Ludwig Courvoisier
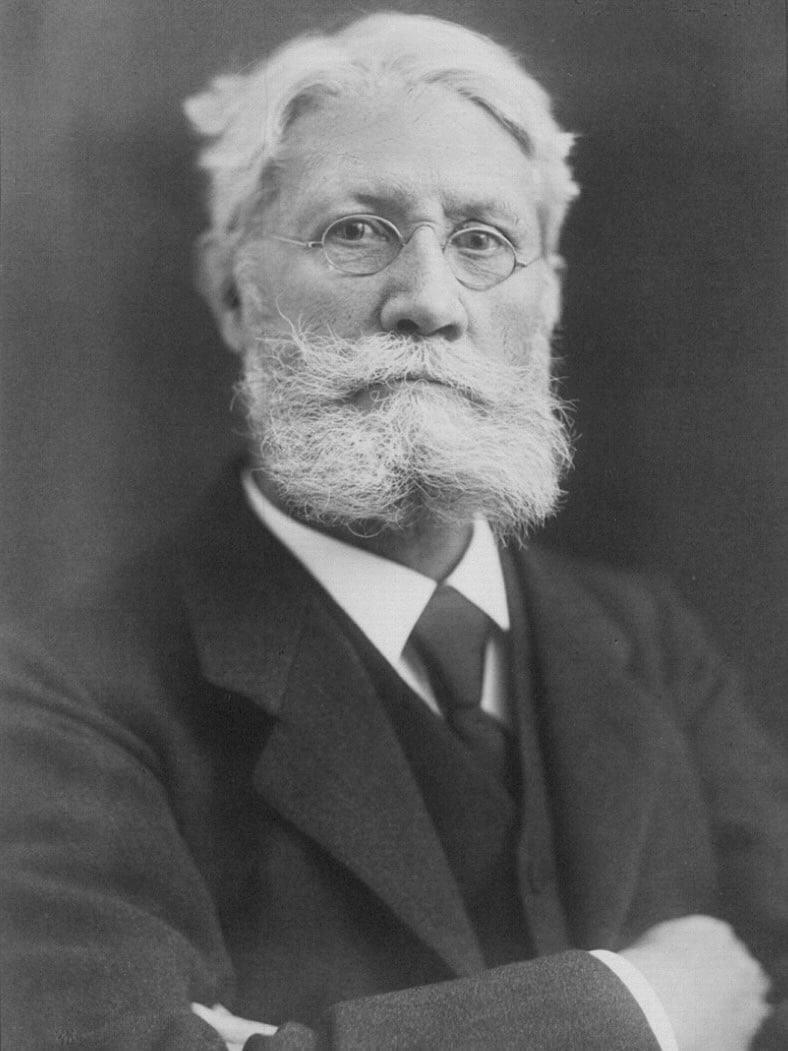
Ludwig Georg Courvoisier (1843-1918) was a Swiss surgeon.
Courvoisier was a surgeon, academic, and naturalist best remembered for Courvoisier’s sign, an important clinical indicator in biliary obstruction. He was educated at the University of Basel completing his medical degree with a dissertation on the spinal ganglia. Postgraduate training in London and Vienna brought him into contact with leading surgeons of the time, including William Ferguson, Spencer Wells, Theodor Billroth, and Vincenz Czerny.
In 1871, Courvoisier was appointed head surgeon at the Diakonissenspital in Riehen, where he remained in active practice for nearly five decades. A gifted clinician and precise observer, he published widely across surgical disciplines. His 1890 monograph Casuistisch-statistische Beiträge zur Pathologie und Chirurgie der Gallenwege introduced the observation that a painless, enlarged gallbladder in the presence of jaundice is unlikely to be caused by gallstones. He also described early gastric bypass surgery, wrote on neuromas, and pioneered antiseptic practices in Basel, building on the work of his mentor August Socin.
Courvoisier was involved in both civic and scientific life in Basel. He served as professor of surgery at the University of Basel, president of the Swiss Federal Medical Examination Commission, and was a member of several natural science societies. In later life, he focussed on his love of natural history, publishing scholarly papers on butterflies.
