Needing a Diagnostic Kick-start
aka Paediatric Perplexity 008
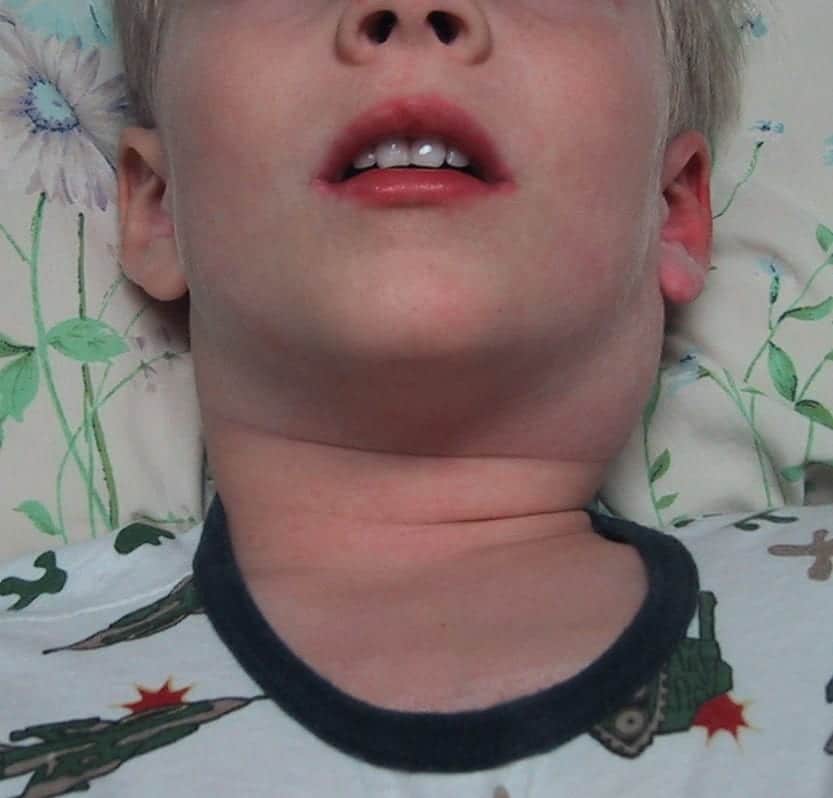
A 4 year-old boy has been brought to the emergency department by his worried parents. He has had fevers for the past 6 days. They are concerned because he is not getting better despite repeated visits to a number of doctors. Each time they were told he had a viral illness.
On examination you note the presence of bilateral conjunctivitis, and erythematous rash on his torso and limbs, a 4 cm tender left-sided cervical lymph node and a diffusely red pharynx.
Q1. What is the likely diagnosis?
Answer and Interpretation
Kawasaki disease
Also known as Mucocutaneous Lymph Node Syndrome (MNLS), this vasculitic disorder was first described by Dr. Tomisaku Kawaski in 1967. It is of uncertain etiology, but may be a post-infectious condition.
Q2. How is this diagnosis made?
Answer and Interpretation
The diagnosis is made on the basis of the following clinical criteria (A + B):
A.Fever ≥5 days
B. At least 4 of the 5 following physical examination findings:
1. Bilateral, nonexudative bulbar conjunctival injection. Bilateral scleral injection with perilimbic sparing
2. Oropharyngeal mucous membrane changes. Pharyngeal erythema, red/cracked lips, and a strawberry tongue
3. Cervical lymphadenopathy. With at least one node >1.5 cm in diameter.
4. Peripheral extremity changes
The
diffuse palmar erythema seen in KD is in contrast to the discrete
macular lesions of various viral illnesses (e.g., measles) that can
sometimes be seen on the palms and soles.
– acute phase: diffuse erythema and swelling of the hands and feet.
– convalescent phase: periungual desquamation (weeks 2 to 3)
5. A polymorphous generalized rash. Nonvesicular and nonbullous. There is no specific rash that is pathognomonic for KD
The manifestations may appear sequentially rather than concurrently. Atypical cases may not meet all the criteria but may still have the same risks of cardiac complications. These ‘incomplete’ cases occur more often in infants less than 6 months-old — further investigations (see Q5) should be performed if fever of 5 days and 2 or 3 of the other criteria are present.
Clinicians should have a high index of suspicion for this diagnosis in any child with a prolonged fever as early diagnosis and treatment may help prevent the potentially fatal complications of Kawasaki disease.
