaborating to ensure that every child with this emerging syndrome has the opportunity to consent to take part in a study exploring mechanisms.
Associated Persons
- Tomisaku Kawasaki 川崎 富作 (1925 – )
Alternative names
- Kawasaki’s disease; KD; Kawasaki’s syndrome
- Mucocutaneous-ocular syndrome
- Acute Febrile Mucocutaneous Lymph Node Syndrome (MNLS).
References
Original articles
- Kawasaki T. [Acute febrile mucocutaneous syndrome with lymphoid involvement with specific desquamation of the fingers and toes in children]. Arerugi. 1967 Mar;16(3):178-222. [Original publication]
- Kawasaki T, Kosaki F, Okawa S, Shigematsu I, Yanagawa H. A new infantile acute febrile mucocutaneous lymph node syndrome (MLNS) prevailing in Japan. Pediatrics. 1974 Sep;54(3):271-6. [First English publication]
- Kawasaki T. Kawasaki disease. Proc Jpn Acad Ser B Phys Biol Sci. 2006;82(2):59‐71.
Review articles
- Kawasaki Disease. Nelson: Textbook of Pediatrics. (11th edition) 1979: 673-674
- Burns JC, Kushner HI, Bastian JF, et al. Kawasaki disease: A brief history. Pediatrics. 2000;106(2):E27.
- Burns JC. Commentary: translation of Dr. Tomisaku Kawasaki’s original report of fifty patients in 1967. Pediatr Infect Dis J. 2002; 21(11): 993-995.
- Newburger JW, Takahashi M, Gerber MA, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association [published correction appears in Pediatrics. 2005 Apr;115(4):1118]. Pediatrics. 2004;114(6):1708‐1733.
- Singh S, Jindal AK. Fifty Years of Kawasaki Disease – A Tribute to Dr Tomisaku Kawasaki. Indian Pediatr. 2017; 54(12): 1037-1039.
- Dietz SM, van Stijn D, Burgner D, et al. Dissecting Kawasaki disease: a state-of-the-art review. Eur J Pediatr. 2017;176(8):995‐1009.
- Viner RM, Whittaker E. Kawasaki-like disease: emerging complication during the COVID-19 pandemic. Lancet. 2020; 10.1016 /S0140-6736(20)31129-6
- Verdoni L, Mazza A, Gervasoni A, et al. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet. 2020
- Guidance: Paediatric multisystem inflammatory syndrome temporally associated with COVID-19. RCPCH May 2020
- Nickson C. Needing a Diagnostic Kick-start. LITFL
[cite]
eponymictionary
the names behind the name