Biographical Timeline
- Born November 10, 1843 in Basel, Switzerland, the eldest of nine children to Georg Courvoisier and Mary née Louwndes, from Wales.
- 1860s – Studied medicine at the University of Basel and the University of Göttingen. Influenced by teachers including Schönbein, Wiedemann, His, and Rütimeyer.
- 1865 – University of Basel gekrönten Preisschrift for Beobachtungen über den sympathischen Gränzstrang
- 1866–1868 – Assistant to August Socin (1837–1899) and Karl Wilhelm Bischoff in Basel’s surgical clinic. Graduated MD summa cum laude from the University of Basel; dissertation Ueber die Zellen der Spinalganglien.
- 1869–1870 – Postgraduate studies in London (with Sir William Ferguson and Sir Spencer Wells), then Vienna (with Theodor Billroth and Vincenz Czerny).
- 1870–1871 – Served under Socin as an operations assistant during the Franco-Prussian War at the military hospital in Karlsruhe.
- 1871 – Appointed physician and later head surgeon at the Diakonissenspital in Riehen; served there for 47 years until his death.
- 1874 – Published Die häusliche Krankenpflege, a guide to home nursing, which saw at least four editions.
- 1880 – Gained habilitation with a lecture on Felix Würtz, a 16th century Basel surgeon.
- 1883 – Published account of Gastro-Enterostomie nach Wölfler.
- 1886 – Published Die Neurome, a monograph on neuromas.
- 1888 – Appointed professor extraordinary (außerordentlicher Professor) of surgery at the University of Basel.
- 1890 – Published Casuistisch-statistische Beiträge zur Pathologie und Chirurgie der Gallenwege, the basis of Courvoisier’s sign.
- 1899 – Appointed professor ordinary (ordentlicher Professor) of surgery at the University of Basel.
- 1900–1912 – Continued academic and surgical work while serving as president of the Swiss Federal Medical Examination Commission and holding civic roles in Basel.
- 1907–1917 – Published several entomological papers, particularly on Lycaenid butterflies.
- Died April 8, 1918 in Basel from pneumonia at age 74.
Medical Eponyms
Courvoisier Sign (1890)
Courvoisier’s sign or law refers to the clinical finding of a palpable, non-tender, distended gallbladder in the presence of painless obstructive jaundice. It suggests a non-calculous (usually malignant) cause of biliary obstruction, typically pancreatic head carcinoma, cholangiocarcinoma, or ampullary carcinoma, as opposed to gallstone disease.
1890 – Courvoisier’s landmark monograph ‘Casuistisch-statistiche Beiträge zur Pathologie und Chirurgie der Gallenwege‘ synthesized over 400 cases of gallstone surgery. It marked a turning point in the understanding of biliary pathology. In this extensive case-based and statistical review, he emphasised the pathophysiological consequences of chronic cholelithiasis, including the development of cholecystoenteric fistulae and gallstone ileus.
Courvoisier catalogued multiple presentations of gallstone obstruction, distinguishing between acute and chronic forms, and laid out early arguments for surgical intervention. He described 187 cases of common bile duct obstruction, making the observation that gallbladder dilatation seldom occurred with stone obstruction of the bile duct.
Theile ich sämmtliche für diese Untersuchung verwendbaren 187 Fälle in 2 Hauptgruppen, so erhalte ich 87 Steinobstructionen, 100 andre Obstructionen. Wegen ihrer annähernd gleichen numerischen Stärke lassen sich beide gut vergleichen! Nun collidiren mit den Steinobstructionen weitaus am haüfigsten die Gallenblasenatrophien (70:87 Fällen = 80,4%), viel seltener die Ectasien (17:87 = 19,6%). Die andern Verschlüsse dagegen treffen viel seltener mit Atrophie (8:100), viel haüfiger mit Ectasie (92:100) zusammen. Oder anders ausgedrückt: Bei Steinobstruction des Choledochus ist Ectasie der Gallenblase selten; das Organ ist vorher schon gewöhnlich geschrumpft. Bei Obstruction andrer Art ist dagegen Ectasie das Gewöhnliche; Atrophie besteht nur in 1/12 dieser Fälle
In a collection of 187 cases, two main groups were usable for this investigation: 87 stone obstructions and 100 other obstructions. Because of their approximately same numerical strength, they can be compared well. Gallbladder atrophy with stone obstruction (70:87 cases = 80.4%) was more common than the rare ectasia (17:87 = 19.6%). With other causes of obstruction to the choledochus, it is rarer to see atrophy (8:100) than ectasia (92:100). Or differently expressed, with stone obstruction of the choledochus, ectasia of the gallbladder is rare; usually, the organ has already shrunk. Ectasia is usual with obstruction of other kinds; atrophy exists in only 1 of 12 of these cases
Although often described as a ‘law’ and related to malignancy, Courvoisier fell short of making such a definitive statement. It is unclear when this observation became a ‘law’ in the literature. He stated that in cases of a palpable gallbladder in the presence of an obstructed bile duct, that stone obstruction is less likely and that ‘‘other causes’’ (without specifying diagnoses) are more likely.
Dieses Ergebnis der Untersuchung ist mir überraschend genug gewesen. Gewöhnlich wird in den Hand- und Lehrbüchern angegeben, Steinobstruction des Choledochus führe durch Gallenstauung zu Gallenblasenerweiterung. Ich finde das gerade Gegentheil und muss das Fehlen einer Ectasie bei Verlegung des Gangs geradezu als charakteristisch für Stein, ihr Vorhandensein als bezeichnend für sonstige Occlusion betrachten. Wenn sich das noch weiter bestätigen
sollte, so wäre damit ein wichtiger Anhaltspunkt für die differentielle Diagnostik gewonnen!
It is usually stated in the manuals and textbooks that stone obstruction of the choledochus leads to enlargement of the gallbladder by biliary obstruction. I do not find this to be true, and must consider the absence of dilation of the gallbladder due to a gallstone and the presence of gallbladder dilation due to other causes of obstruction. If this were to be confirmed further, this would be an important point of reference for the differential diagnostics!
The presence of a distended, palpable, non-tender gallbladder in a jaundiced patient is 83 – 90% specific with a sensitivity of only 26 – 55% for malignant obstruction of the bile duct. The sign has been described in a number of conditions including chronic pancreatitis; cholelithiasis; choledocholithiasis; Hartmann’s pouch obstruction; chronic autoimmune pancreatitis; congenital choledochal cysts; and parasitic obstruction of the biliary system.
Uebrigens ist die Erklärung für diesen Unterschied nicht schwierig. Laut früherer Darstellung (p. 47) stammen die Choledochussteine in der Regel aus der Gallenblase. Auf ihrem Weg aber haben sie, wie eben dort gezeigt worden ist, den Cysticus und zum Theil die Blase gereizt und in beiden deutliche Spuren eines erzwungenen Durchtritts in Form einer chronischen Entzündung der Wandung hinterlassen, welche häufig zuletzt zur Schrumpfung jener Behälter führt. Ist nun die Gallenblase so verändert, so wird auch die stärkste Gallenstauung sie nicht mehr ausdehnen können. Bei den meisten andern Obstructionen, speciell bei denjenigen durch drückende Geschwülste, findet die andringende Galle eine normale, nachgiebige Blase vor!
According to the earlier account (p. 47), the stones in the common bile duct originate from the gallbladder. On their way, however, as they have been shown, the stones as they pass irritate the cystic duct as well as the gallbladder and this irritation causes chronic inflammation of the gallbladder wall, which often leads to a shrinking of the duct and gallbladder. If the gallbladder is altered, the strongest biliary stasis will no longer be able to expand it. In most other cases of obstruction, especially those due to tumor, bile flow shows a normal compliant gallbladder!
1901 – Richard Clarke Cabot (1868-1939) formally introduced the term “Courvoisier’s Law” after analyzing data from Courvoisier, Kehr, Mayo Robson, Naunyn, and 86 cases from Massachusetts General Hospital (finding only 4 exceptions). He affirmed its diagnostic value in distinguishing malignant from calculous bile duct obstruction, highlighting its relevance in cases of painless jaundice with a palpable gallbladder.