The approach to ‘incomplete’ Kawasaki disease is summarised nicely in this Paucis Verbis card from Academic Life in Emergency Medicine: Kawasaki disease.
Q3. Who gets this condition?
Answer and Interpretation
Kawasaki disease may occur in any child of any age, and even adults in some cases.
However, it is more common in:
- children aged < 5 years
- Asians
- males (RR 1.5)
Q4. What are the important differential diagnoses?
Answer and Interpretation
Diagnosis may be difficult as Kawasaki disease may mimic a number of other conditions:
- Viral exanthemas including measles
- Streptococcal disease (e.g. scarlet fever, toxic shock syndrome)
- Staphylococcal disease (e.g. scalded skin syndrome, toxic shock syndrome)
- Bilateral cervical lymphadenitis
- Leptospirosis and rickettsial diseases
- Stevens-Johnson syndrome and Toxic Epidermal Necrolysis
- Drug reactions including mercury hypersensitivty reaction
- Juvenile Chronic Arthritis
Q5. What investigations should be performed?
Answer and Interpretation
Echocardiography
The most important investigation to assess for cardiac complications. If no abnormalities on presentation the study should be repeated in 4-6 weeks.
Laboratory tests:
- Rule out other causes:
- ASOT, AntiDNAse B, throat swabs, blood cultures
- Non-specific findings seen in KD include:
- FBC: normochromic anemia and leukocytosis; thrombocytosis (in the 2nd week)
- LFT changes and hypoalbuminemia
- increased CRP and ESR
- Sterile pyuria of ≥10 WBCs per high-power field
The approach to ‘incomplete’ Kawasaki disease is summarised nicely in this Paucis Verbis card from Academic Life in Emergency Medicine: Kawasaki disease.
Q6. What complications may occur?
Answer and Interpretation
Cardiac complications:
- Carditis during the febrile phase
- myocarditis with ST-T changes (25%), pericardial effusions (20-40%), valvular dysfunction (1-2%) and cardiac failure (~5%)
- Coronary vessel abnormalities (occur in 20% of cases if untreated and <5% if treated; peaks at 2-4 weeks)
- aneurysm formation may lead to fatalities from thrombosis, rupture or ischemia-related dysrhythmia (usually within 6 weeks of onset, but may occur many years later.
Kawasaki disease is a vasculitis that can potentially affect almost any organ, it is commonly associated with:
- arthritis
- keratitis and uveitis
- diarrhoea, vomiting and gallbladder disease
- coryza and cough
Q8. What specific treatment is required?
Answer and Interpretation
IV immunoglobulin and aspirin
IV immunoglobulin
- 2g/kg IV over 10 hours
- ideally start within 10 days of the onset of the illness
- a second dose may be given if fevers persist
Aspirin
- 3-5 mg/kg PO daily for 6-8 weeks (when laboratory parameters have fully normalised)
- some advise higher doses of aspirin until the patient is afebrile or 48-72 hours, but others argue this offers no benefit in addition to treatment with IV immunoglobulin.
Despite these therapies 2-4% of cases still go on to develop coronary artery abnormalities. Corticosteroids may be considered in refractory cases, although there is little evidence supporting their use.
References
- Tomisaku Kawasaki 川崎 富作 (1925 – )
- Kawasaki disease. LITFL
- Royal Children’s Hospital Melbourne. RCH Clinical Practice Guidelines — Kawasaki disease
- Paucis Verbis: Kawasaki Disease – Academic Life in Emergency Medicine
- Burns JC. Commentary: translation of Dr. Tomisaku Kawasaki’s original report of fifty patients in 1967. Pediatr Infect Dis J. 2002; 21(11): 993-995.
- Freeman AF, Shulman ST. Kawasaki disease: summary of the American Heart Association guidelines. Am Fam Physician. 2006 Oct 1;74(7):1141-8.
- Kim DS. Kawasaki disease. Yonsei Med J. 2006 Dec 31;47(6):759-72.
- Dietz SM, van Stijn D, Burgner D, et al. Dissecting Kawasaki disease: a state-of-the-art review. Eur J Pediatr. 2017;176(8):995‐1009.
- Verdoni L, Mazza A, Gervasoni A, et al. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet. 2020; 10.1016 /S0140-6736(20)31103-X.
- Guidance: Paediatric multisystem inflammatory syndrome temporally associated with COVID-19. RCPCH May 2020

CLINICAL CASES
Paediatric Perplexity
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC