Lung Ultrasound: Comprehensive Examination
Comprehensive lung ultrasound examination involves the following steps:
- Thorough clinical assessment with integration of history, clinical findings and other investigations. This enables formulation of a differential diagnosis and allows more accurate interpretation of the ultrasound findings.
- Ultrasound examination of all accessible pleural surfaces and the adjacent lung.
- Echocardiography adds enormously but requires additional expertise.
- Where pulmonary embolism is considered sonographic examination of the deep veins may be useful.
Technique for Complete Lung Ultrasound
Where time allows and a complete ultrasound examination is required the clinician must examine the anterior, lateral, posterior and inferior pleural surfaces. This is most readily done in a patient who can sit up and assist with inspiratory and expiratory effort as required.
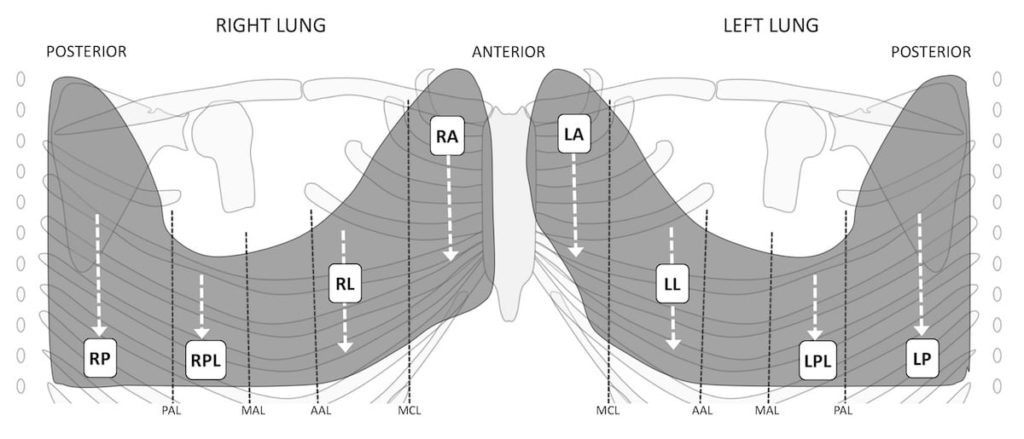
Follow each of the dotted white lines on the above schematic, with the ultrasound probe initially with the oriented longitudinally across the ribs, and then transversely or obliquely – so the ultrasound beam aligns with the intercostal space and avoids the ribs. Assess for lung sliding, and define and explore the costophrenic angles. Probe longitudinal.
- Place the transducer in the longitudinal plane where lung sliding is most clearly demonstrated. Hold the probe still and watch for sliding, then move toward the diaphragm. The clinician begins anteriorly starting cranially and moves the transducer caudally in the mid clavicular line until the costophrenic angle is seen. This is repeated laterally and posteriorly.
- Fluid collects in the costophrenic angle and if a chest drain is to be inserted being certain where the thoracic cavity ends is essential.
Examine the pleural surface and underlying lung over the entire thorax. Probe oblique.
- The transducer is positioned to lie along the intercostal space between the ribs (6-11). Holding the probe still in any intercostal space, whilst a patient breathes in will bring lung from above into view, and then in expiration, the lung from below into view. Sequentially moving down one rib space at a time will ensure the entire accessible lung is interrogated.
- Begin anteriorly cranially and progress down to the diaphragm, and repeat moving laterally and then posteriorly, as if “mowing the lawn” with the transducer.
- In each view chest wall, pleural surface, and any deeper pathology is carefully assessed and described.
- The undersurface of the right lung can be explored by using the liver as an acoustic window. With the probe in longitudinal, transverse or oblique, angle upward from below the diaphragm, to see the dome of diaphragm with lung above it.
- This is a little more difficult on the left but the spleen can act as a similar window by angling upward through an interspace at the left posterior axillary line.
Describe any abnormality found ideally on a standardised report form.
- Describe its location and extent.
- Describe what structures are involved – chest wall, pleura, lung…
- Describe the appearance using ultrasound terminology, and where appropriate make a clinical conclusion.
Examples:
Example 1: There is loss of lung sliding on the right anteriorly with an increase in A-lines. A lung point is seen at the right anterior axillary line. This is consistent with a small pneumothorax.
Example 2: There is a moderate left basal pleural effusion extending from diaphragm up to the midzone posteriorly and laterally. The maximal depth from chest wall to underlying lung is 3cm at the posterior base. The effusion is anechoic and there is a small area of associated basal atelectasis.
Example 3: There is a single area of consolidation at the right anterior and lateral lower chest. As well as sonographic hepatization, air bronchograms and shred sign are evident. There is no associated pleural effusion. The clinical and sonographic picture support the diagnosis of pneumonia.
Continue to echocardiographic examination as indicated.
Related Clinical Cases
- LITFL Ultrasound library
- LITFL Top 100 ultrasound cases
- LUNG ultrasound WORKED CASES
- LUNG ultrasound MODULES
ULTRASOUND LIBRARY
POCUS
An Emergency physician based in Perth, Western Australia. Professionally my passion lies in integrating advanced diagnostic and procedural ultrasound into clinical assessment and management of the undifferentiated patient. Sharing hard fought knowledge with innovative educational techniques to ensure knowledge translation and dissemination is my goal. Family, wild coastlines, native forests, and tinkering in the shed fills the rest of my contented time. | SonoCPD | Ultrasound library | Top 100 | @thesonocave |