This rule of Courvoisier’s has often been stated before, but I do not find it elsewhere named as his law. It seems to me a real help in diagnosis, and I venture to name it thus
Cabot, 1901
Major Publications
- Courvoisier LG. Beobachtungen über den sympathischen Gränzstrang. 1866
- Courvoisier LG. Ueber die Zellen der Spinalganglien, sowie des Sympathicus beim Frosch. Archiv f. mikrosk. Anatomie 1868; 4, 125–145
- Courvoisier LG. Die häusliche Krankenpflege. 1874
- Courvoisier LG. Gastro-Enterostomie nach Wölfler bei inoperablem Pylorus Carcinom, Tod. Centralblatt für Chirurgie. 1883; 10: 794-797
- Courvoisier LG. Die Neurome: eine klinische Monographie, 1886
- Courvoisier LG. Casuistisch-statistiche Beiträge zur Pathologie und Chirurgie der Gallenwege. 1890
- Courvoisier LG. Ueber Zeichnungs-Aberrationen bei Lycaeniden. Zeitschrift für wissenschaftliche Insektenbiologie 1907; 3: 73-78
- Courvoisier LG. Entdeckungsreisen und kritische Spaziergänge ins Gebiet der Lycaeniden. Entomologische Zeitschrift 1910; 24: 88-89
- Courvoisier LG. Uebersicht über die um Basel gefundenen Lycaeniden. Verhandlungen der Naturforschenden Gesellschaft in Basel. 1910; 21: 153–164
- Courvoisier LG. Zur Synonymie des Genus Lycaena. Deutsche entomologische Zeitschrift “Iris”, 1914; 28: 143-229
References
Biography
- Lotz A. Zum Gedächtnis an Professor Dr. Ludwig Courvoisier, 1843–1918. Basel 1918.
- Prof. Dr. med. L. G. Courvoisier. Correspondenz-Blatt für Schweizer Aerzte, 1918; 48: 1314-1319. [PDF]
- Veillon E. Prof. Dr. med. L. G. Courvoisier. Basler Jahrbuch 1920: 1–13.
- Ludwig Georg Courvoisier. Gemeinde Lexikon Riehen
- Fresquet JL. Ludwig Courvoisier (1843-1918). Historia de la Medicina
Eponymous terms
- Shepper E. Ludwig Georg Courvoisier (1843–1918) and his Position in the History of Gall Bladder Surgery. Hochschulschrift. Basel 1960.
- Chung RS. Pathogenesis of the “Courvoisier gallbladder”. Dig Dis Sci. 1983 Jan;28(1):33-8.
- Bromley PJ, Keller FS. Images in clinical medicine. Courvoisier’s gallbladder. N Engl J Med. 2001 Nov 22;345(21):1542.
- Parmar MS. Courvoisier’s law. CMAJ. 2003 Apr 1;168(7):876-7.
- Fitzgerald JE, White MJ, Lobo DN. Courvoisier’s gallbladder: law or sign? World J Surg. 2009 Apr;33(4):886-91.
- Murphy K, McLaughlin P, O’Connor BR, Breen M, O’Súilleabháin C, Maceneaney P, Maher MM. Does Courvoisier’s sign stand the test of time? Clin Radiol. 2012 Nov;67(11):e27-30.
- Rastogi V, Singh D, Tekiner H, Ye F, Kirchenko N, Mazza JJ, Yale SH. Abdominal Physical Signs and Medical Eponyms: Physical Examination of Palpation Part 1, 1876–1907. Clinical Medicine & Research. 2018 Dec 1;16(3-4):83-91.
- Giambelluca D, Dimarco M, Salvaggio G, Madiri M. The Courvoisier’s sign. Abdom Radiol 2019; 44: 1185–1186
Eponym
the person behind the name
MbChB University of Bristol, UK. Currently working at Sir Charles Gairdner Hospital, Perth, Australia in emergency medicine.
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | On Call: Principles and Protocol 4e| Eponyms | Books |

